THE CUTTING EDGE
Long-Distance Orthodontic Treatment with Adjunctive Light Therapy
This column is compiled by JCO Technology Editor W. Ronald Redmond, DDS, MS. To help keep our readers on The Cutting Edge, Dr. Redmond will spotlight a particular area of orthodontic technology every few months. Your suggestions for future subjects or authors are welcome.
Orthodontists are constantly looking for ways to improve the ease of treatment, patient comfort, and "throughput". Prescription bonded brackets and nickel titanium wires are just two examples of these efforts.
In our Cutting Edge column this month, Dr. Timothy Shaughnessy explores another trend in orthodontic treatment: accelerated orthodontics. During my five decades in the profession, various methods for speeding up treatment, including electrical stimulation and hormonal and chemical applications, have occasionally surfaced. None of these has gained widespread acceptance. Now gaining some traction, however, are both invasive procedures that stimulate the body's reparative process and noninvasive vibratory stimulation of the periodontal membrane.
Photobiomodulation (PBM) - borrowed from the medical profession, where it is used for acceleration of bone healing - has recently been adapted for use in orthodontics. PBM stimulates the mitochondria, causing them to produce additional adenosine triphosphate and thus accelerate tooth movement. The latest improvements have replaced lasers with light-emitting diodes (LEDs), as in the OrthoPulse* unit, which is inserted intraorally to irradiate the upper and lower arches for five minutes each per day.
Similar articles from the archive:
Dr. Shaughnessy describes how he used PBM to accelerate the orthodontic treatment of two long-distance patients, reducing their number of office visits. Combined with the efficient use of nickel titanium archwires and prescription brackets, PBM produced a dramatic effect on the overall treatment experience.
The acceleration of tooth movement, with a concomitant reduction in the required number of appointments, is the Holy Grail of orthodontics. We need to keep a close eye on this technology; it is likely to have a far-ranging impact, not only on orthodontic treatment but on our practice-management model.
WRR
Long-Distance Orthodontic Treatment with Adjunctive Light Therapy
Various techniques have been proposed to accelerate tooth movement and shorten orthodontic treatment time. Most require surgical intervention, lessening their acceptance by patients and clinicians.1-4 As an alternative, low-level light therapy (LLLT), also known as photobiomodulation (PBM), has recently been developed as a noninvasive method of accelerating orthodontic tooth movement.
LLLT delivers tissue-penetrating red or near-infrared light to the periodontium to promote connective- tissue and bone remodeling.5,6 Cytochrome c oxidase, a component of the mitochondrial respiratory chain, is activated upon photon absorption, increasing adenosine triphosphate production. Nitric oxide bioavailability also increases, thus promoting microcirculation through angiogenesis at the irradiated sites. Reactive oxygen species produced in the mitochondria have also been identified as modulators of bone metabolism.7 Preliminary data indicate that LLLT is safe and effective in accelerating tooth movement.8-10
Accelerated treatment is advantageous not only for patients who may be concerned about treatment duration, but also for those who are unable to attend frequent orthodontic appointments. When appointment intervals are extended, efficient tooth movement becomes even more critical in reducing treatment time. This article chronicles two long-distance patients treated with LLLT from OrthoPulse - a removable intraoral device that emits a continuous light of 850 nanometers by means of LEDs (Fig. 1) - in conjunction with comprehensive fixed-appliance therapy.
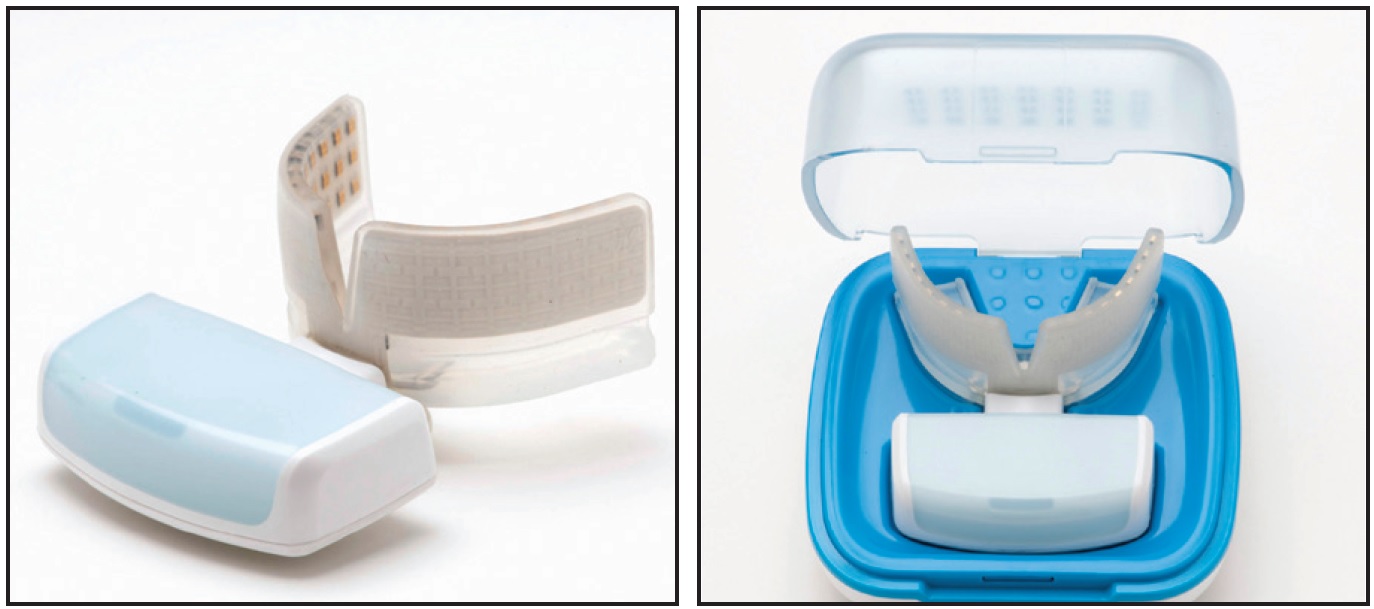
Fig. 1 OrthoPulse* low-level light therapy device.
