Long-Term Stability of Class II Correction with the Twin Force Bite Corrector
Numerous studies and case reports have highlighted the effectiveness of fixed-functional appliances in correcting Class II malocclusion, but long-term analyses of the stability of these results have seldom been reported in the literature. The following case series shows a follow-up evaluation of five Class II, division 1 patients treated with the Twin Force Bite Corrector (TFBC*), part of a prospective clinical study at the University of Connecticut Health Center.1
The overall treatment objectives in these cases were overjet reduction, achievement of a stable Class I molar and canine relation with coincident midlines, and improvement of the soft-tissue profile. Favorable treatment results were obtained in the short term and maintained for an average of six years after debonding in all five cases.
Appliance Design
The TFBC is a fixed push-type appliance clamped bilaterally to the upper and lower archwires. Each unit is made of two parallel 15mm cylinders housing nickel titanium coil springs (Fig. 1). A plunger is incorporated in each cylinder, at opposite ends. At the free ends of the plungers, hex nuts attach the appliance to the archwires mesial to the upper molars and distal to the lower canines. A constant force of approximately 210g is delivered on each side at full compression (Fig. 2). Since the appliance is muscle-driven, however, its exact force magnitude is difficult to quantify.
Similar articles from the archive:
- JCO ROUNDTABLE Stability of Orthodontic Treatment, Part 1 January 2006
- Important Aspects of Long-Term Stability September 1997
- Class II Correction with the Twin Force Bite Corrector April 2004
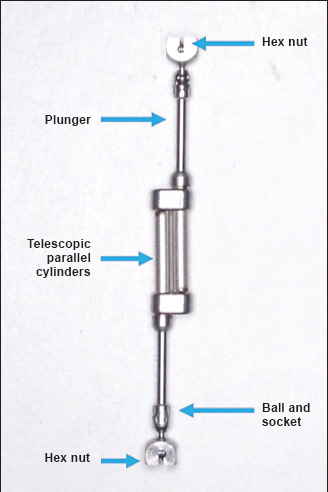
Fig. 1 Components of Twin Force Bite Corrector (TFBC).
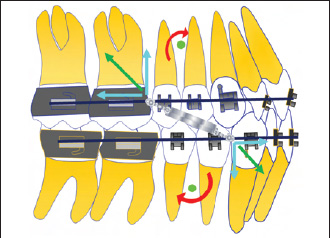
Fig. 2 Forces and moments produced by TFBC. Appliance is attached to archwire mesial to upper first molars, reducing distance between point of force application and center of resistance of upper arch. This generates smaller moment in upper arch than with other bite jumping appliances, where point of force application is distal to upper first molars.
Treatment Protocol
After initial leveling and alignment, the archwires are progressively increased to .019" x .025" stainless steel in the upper arch and .021" x .025" stainless steel in the lower. The archwires are cinched, consolidating each arch into a single unit to avoid space opening or flaring of the incisors. An .032" x .032" stainless steel transpalatal arch is placed to counteract the buccal forces exerted by the TFBC. Additionally, to prevent lower incisor flaring, lower anterior brackets with a negative torque prescription are used. When the standard TFBC is attached to the archwires mesial to the maxillary molars and distal to the lower canines, the mandible is postured forward in an anterior edge-to-edge relationship (Fig. 3).

Fig. 3 Treatment protocol for TFBC. A. 13-year-old male Class II patient before treatment. B. Upper .019" x .025" and lower .021" x .025" stainless steel archwires. C. After attachment of TFBC, mandible postured forward in edge-to-edge relationship. D. Overcorrected Class I molar and canine relationships after three months of TFBC wear. E. Finishing and detailing. F. Patient after 24 months of treatment.
