CASE REPORT
Combining Skeletal Anchorage and Intermaxillary Elastics in Class II Treatment
Appliances designed for Class II correction generate either pulling, interarch force vectors (intermaxillary elastics) or pushing, interarch force vectors (bite-jumping devices).1 Intermaxillary elastics, which have the capacity to produce both sagittal and extrusive forces at the point of attachment, are the most popular mechanism for correction of sagittal problems.1-3 Class II elastics should be used judiciously, however, because of their association with such adverse effects as mandibular anchorage loss, lower molar extrusion, clockwise rotation of the occlusal plane, lower incisor proclination, and upper incisor extrusion.4-6 Some authors assert that treatment results are less satisfactory in terms of skeletal relationships and facial esthetics when Class II elastics are used. The esthetic compromise results from extrusion of the lower molars and upper incisors and consequent clockwise rotation of the occlusal plane.5-7 Upper incisor extrusion also increases gingival exposure and thus impairs smile esthetics.
At least in the short term, bite-jumping devices achieve greater skeletal changes than Class II elastics because they are fixed and therefore less dependent on patient compliance.6,8-14 To overcome this advantage while improving the predictability of outcomes, orthodontists have begun to combine Class II elastics with skeletal anchorage from temporary anchorage devices (TADs). Besides avoiding the loss of anchorage associated with toothborne appliances and auxiliaries, TADs have the advantages of low cost and easy insertion.15,16 The following case report demonstrates this innovative integration of treatment mechanics in the correction of Class II malocclusion.
Similar articles from the archive:
- CASE REPORT Class II Correction in an Adult High-Angle Patient Using Low-Friction Mechanics and Skeletal Anchorage July 2017
- CASE REPORT Targeted Mechanics for Limited Posterior Treatment with Mini-Implant Anchorage December 2015
- CASE REPORT Mini-Implant Anchorage in a Unilateral Class II Patient May 2012
Diagnosis and Treatment Plan
A 12-year-old female was referred by her dentist for orthodontic correction of protrusive maxillary teeth. Clinical examination showed bilateral Class II molar and canine relationships, with a 1mm discrepancy between the upper and lower dental midlines, a convex profile, and incompetent lips (Fig. 1).
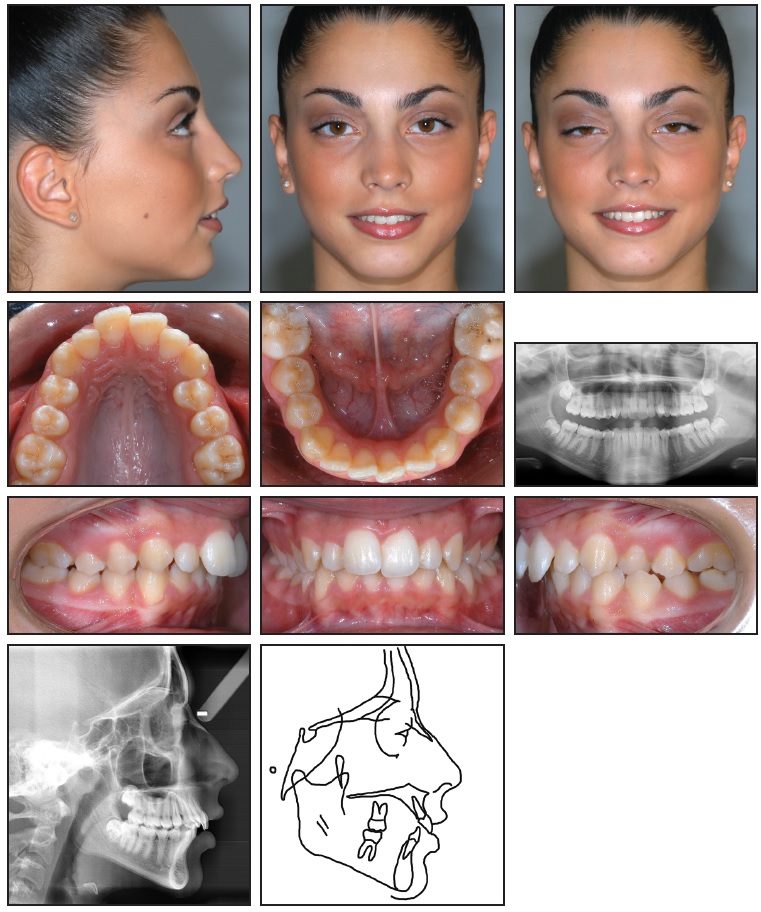
Fig. 1 12-year-old female patient with convex profile; retrusive mandible; anterior crowding; and Class II, division 1 malocclusion before treatment.