Case 1
A 14-year-old female living in Charleston, South Carolina, presented to an office in suburban Atlanta for orthodontic treatment. Clinical examination showed inadequate space for the upper and lower left canines, mild lower-incisor malalignment, and relative extrusion of the upper central incisors (Fig. 2).
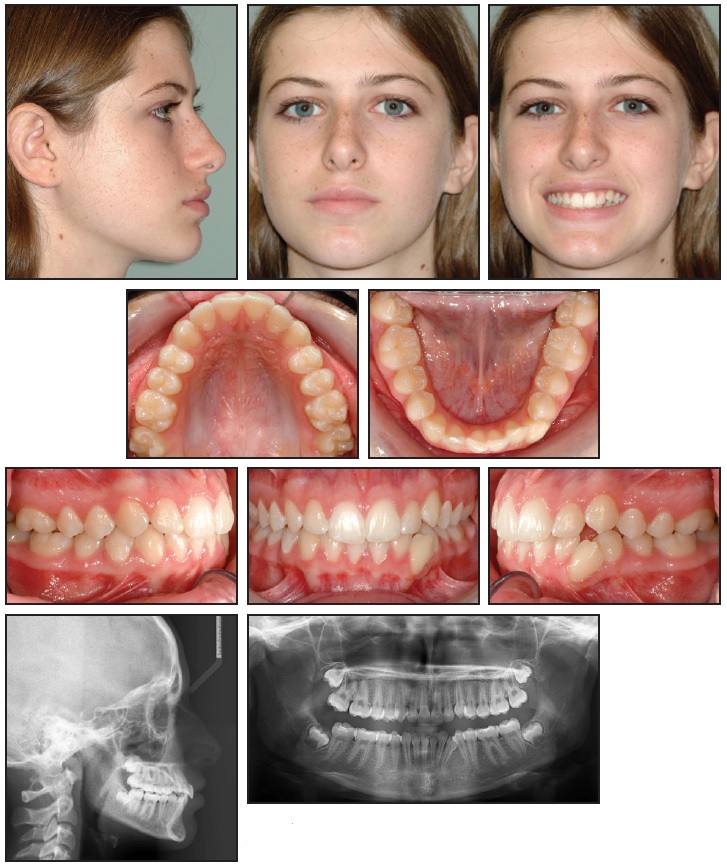
Fig. 2 Case 1. 14-year-old female with lower anterior crowding before treatment.
The interarch relationship was Class I on both sides, but the patient had a mildly excessive overbite. The mandibular dental midline was deviated to the left, reflecting the space shortage for the lower left canine; there was minimal attached gingiva on the facial surface of the displaced tooth. Cephalometric and facial evaluation indicated a skeletal Class I relationship with a normal vertical dimension. The panoramic x-ray revealed significant root divergence between the lower left canine and the adjacent first premolar. All four developing third molars were present.
Nonextraction treatment was proposed as a "therapeutic diagnosis". If advancement of the anterior teeth became excessive following alignment, extractions would then be considered. Particular concerns with nonextraction treatment were a negative effect on facial esthetics and an increased risk of gingival recession. The patient agreed to use an OrthoPulse for five minutes per arch per day (Fig. 3).
Treatment began with .018" Mini Diamond** brackets on all teeth, except for a button on the lower left canine, and .014" nickel titanium arch- wires (Fig. 4).
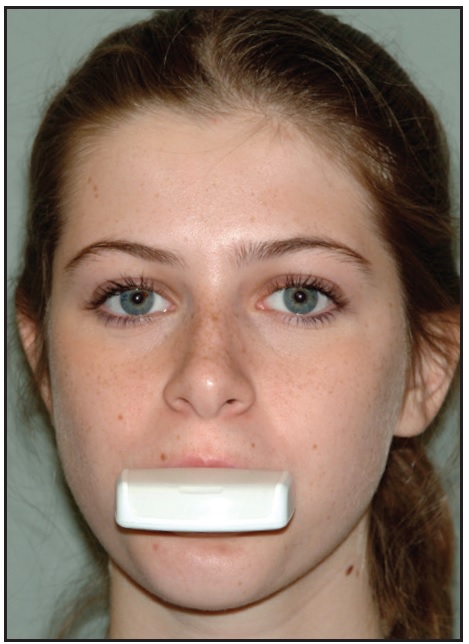
Fig. 3 Case 1. OrthoPulse used for five minutes per arch per day.