During each visit, the nickel titanium springs should be removed from the telescoping units to check their integrity. The springs are reactivated if necessary, so that the patient is forced to bite in an edge-to-edge relationship. After three months of appliance wear, the patient usually shows overcorrected Class I molar and canine relationships, compensating for any relapse that could occur after appliance removal. Appropriate finishing and detailing are performed, and the patient is subsequently debonded (Fig. 3). The retention protocol involves a fixed 3-3 retainer for the lower arch and a removable wraparound retainer for the upper. Average treatment time is about 24 months.
Case 1
A 12-year-old prepubertal male presented with the chief complaint of a 100% deep bite (Fig. 4A). He had a Class II malocclusion due to a retrognathic mandible, displaying a full-cusp Class II molar relationship on both sides and more than 6mm of overjet.
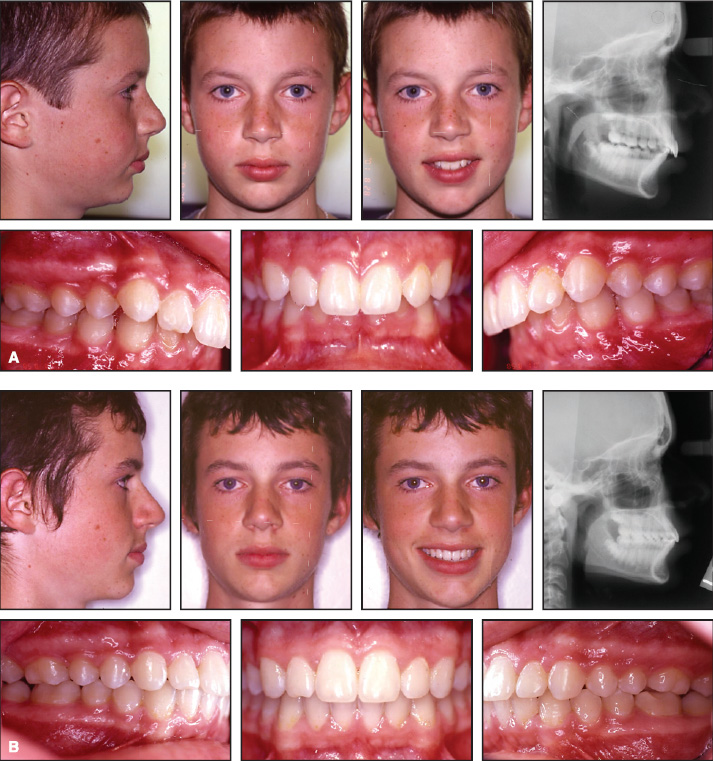
Fig. 4 Case 1. A. 12-year-old male patient with retrognathic mandible, deep bite, and 6mm overjet before treatment. B. Patient after 23 months of treatment, including three months of TFBC wear. (continued in next image)
After initial leveling and alignment, stiff upper .019" x .025" and lower .021" x .025" stainless steel archwires were placed, and the TFBC was attached with 5mm of activation. After three months of appliance wear, the patient exhibited an overcorrected Class I molar relationship. Finishing and detailing were accomplished with .017" x .025" CNA* beta titanium archwires and Class II elastics (Fig. 4B).
Post-treatment cephalometric analysis showed restriction of maxillary growth, redirection of mandibular growth, and mild proclination of the lower incisors (Table 1). Six years after appliance removal, no maxillary growth was observed; the mandible had continued to grow favorably, and the dental relationships had been maintained (Fig. 4C,D).