The patient exhibited a crossbite between the upper and lower left first premolars. The maxillary arch was constricted, with anterior crowding; the mandibular arch also had mild anterior crowding.
The panoramic radiograph showed the presence of all permanent teeth. Cephalometric analysis indicated a skeletal Class II malocclusion (Table 1).
Treatment goals were to improve facial esthetics while achieving Class I molar and canine positions. Additional objectives were to widen the maxillary arch and correct the dental midlines without negatively affecting facial esthetics.
An accomplished dancer, the patient requested treatment that would require minimal compliance and would not affect her appearance on stage. Although the literature suggests that patients can gradually acclimate to bite-jumping appliances, it was clear that a less cumbersome option would be preferred.17,18 In addition, the treatment mechanics needed to favor mandibular advancement because of the patient’s retrusive mandible and normal maxillary position. Class II camouflage treatment involving the extraction of upper premolars and maxillary dental compensation was ruled out for esthetic reasons, since the nasolabial angle was within normal limits and maxillary crowding was minimal. Asymmetrical extractions followed by clear-aligner therapy with pontics in the extraction sites would have been a more esthetic alternative, but this was rejected because it required a high degree of patient compliance.
Our strategy therefore focused on improving the maxillary and mandibular archforms and enhancing mandibular advancement, using TADs to avoid excessive proclination of the lower incisors and reduce the need for patient cooperation.
Treatment Progress