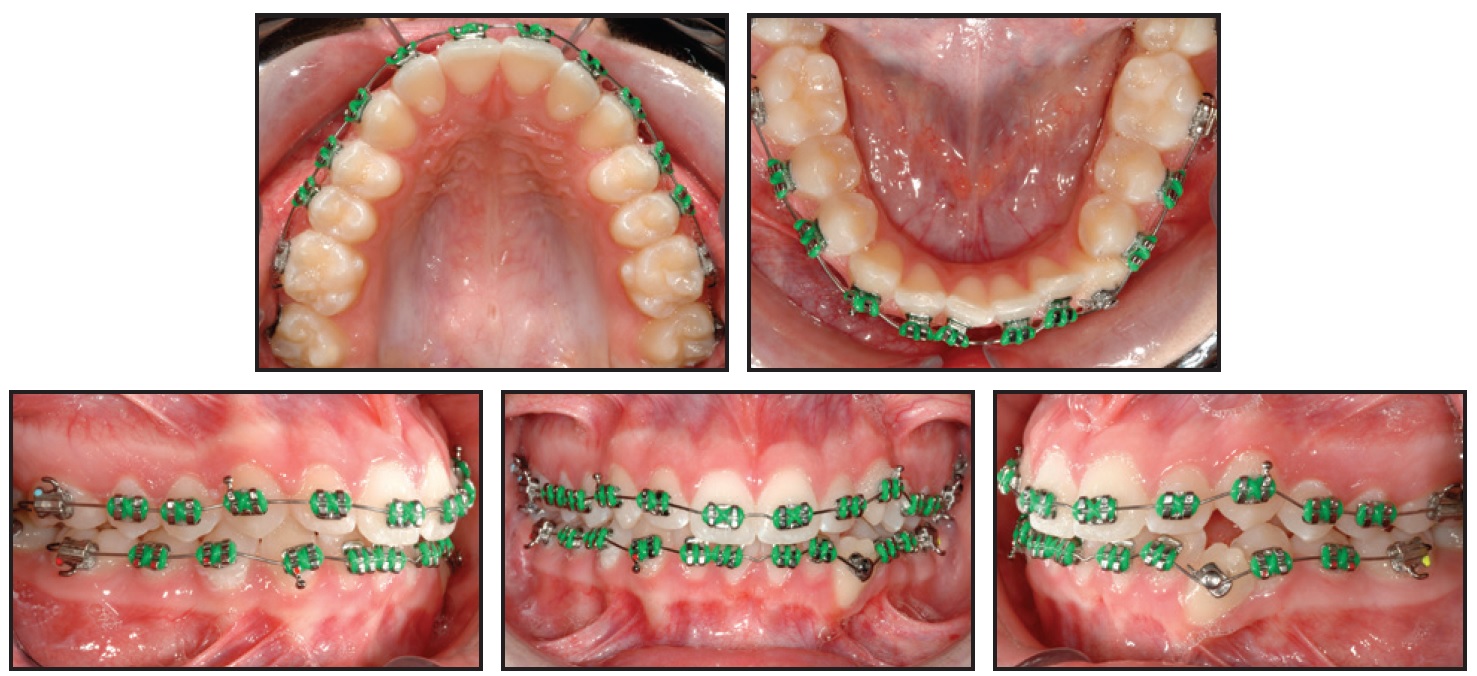
Fig. 4 Case 1. Initial placement of .018" Mini Diamond** brackets and .014" nickel titanium archwires.
Twelve weeks later, the archwires were changed to .016" × .016" nickel titanium in the maxillary arch and .016" nickel titanium in the mandibular arch, and a coiled spring was placed over the lower left canine button to gain space (Fig. 5).
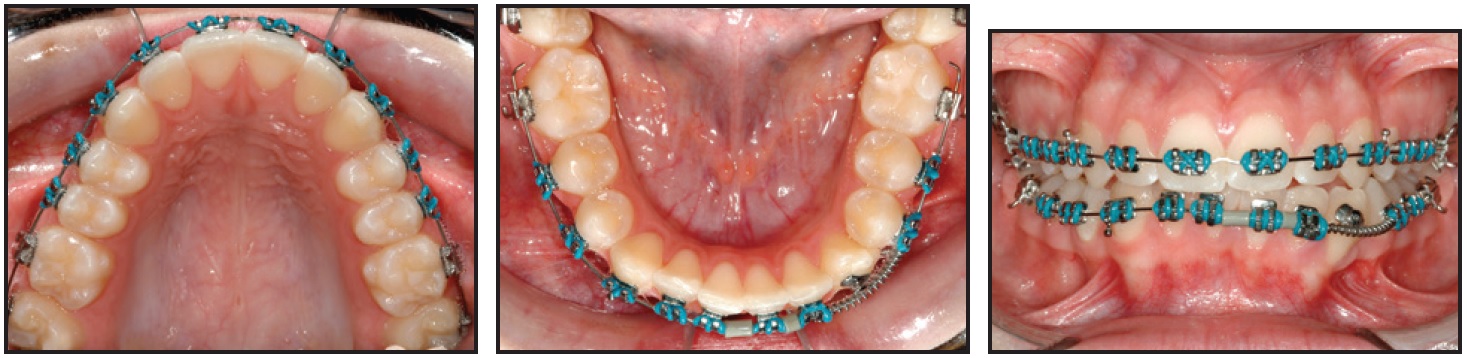
Fig. 5 Case 1. After 12 weeks of treatment, placement of .016" × .016" nickel titanium maxillary archwire and .016" nickel titanium mandibular archwire.
Ten weeks later, the canine was bracketed, the mandibular archwire was reduced to .014" nickel titanium and extended to the lower left second molar, and the maxillary archwire was changed to .016" × .016" stainless steel (Fig. 6).
After 28 weeks of treatment, the mandibular archwire was increased to .016" nickel titanium; seven weeks later, an .016" × .022" nickel titanium archwire was placed (Fig. 7). A lingual button was bonded to the upper left canine for attachment of a crossbite elastic, facilitating the transverse correction and differential extrusion of the mandibular teeth connected by the flexible archwire. Detailing bends were made in the maxillary anterior segment of the stiffer stainless steel archwire.
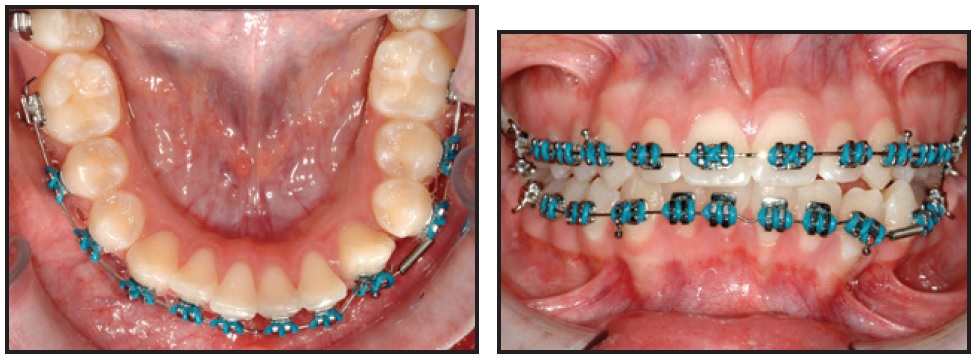
Fig. 6 Case 1. After 22 weeks of treatment, bracketing of lower left canine and placement of .014" nickel
titanium mandibular archwire, extended to lower left second molar, and .016" × .016" stainless steel maxillary
archwire.