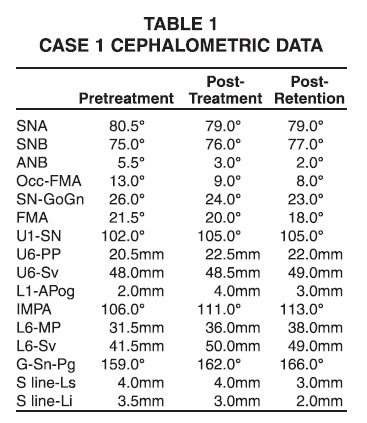
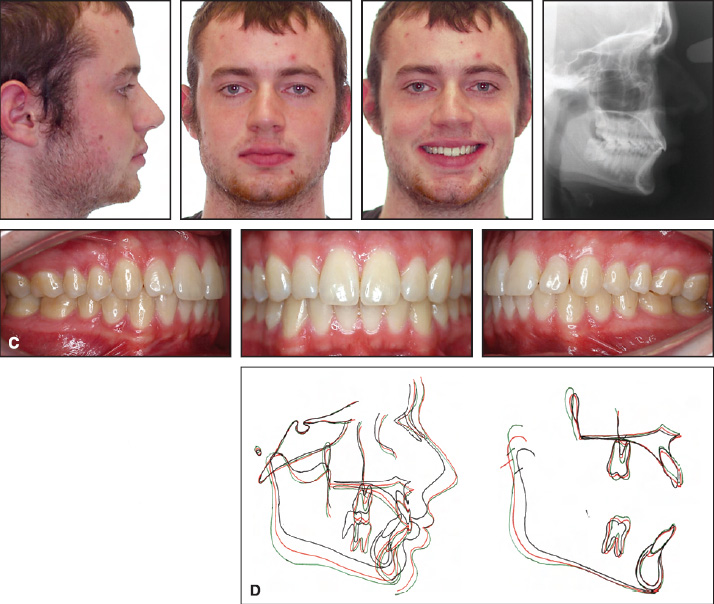
Fig. 4 Case 1 (cont.) C. Patient after six years of retention. D. Superimposition of pretreatment (black), post-treatment (red), and postretention (green) cephalometric tracings.
Case 2
An 11-year-old prepubertal male in the late mixed dentition presented with the chief complaint of crooked teeth (Fig. 5A). The patient had a Class II malocclusion due to a retrognathic mandible and a bilateral end-on molar relationship, with minimal crowding in both arches.

Fig. 5 Case 2. A. 11-year-old male patient with Class II malocclusion, minimal upper and lower crowding, 5mm overjet, and deep bite before treatment. B. Patient after three months of treatment with TFBC and stiff upper and lower archwires and total 24 months of treatment. (continued in next image)
With 5mm of overjet, he had a 50% deep bite. After initial leveling and alignment, the deciduous upper left second molar was extracted, and the second premolar was exposed and brought into the arch. Stiff upper and lower archwires were then placed in conjunction with the TFBC for three months to achieve over corrected Class I molar and canine relationships. The case was debonded with stable Class I molar and canine relationships (Fig. 5B). Cephalometrically, the patient showed mild restriction of maxillary growth and redirection of mandibular growth (Table 2). A six-year retention evaluation demonstrated stable Class I molar and canine relationships, with good intercuspation of the buccal segments (Fig. 5C,D). A mild relapse of the midline diastema was noted, and the patient's upper and lower incisors were more proclined at the retention review compared to the post-treatment values.