Treatment began with rapid maxillary expansion from a Hyrax* appliance anchored to the first molars and bonded to the palatal surfaces of the canines. After four months of expansion, the mandibular teeth were bonded with .022" × .028" preadjusted brackets**; the maxillary teeth were bonded two months later. Leveling and alignment were achieved with two months each of .014" and .016" × .022" nickel titanium archwires.
A miniscrew*** was then inserted on each side in the mandibular buccal bone between the roots of the first molars and second premolars (Fig. 2).
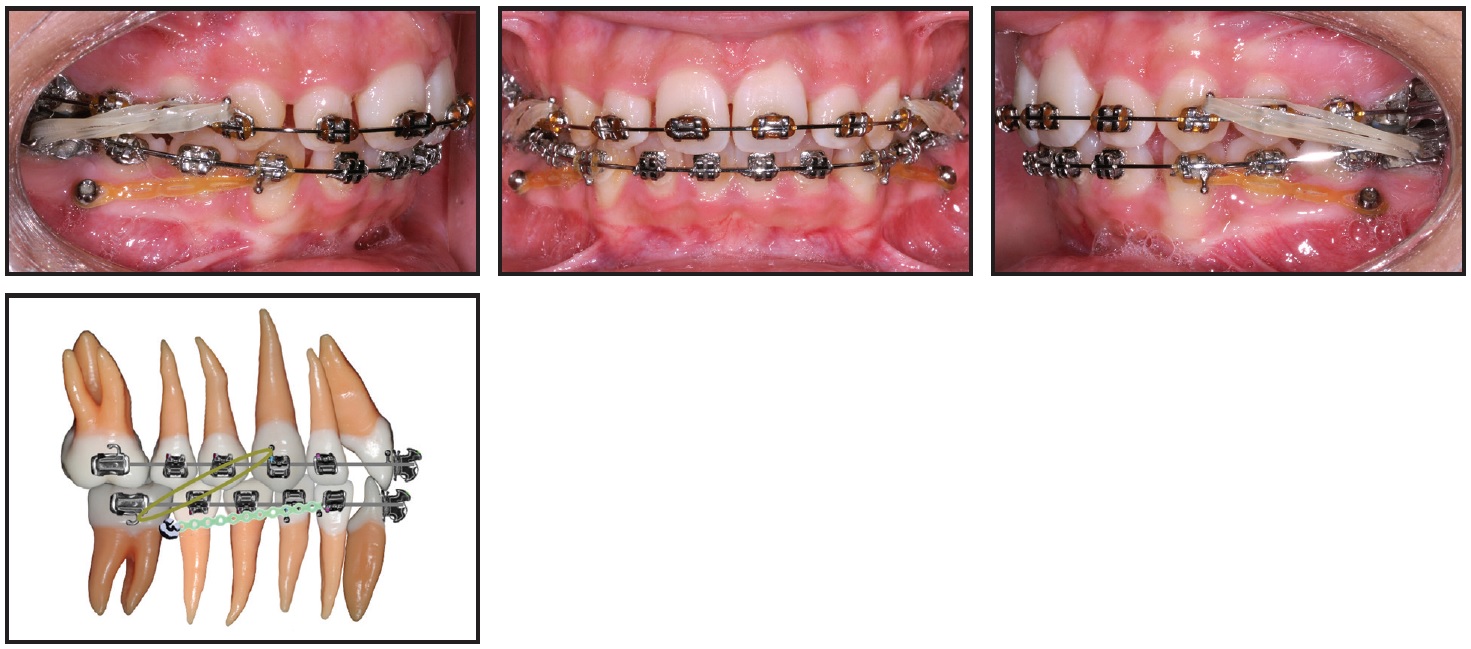
Fig. 2 After 10 months of treatment, miniscrew*** inserted and 100g power chain attached to canine on each side; .017" × .025" stainless steel archwires placed and 2.5oz, 7.9mm Class II elastics initiated.
Elastic power chain (100g) was stretched between the miniscrew and the lower canine to reinforce anchorage and minimize flaring of the lower incisors. The power chain was replaced every 28 days. Class II correction was accomplished using progressively stronger Class II elastics coupled with rectangular stainless steel wires. During the first month, .017" × .025" stainless steel archwires and 2.5oz, 7.9mm elastics were worn 22 hours per day. This routine was followed by .021" × .028" stainless steel archwires and 4.5oz, 3.2mm elastics worn full-time for six months and then only at night for four months. Finally, 6.5oz, 3.2mm elastics were worn for three months to improve intercuspation.
The upper arch was debonded first, and the lower arch two months later. Total treatment time was 26 months. Removable wraparound retainers were delivered for both arches.
Treatment Results
The results were a balanced profile with an esthetic and pleasing smile, harmony between the upper and lower lips, lip competence, and bilateral Class I canine and molar relationships (Fig. 3).