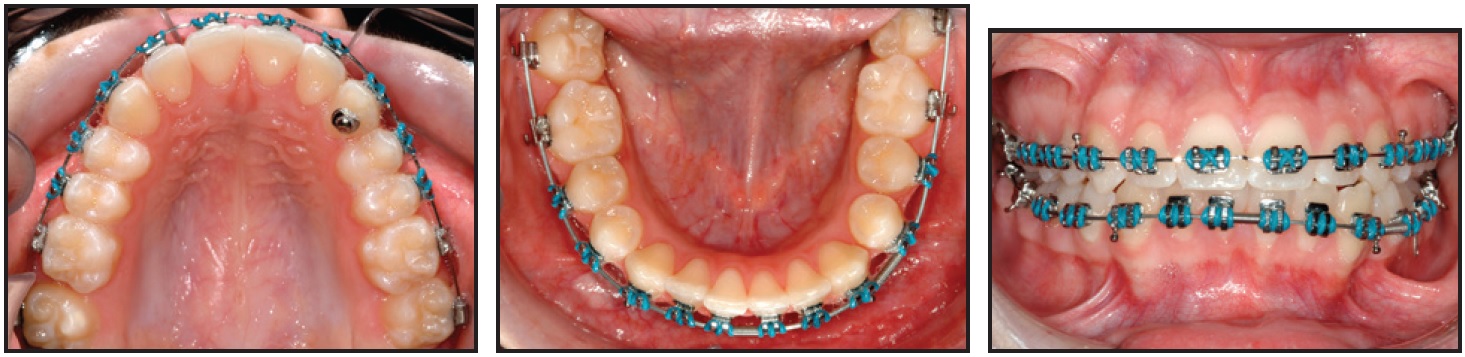
Fig. 7 Case 1. After 35 weeks of treatment, placement of .016" × .022" nickel titanium mandibular archwire.
After 42 weeks of treatment, an .016" × .016" stainless steel archwire was placed in the mandibular arch, with elastic chain added for space closure in the left quadrant (Fig. 8). Nine weeks later, because the overjet had increased slightly with the lower space closure, appropriate elastics were added for overjet correction (Fig. 9). Another five weeks later, the fixed appliances were removed and a fixed retainer was bonded in the mandibular arch, extending to the lower left first premolar to avoid relapse of the adjacent canine.
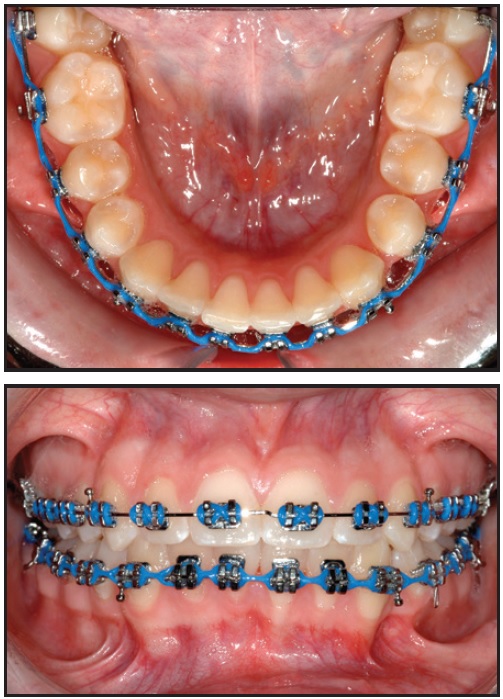
Fig. 8 Case 1. After 42 weeks of treatment, placement of .016" × .016" stainless steel mandibular archwire for space closure with elastic chain.

Fig. 9 Case 1. After 51 weeks of treatment, attachment of elastics for interarch correction.
This patient was seen nine times during 13 months of treatment, including the day of bracket placement and the day of bracket removal and retainer placement. Extraoral evaluation showed the lower lip slightly ahead of the E-line (Fig. 10). Lip competence was maintained, even though both the anterior teeth and lips were mildly advanced. The other primary concern with nonextraction treatment was the minimal attached gingiva overlying the labially displaced lower left canine. The tissue in this area appeared to improve, as the tooth was moved lingually into a better position over the alveolar ridge. The panoramic x-ray also showed that the canine root was tipped distally by a significant amount to achieve root parallelism. Unfortunately, efforts to level the marginal ridges between the lower right first and second molars inadvertently produced excessive mesial root angulation of the second molar.