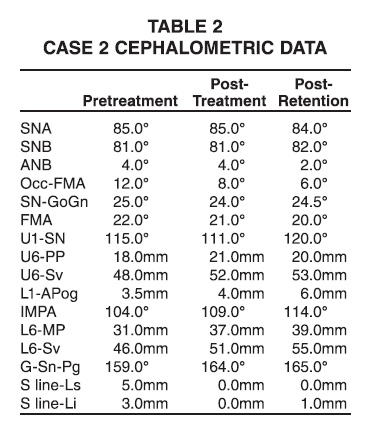
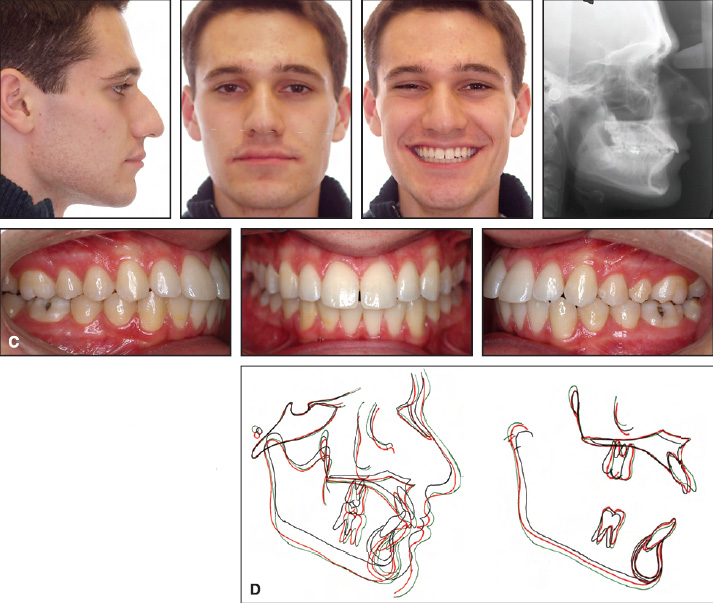
Fig. 5 Case 2 (cont.) C. Mild relapse of midline diastema seen at sixyear post-retention examination. D. Superimposition of pretreatment (black), post-treatment (red), and post-retention (green) cephalometric tracings.
Case 3
An 11-year-old female presented with the chief complaint of crowding (Fig. 6A). Initial examination revealed a Class II, division 1 malocclusion due to a combination of a prognathic maxilla and a retrognathic mandible, with Class II molar and canine relationships on both sides. An ANB measurement of 11.5º was combined with an overjet of 7mm, a 70% overbite, and a bilateral molar crossbite.
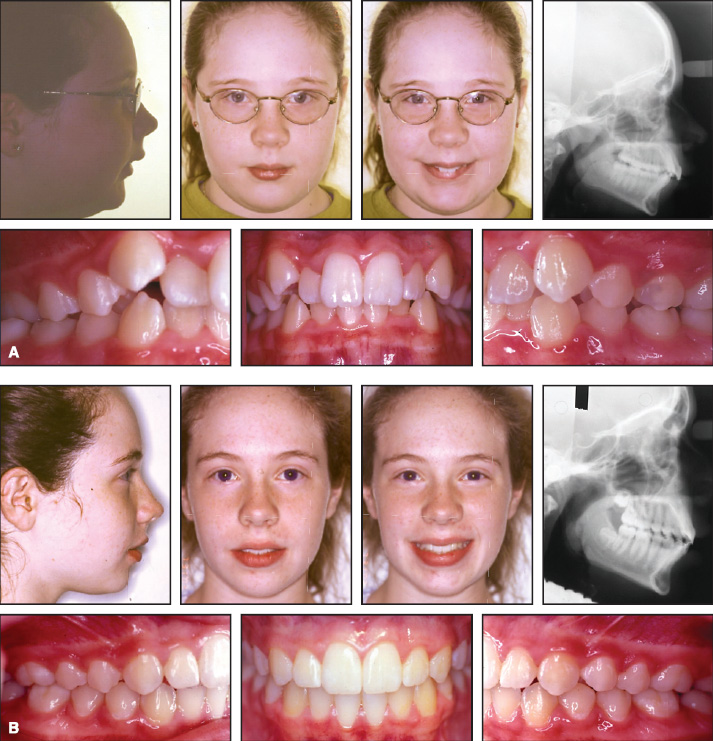
Fig. 6 Case 3. A. 11-year-old female patient wit Class II, division 1 malocclusion, 7mm overjet, deep overbite, and bilateral molar crossbite before treatment. B. Patient after 24 months of treatment.
Treatment began with rapid maxillary expansion to correct the crossbite. Fixed appliances were then bonded, and leveling and alignment were initiated to set up the upper and lower arches for TFBC placement. After 24 months of active treatment, the patient showed bilateral Class I molar and canine relationships (Fig. 6B). At the follow-up examination after seven years of retention, she displayed a harmonious soft-tissue profile with a stable buccal occlusion (Fig. 6C,D). Cephalometric analysis indicated a mild relapse of the dental compensations achieved by the TFBC (Table 3).