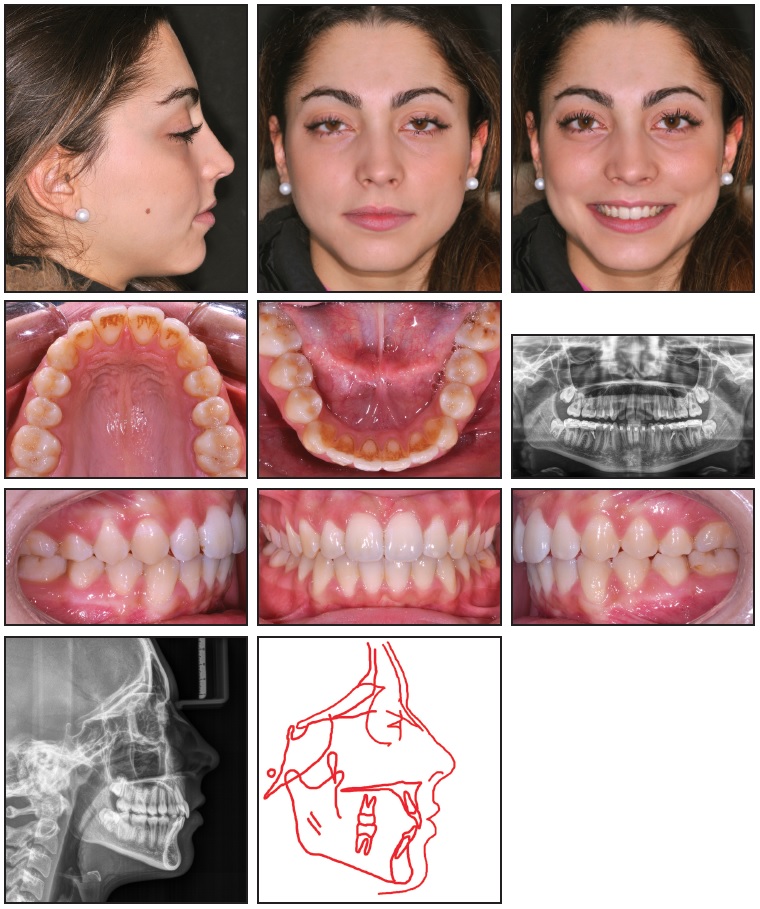
Fig. 3 Patient after 26 months of treatment (panoramic radiograph taken two months before debonding).
The dental midlines were corrected, and no muscle or joint problems had developed.
A panoramic radiograph taken two months before debonding showed acceptable root angulations, no evidence of root resorption, and stable bone levels. The x-ray did reveal a lack of space for proper eruption of the lower third molars.
Post-treatment cephalometric analysis showed that the sagittal jaw relationship improved while facial height remained constant (Table 1). There was a mild increase in lower incisor inclination, but the measurement was still within normal limits. The overjet was corrected, addressing the patient’s initial complaint of protrusive teeth. She was satisfied with the overall esthetics and treatment outcome.
One year after the end of treatment, the patient’s facial appearance was unchanged (Fig. 4).
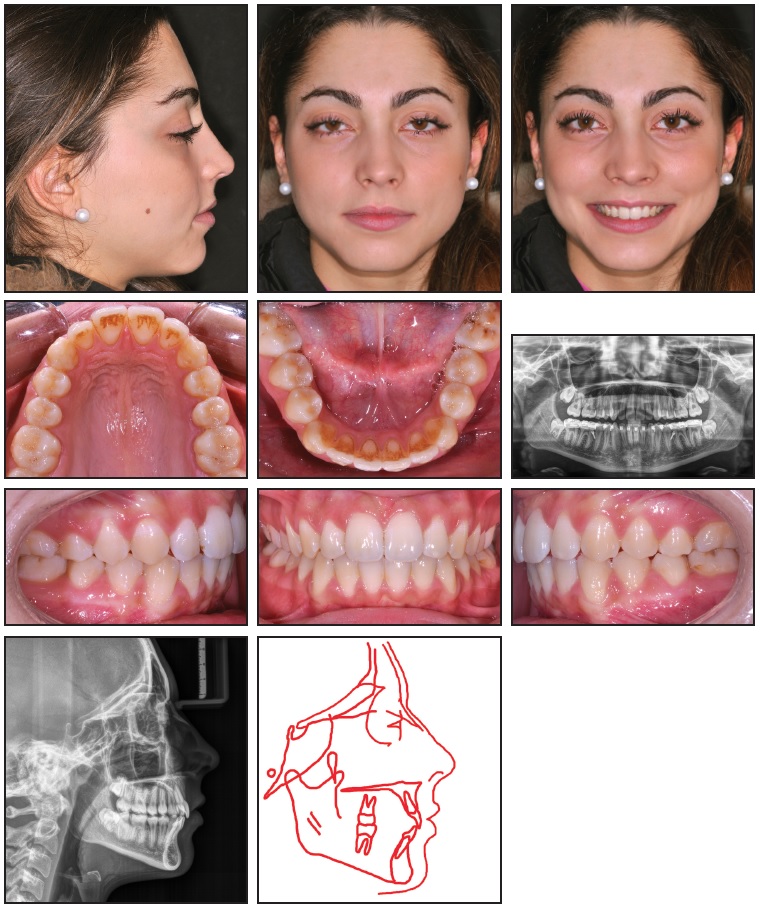
Fig. 4 Patient one year after treatment.