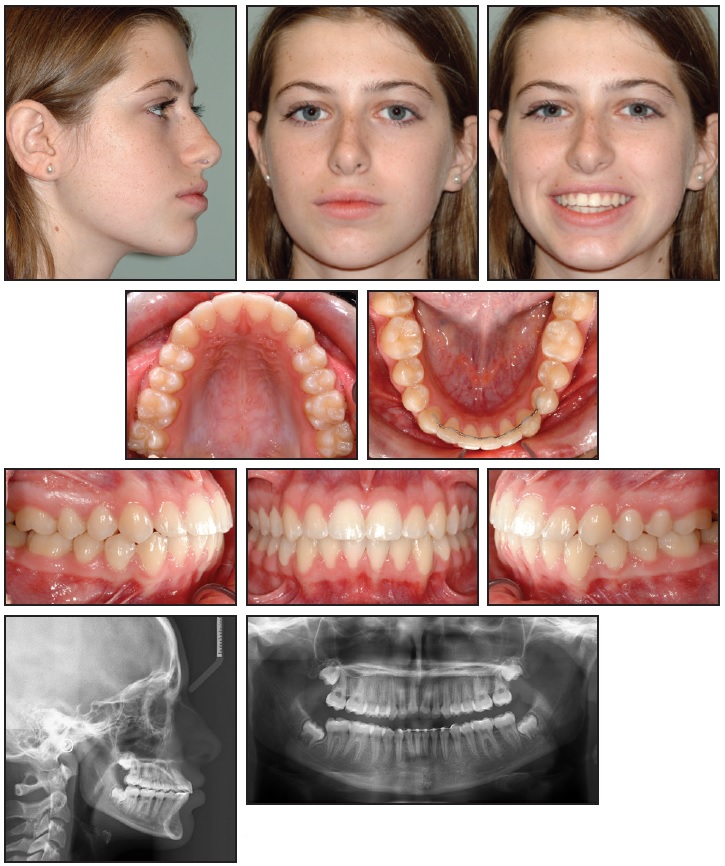
Fig. 10 Case 1. Patient after 13 months of treatment.
The teeth were well aligned in both arches, and the left canines were brought into good static and functional occlusion. The Class I molar and canine relationship was maintained, while the midline was corrected. The bite was opened in part by intruding the upper central incisors to harmonize the gingival margins of the maxillary anterior teeth. Anterior guidance in protrusive movement still resulted in disclusion of the posterior teeth.
Case 2
The 12-year-old younger sister of the patient shown in Case 1 also presented for orthodontic treatment, and likewise was treated long distance. She had a unilateral left Class II dentition, a maxillary right midline discrepancy, and mildly excessive overjet (Fig. 11).
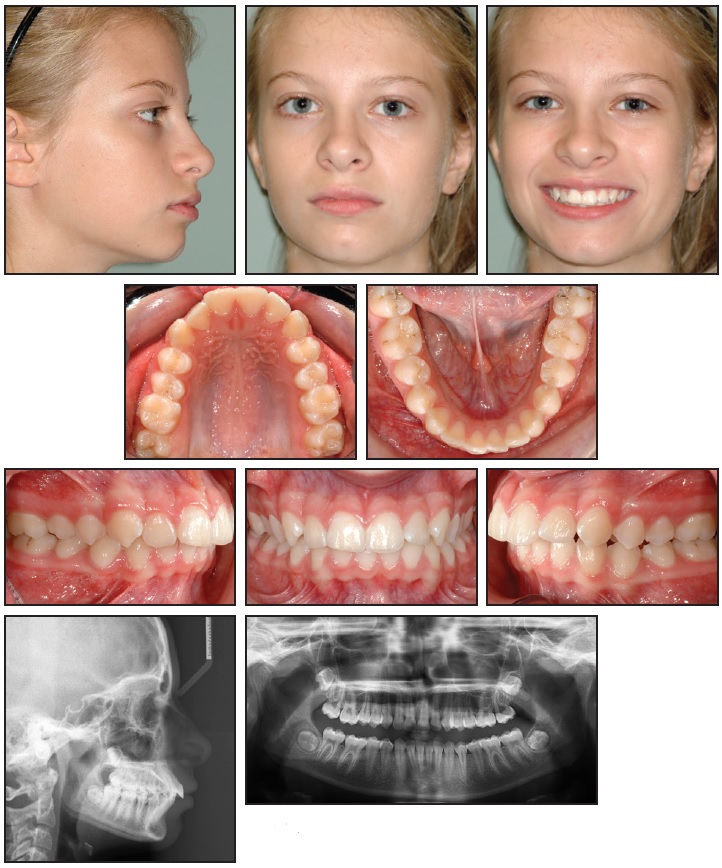
Fig. 11 Case 2. 12-year-old female with unilateral left Class II relationship and maxillary right midline deviation before treatment.
A mild malalignment of the anterior teeth was accompanied by rotation of the upper and lower right second premolars. All four third molars were immature and present on the panoramic x-ray. Cephalometric analysis confirmed a mild skeletal Class II relationship and a normal vertical dimension. Frontal and profile facial esthetics were pleasing, and there were no periodontal concerns.
Extraction of a premolar in the maxillary left quadrant was proposed for efficient and predictable correction of the asymmetrical occlusion. This plan would also reduce the need for auxiliary appliances and patient compliance. Unilateral space closure would result in overjet reduction, Class II canine correction, and movement of the maxillary dental midline to the left. As in Case 1, the patient agreed to wear an OrthoPulse for five minutes per arch per day.
Initially, .018" Mini Diamond brackets and an .014" nickel titanium archwire were placed only in the maxillary arch (Fig. 12). Since anchorage demands were low, the patient was referred to her pediatric dentist for extraction of the upper left second premolar, which was smaller than the adjacent first premolar and also slightly rotated and tipped. Five weeks later, brackets were bonded to the mandibular teeth and an .014" nickel titanium archwire was fully engaged; the maxillary archwire was increased to .016" nickel titanium (Fig. 13).
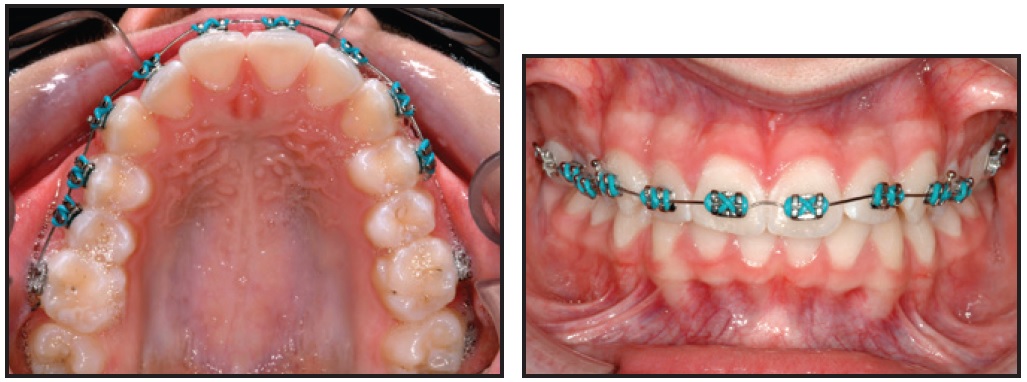
Fig. 12 Case 2. Initial placement of maxillary brackets and .014" nickel titanium archwire, before extraction of upper left second premolar.