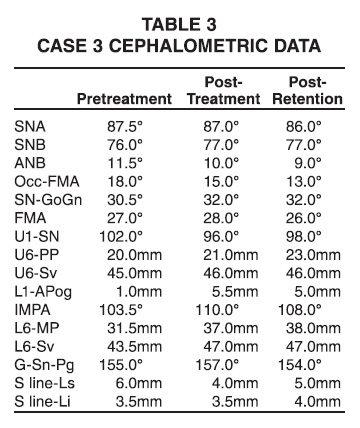
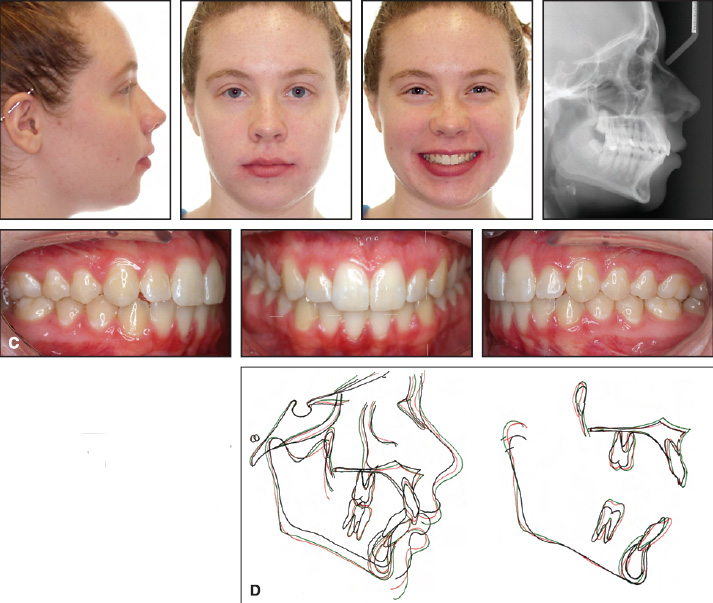
Fig. 6 Case 3 (cont.) C. Patient after seven years of retention. D. Superimposition of pretreatment (black), post-treatment (red), and postretention (green) cephalometric tracings.
Case 4
A 9-year-old female presented with the chief complaint of crowding (Fig. 7A). The patient was in the mixed dentition, with a Class II malocclusion and an end-on molar relationship. She had an overjet of 3mm, an overbite of 30%, and a convex soft-tissue profile.
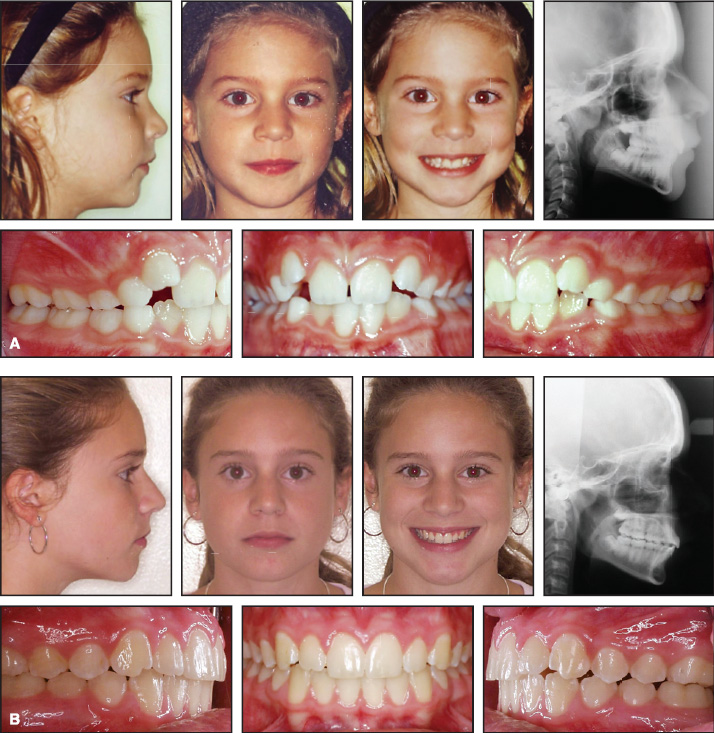
Fig. 7 Case 4. A. 9-year-old female patient with crowded Class II malocclusion, 3mm overjet, and 30% overbite before treatment. B. Patient after 28 months of treatment, including three months of TFBC wear. (continued in next image)
Although the paitent was initially given a cervical headgear to distalize the molars, she did not cooperate with the headgear wear. Once the deciduous teeth had exfoliated, the upper and lower arches were leveled and aligned. A TFBC with 4mm of activation was attached to stiff upper .019'' x .025'' and lower .021'' x .025'' stainless steel archwires. Three months later, a mild