No substantial occlusal modification had occurred, and the archforms and alignment were maintained.
Discussion
Treatment planning involves many factors, including the patient’s attitude and willingness to cooperate and the efficiency, cost, and side effects of potential appliances. Elastics remain one of the most popular and effective means of correcting Class II malocclusions. Multiple studies have reported a lack of strong evidence that the use of Class II elastics results primarily in negative side effects, as was previously suggested.4,6,19 Class II elastics do require some patient compliance, but they tend to be more patient-friendly and tolerable and are less expensive than bite-jumping devices. As the present case shows, when Class II elastics are supported by skeletal anchorage, the adverse effects of elastics alone are minimized and the ability to advance the mandible is improved.
The mechanism of ligating the teeth to the miniscrews is crucial. Our decision to use power chain instead of stainless steel ligature wire to reinforce the anterior anchorage unit was based on research showing that miniscrew implants tend to migrate in the direction of traction.20 Power chain, with its inherent elasticity, produces more constant traction, but simultaneously causes a slight forward movement of the miniscrew toward the incisors and a reciprocal backward movement of the anterior segment toward the miniscrew implant. Therefore, there is no anterior anchorage loss.15,21
In our case, this dual-anchorage setup of Class II elastics reinforced with TADs produced a protrusive effect on the mandible, taking advantage of the patient’s growth spurt while controlling dental side effects. Additionally, the anchorage design avoided any significant change in the vertical dimension during sagittal correction of the Class II malocclusion. The occlusal plane remained almost stable (2° increase), and no lower molar extrusion occurred. Although the lower molars were not anchored directly to the TADs, the force of the elastics on the archwire restricted anteroposterior and vertical dental movements. There was a slight proclination (5°) of the lower incisors, but this might have been attributable more to unraveling of the crowding than to unwanted flaring from the Class II correction.
FOOTNOTES
- *Registered trademark of Dentaurum, Inc., Newtown, PA; www.dentaurum.com.
- **Butterfly System, Trademark of American Orthodontics, Sheboygan, WI; www.americanortho.com.
- ***Micerium Anchorage System, Micerium S.p.A., Avegno, Italy; www.micerium.it.
REFERENCES
- 1. Jasper, J.J. and McNamara, J.A. Jr.: The correction of interarch malocclusions using a fixed force module, Am. J. Orthod. 108:641-650, 1995.
- 2. Proffit, W.R.; Fields, H.W.; and Moray, L.J.: Prevalence of malocclusion and orthodontic treatment need in the United States: Estimates from the NHANES III survey, Int. J. Adult Orthod. Orthog. Surg. 13:97-106, 1998.
- 3. McNamara, J. Jr.: Components of a Class II malocclusion in children 8-10 years of age, Angle Orthod. 51:177-202, 1981.
- 4. Buchner, H.J.: Maintaining mandibular anchorage in Class II, division 1, treatment, Angle Orthod. 19:231-249, 1949.
- 5. Nelson, B.; Hansen, K.; and Hägg, U.: Overjet reduction and molar correction in fixed appliance treatment of Class II, division 1, malocclusions: Sagittal and vertical components, Am. J. Orthod. 115:13-23, 1999.
- 6. Janson, G.; de Freitas, M.R.; Araki, J.; Franco, E.J.; and Barro, S.E.: Class III subdivision malocclusion corrected with asymmetric intermaxillary elastics, Am. J. Orthod. 138:221-230, 2010.