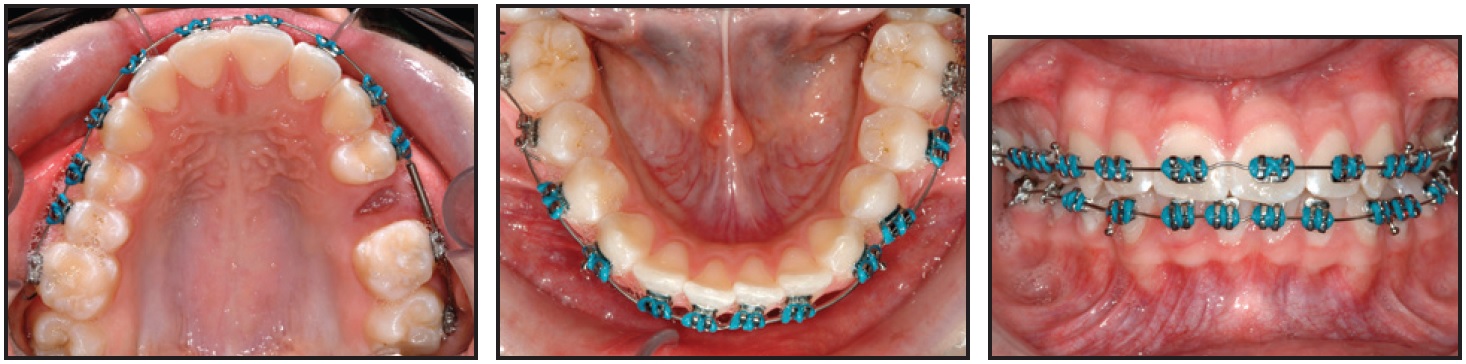
Fig. 13 Case 2. After five weeks of treatment, addition of mandibular brackets and .014" nickel titanium archwire and placement of .016" nickel titanium maxillary archwire.
Ten weeks later, the maxillary archwire was changed to .016" × .022" nickel titanium and the mandibular archwire to .016" nickel titanium. Another seven weeks later, the mandibular archwire was increased to .016" × .016" nickel titanium.
After 28 weeks of treatment, .016" × .022" archwires were placed in both arches, stainless steel in the upper and nickel titanium in the lower (Fig. 14).
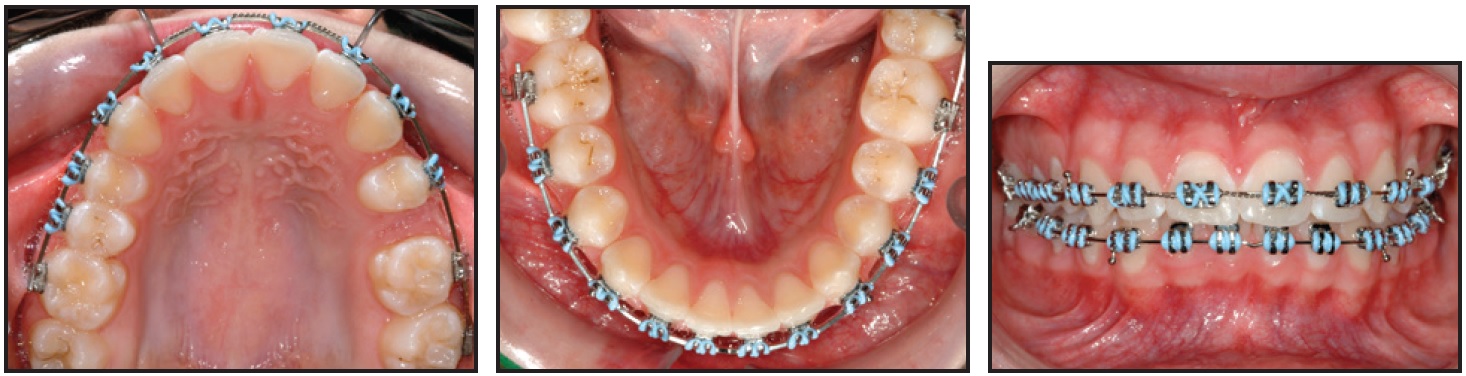
Fig. 14 Case 2. After 28 weeks of treatment, placement of .016" × .022" stainless steel maxillary and nickel titanium mandibular archwires.
Space closure was not initiated for seven more weeks, giving the maxillary archwire an opportunity to fit passively. Elastic chain was used for space closure instead of a self-limiting closing-loop archwire. Nine weeks later, after about half the space had been closed at a rate of 1.4mm per month, the elastic chain was replaced and Class II elastics were added for midline control (Fig. 15).
A colleague in Charleston replaced the elastic chain in another six weeks, saving the patient a trip to Atlanta. After 13 months of treatment, the elastic chain was replaced for the last time. Two months later, the patient returned for debonding of fixed appliances and placement of a mandibular bonded retainer.