Class III molar relationship had been obtained, and the TFBC was removed for finishing and detailing (Fig. 7B). Cephalometric analysis showed a mild distalizing effect on the maxilla and forward growth of the mandible, along with proclination of the lower incisors (Table 4). Six years into retention, the lower arch had continued its favorable growth, further reducing the ANB angle. The patient showed mild relapse of the crowding in the upper right lateral incisor region, but maintained the buccal occlusion and soft-tissue profile improvement (Fig. 7C,D).
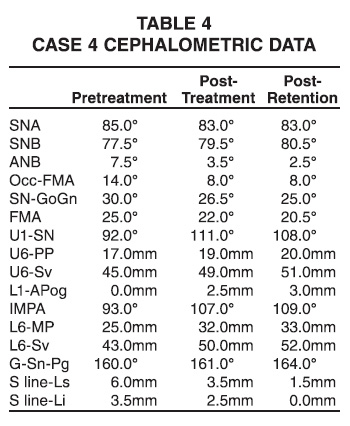
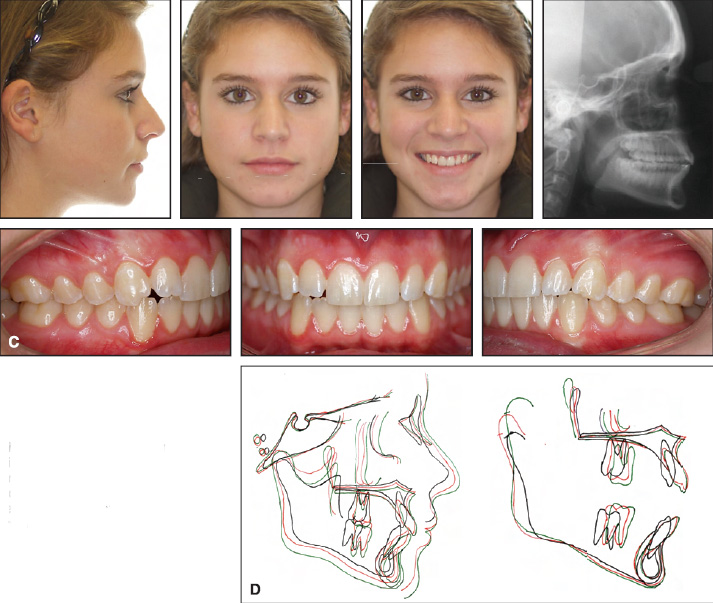
Fig. 7 Case 4 (cont.) C. Patient after six years of retention. D. Superimposition of pretreatment (black), post-treatment (red), and post-retention (green) cephalometric tracings.
Case 5
An 11-year-old prepubertal male patient, primarily concerned about his excessive overjet, presented with a Class II malocclusion due to a retrognathic mandible (Fig. 8A).

Fig. 8 Case 5. A. 11-year-old male Class II patient with fingersucking habit, posterior crossbite, and 7mm overjet. B. Patient after 30 months of treatment (continued in next image).