- 7. Ellen, E.K.; Schneider, B.J.; and Sellke, T.: A comparative study of anchorage in bioprogressive versus standard edgewise treatment in Class II correction with intermaxillary elastic force, Am. J. Orthod. 114:430-436, 1998.
- 8. Serbesis-Tsarudis, C. and Pancherz, H.: “Effective” TMJ and chin position changes in Class II treatment, Angle Orthod. 78:813-818, 2008.
- 9. Nelson, B.; Hägg, U.; Hansen, K.; and Bendeus, M.: A long-term follow-up study of Class II malocclusion correction after treatment with Class II elastics or fixed functional appliances, Am. J. Orthod. 132:499-503, 2007.
- 10. Nelson, B.; Hansen, K.; and Hägg, U.: Class II correction in patients treated with Class II elastics and with fixed functional appliances: A comparative study, Am. J. Orthod. 118:142-149, 2000.
- 11. Wiedel, A.P. and Bondemark, L.: A randomized controlled trial of self-perceived pain, discomfort, and impairment of jaw function in children undergoing orthodontic treatment with fixed or removable appliances, Angle Orthod. 86:324-330, 2016.
- 12. Bergius, M.; Kiliaridis, S.; and Berggren, U.: Pain in orthodontics: A review and discussion of the literature, J. Orofac. Orthop. 61:125-137, 2000.
- 13. Johal, A.; Fleming, P.S.; and Al Jawad, F.A.: A prospective longitudinal controlled assessment of pain experience and oral health-related quality of life in adolescents undergoing fixed appliance treatment, Orthod. Craniofac. Res. 17:178-186, 2014.
- 14. Firestone, A.R.; Scheurer, P.A.; and Bürgin, W.B.: Patients’ anticipation of pain and pain-related side effects, and their perception of pain as a result of orthodontic treatment with fixed appliances, Eur. J. Orthod. 21:387-396, 1999.
- 15. Manni, A.; Pasini, M.; and Mauro, C.: Comparison between Herbst appliances with or without miniscrew anchorage, Dent. Res. J. (Isfahan) 9:S216-S221, 2012.
- 16. Kinzinger, G.S.; Gülden, N.; Yildizhan, F.; and Diedrich, P.R.: Efficiency of a skeletonized Distal Jet appliance supported by miniscrew anchorage for noncompliance maxillary molar distalization, Am. J. Orthod. 136:578-586, 2009.
- 17. Souki, B.Q.; Bastos, B.D.; Araujo, L.F.; Moyses-Braga, W.F.; Pantuzo, M.G.; and Cheib, P.L.: Effective and efficient Herbst appliance therapy for skeletal Class II malocclusion patient with a low degree of collaboration with the orthodontic treatment, Case Rep. Dent. 2015:986597, 2015.
- 18. Silva, J.F.; Gerszewski, C.; Moresca, R.C.; Correr, G.M.; Flores-Mir, C.; and Moro, A.: Retrospective study of clinical complications during orthodontic treatment with either a removable mandibular acrylic splint Herbst or with a cantilever Herbst, Angle Orthod. 85:64-71, 2015.
- 19. Wehrbein, H.; Feifel, H.; and Diedrich, P.: Palatal implant anchorage reinforcement of posterior teeth: A prospective study, Am. J. Orthod. 116:678-686, 1999.
- 20. Fritz, U.; Diedrich, P.; Kinzinger, G.; and Al-Said, M.: The anchorage quality of mini-implants towards translatory and extrusive forces, J. Orofac. Orthop. 64:293-304, 2003.
- 21. Manni, A.; Mutinelli, S.; Pasini, M.; Mazzotta, L.; and Cozzani, M.: Herbst appliance anchored to miniscrews with 2 types of ligation: Effectiveness in skeletal Class II treatment, Am. J. Orthod. 149:871-880, 2016.