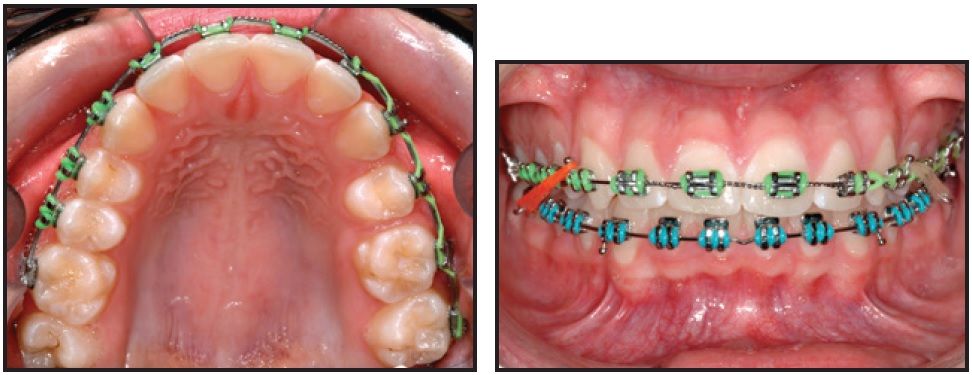
Fig. 15 Case 2. After 44 weeks of treatment, including nine weeks of space closure with elastic chain.
This patient was seen 10 times during her 15 months of treatment, including the day of initial bracket placement and the day of bracket removal and retainer placement. After treatment, although the facial esthetic change was unremarkable, the maxillary dental midline coincided with the midfacial axis and the center of the philtrum in smiling (Fig. 16).
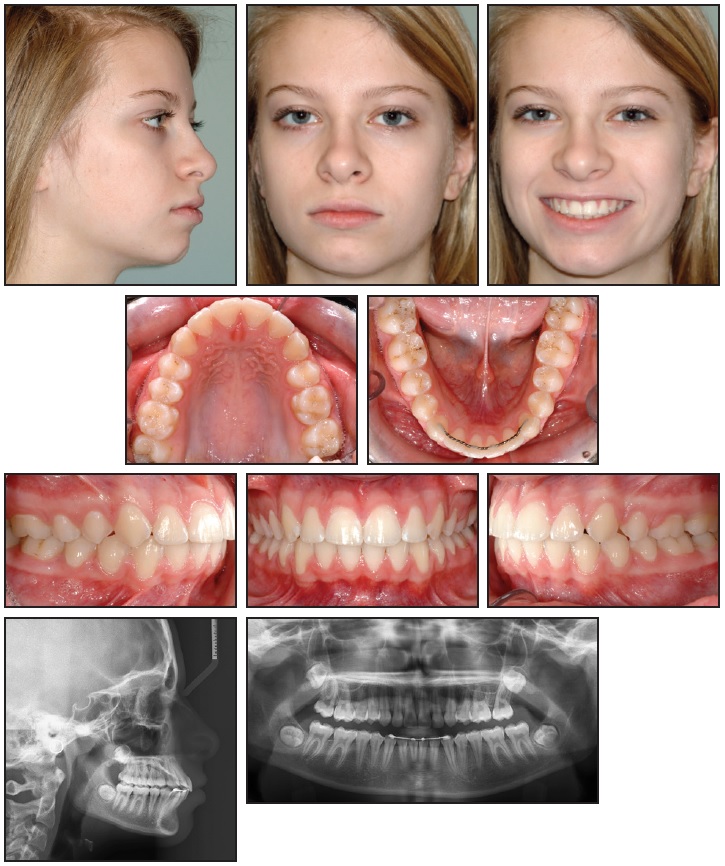
Fig. 16 Case 2. Patient after 15 months of treatment.
Unilateral maxillary space closure resulted in correction of the midline discrepancy, the left Class II canine occlusion, and the excessive overjet. While all the teeth were aligned, a small space persisted between the upper left canine and first premolar - ironically, not at the second-premolar extraction site. Despite the limited space, the teeth fit well and a good functional occlusion was established. The panoramic x-ray confirmed good root parallelism, even at the extraction site. Cephalometric evaluation indicated a mild increase in lower-incisor proclination, secondary to bite opening, and a resolution of the anterior crowding.
Discussion
Although noninvasive, device-assisted techniques such as electrical currents11 and resonance vibration technology12 have been explored in the hope of reducing treatment time, their effects have not been substantiated. In a recent clinical trial, Woodhouse and colleagues found no evidence that supplemental vibrational force significantly increased the rate of alignment or reduced treatment time when used in conjunction with fixed appliances.13
LLLT is the most recent technique developed to enhance biological tooth movement.14-17 In medicine, LLLT has been used to promote wound healing18 and neurorehabilitation.19 In dentistry, it has been employed for pain reduction20 and in both hard- and soft-tissue applications.21,22 Although the first LLLT devices used lasers, LEDs are less expensive and safer because they produce more diffuse light.23 OrthoPulse allows patients to treat themselves at home, which is more practical, time-efficient, and reproducible than laser light delivery in the office.
In the two cases presented here, while treatment times were shorter than would normally be anticipated, the exact reduction would be impossible to quantify. Unlike clear-aligner therapy, which involves a predetermined number of trays, fixed-appliance treatment cannot be forecast in precise time intervals. Several investigators have attempted to evaluate the velocity of tooth movement with LED-LLLT during the alignment and space-closure phases of fixed-appliance treatment. Kau and colleagues showed a statistically significant twofold increase in the rate of alignment with the addition of daily near-infrared LED treatment.8 In a randomized controlled trial, Samara found a 30% increase in the velocity of en masse space closure in children and a 50% increase in adults with daily LED-LLLT.24 These studies indicate a potential one- to two-month reduction in treatment time.
Further clinical trials will be required to better understand the effects of PBM over the entire length of fixed-appliance treatment, including procedures such as leveling, anteroposterior correction, 3rd-order tooth movement, and finishing. It is not unreasonable to suppose that the mechanism for accelerated tooth movement acts throughout treatment, provided the PBM continues on a daily basis. As every clinician knows, however, any savings in treatment time could be negated by missed appointments, broken appliances, poor cooperation, or delayed eruption of teeth. None of those factors applied to the two patients shown in this article.
FOOTNOTES
- *Registered trademark of Biolux Research Ltd., Vancouver, British Columbia, Canada; www.bioluxresearch.com.
- **Registered trademark of Ormco Corporation, Orange, CA; www.ormco.com.
REFERENCES
- 1. Long, H.; Pyrakurel, U.; Wang, Y.; Liao, L.; Zhou, Y.; and Lai, W.: Interventions for accelerating orthodontic tooth movement: A systematic review, Angle Orthod. 83:164-171, 2013.
- 2. Gkantidis, N.; Mistakidis, I.; Kouskoura, T.; and Pandis, N.: Effectiveness of non-conventional methods for accelerated orthodontic tooth movement: A systematic review and meta-analysis, J. Dent. 42:1300-1319, 2014.
- 3. Hassan, A.H.; Al-Fraidi, A.A.; and Al-Saeed, S.H.: Corticotomy-assisted orthodontic treatment: Review, Open Dent. J. 4:159-164, 2010.
- 4. Singh, V.P.; Roychodhury, S.; Vineet; and Nigam, P.: Drug induced orthodontic tooth movement—A review, J. Adv. Med. Dent. Sci. Res. 3:191-195, 2015.
- 5. Chung, H.; Dai, T.; Sharma, S.K.; Huang, Y.Y.; Carroll, J.D.; and Hamblin, M.R.: The nuts and bolts of low-level laser (light) therapy, Ann. Biomed. Eng. 40:516-533, 2012.
- 6. Ross, G. and Ross, A.: Low level lasers in dentistry, Gen. Dent. 56:629-634, 2008.
- 7. Prindeze, N.J.; Moffatt, L.T.; and Shupp, J.W.: Mechanisms of action for light therapy: A review of molecular interactions, Exp. Biol. Med. 237:1241-1248, 2012.
- 8. Kau, C.H.; Kantarci, A.; Shaughnessy, T.; Vachiramon, A.; Santiwong, P.; de la Fuente, A.; Skrenes, D.; Ma, D.; and Brawn, P.: Photobiomodulation accelerates orthodontic alignment in early phase of treatment, Prog. Orthod. 14:30, 2013.
- 9. Nimeri, G.; Kau, C.H.; Corona, R.; and Shelly, J.: The effect of photobiomodulation on root resorption during orthodontic treatment, Clin. Cosmet. Investig. Dent. 6:1-8, 2014.
- 10. Genc, G.; Kocadereli, I.; Tasar, F.; Kilinc, K.; El, S.; and Sarakarati, B.: Effect of low-level laser therapy (LLLT) on orthodontic tooth movement, Lasers Med. Sci. 28:41-47, 2013.
- 11. Hashimoto, H.: Effect of micro-pulsed activity on experimental tooth movement, Nihon Kyosei Shika Gakkai Zasshi 49:352-361, 1990.
- 12. Nishimura, M.; Chiba, M.; Ohashi, T.; Sato, M.; Shimizu, Y.; Igarashi, K.; and Mitani, H.: Periodontal tissue activation by vibration: Intermittent stimulation by resonance vibration accelerates experimental tooth movement in rats, Am. J. Orthod. 133:572-583, 2008.
- 13. Woodhouse, N.R.; DiBiase, A.T.; Johnson, N.; Slipper, C.; Grant, J.; Alsaleh, M.; Donaldson, A.N.; and Cobourne, M.T.: Supplemental vibrational force during orthodontic alignment: A randomized trial, J. Dent. Res. 94:682-689, 2015.
- 14. Sousa, M.V.; Scanavini, M.A.; Sannomiya, E.K.; Velasco, L.G.; and Angelieri, F.: Influence of low-level laser on the speed of orthodontic tooth movement, Photomed. Laser Surg. 29:191-196, 2011.
- 15. Cruz, D.R.; Kohara, E.K.; Ribeiro, M.S.; and Wetter, N.U.: Effect of low-intensity laser therapy on the orthodontic movement velocity of human teeth: A preliminary study, Lasers Surg. Med. 35:117-120, 2004.
- 16. Youssef, M.; Ashkar, S.; Hamade, E.; Gutknecht, N.; Lampert, F.; and Mir, M.: The effect of low-level laser therapy during orthodontic movement: A preliminary study, Lasers Med. Sci. 23:27-33, 2008.
- 17. Doshi-Mehta, G. and Bhad-Patil, W.A.: Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: A clinical investigation, Am. J. Orthod. 141:289-297, 2012.
- 18. Posten, W.; Wrone, D.A.; Dover, J.S.; Arndt, K.A.; Silapunt, S.; and Alam, M.: Low-level laser therapy for wound healing: Mechanism and efficacy, Dermatol. Surg. 31:334-340, 2005.
- 19. Hashmi, J.T.; Huang, Y.Y.; Osmani, B.Z.; Sharma, S.K.; Naeser, M.A.; and Hamblin, M.R.: Role of low-level laser therapy in neurorehabilitation, PM&R 2:S292-S305, 2010.
- 20. Artés-Ribas, M.; Arnabat-Dominguez, J.; and Puigdollers, A.: Analgesic effect of low-level laser therapy (830 nm) in early orthodontic treatment, Lasers Med. Sci. 28:335-341, 2013.
- 21. Walsh, L.J.: The current status of low level laser therapy in dentistry, Part 1. Soft tissue applications, Aust. Dent. J. 42:247-254, 1997.
- 22. Walsh, L.J.: The current status of low level laser therapy in dentistry, Part 2. Hard tissue applications, Aust. Dent. J. 42:302-306, 1997.
- 23. Bozkurt, A. and Onaral, B.: Safety assessment of near infrared light emitting diodes for diffuse optical measurements, Biomed. Eng. Online 3:9, 2004.
- 24. Samara, S.A.: Velocity of orthodontic extraction space closure with and without photobiomodulation: A single center randomized clinical trial, thesis, European College University, Dubai, 2014.