The patient had a fingersucking habit, and the posterior teeth were in crossbite, while the anterior teeth showed mild crowding and an overjet of 7mm. Once the fingersucking habit was controlled, fixed appliances were bonded, and a rapid maxillary expansion appliance was placed to correct the posterior crossbite. After 5mm of expansion had been achieved, a TFBC was attched to a stiff .019'' x .025'' stainless steel archwire in the upper arch and an .021'' x .025'' stainless steel wire in the lower arch. The patient was debonded after 30 months of active treatment with Class I molar and canine relationships and an improved soft-tissue profile (Fig. 8B). Five years later, the post-treatment results had been maintained (Fig. 8C,D, Table 5).
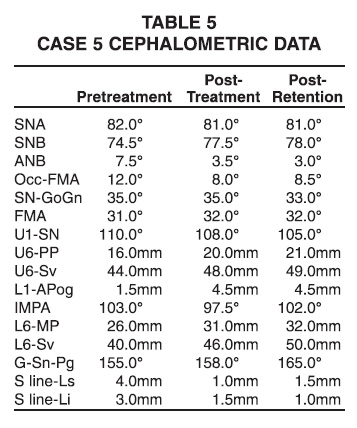
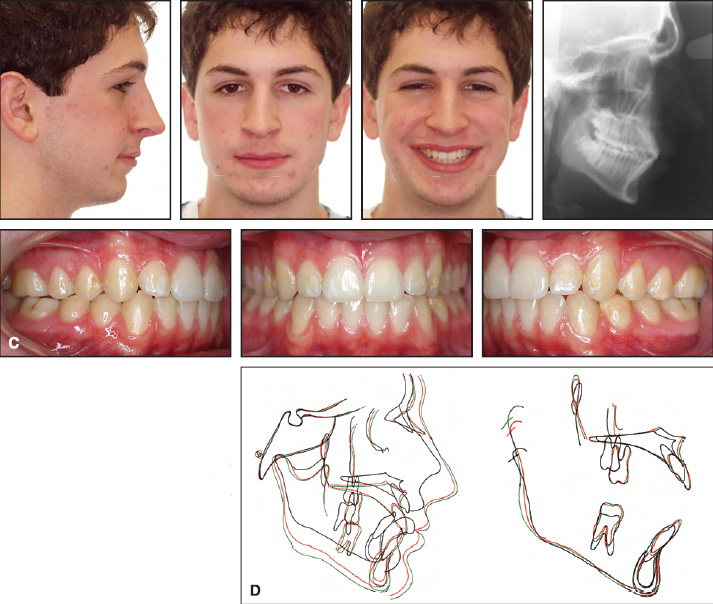
Fig. 8 Case 5 (cont.) C. Patient after five years of retention. D. Superimposition of pretreatment (black), post-treatment (red), and post-retention (green) cephalometric tracings.
Discussion
All these patients showed stable post-treatment occlusions and harmonious soft-tissue profiles, as reported for two of the cases in a previous article.2 Cephalometric superimpositions demonstrated improvements in both the skeletal and soft-tissue parameters.
Establishment of an ideal occlusion and a beautiful smile with minimal detrimental effects are among the primary goals of orthodontic treatment. Follow-up studies of Class II patients have shown a tendency to return to the original malocclusion after treatment. Madone and Ingervall found small increases in overjet and overbite and partial relapse of the molar relationships.3 Uhde and colleagues4 and Hellekant and colleagues5 have also reported minor relapse of molar relationships and overjet in treated cases.
Proper interdigitation of the posterior occlusion after bracket removal appears to be an important contributor to the stability of the correction.6-8 Significant amounts of relapse were observed by Pancherz9 and Wieslander10 in cases treated to unstable occlusal relationships.
The cases in this report are part of a longterm prospective study.1 To date, 50 Class II patients have been treated with the TFBC, and their results are being evaluated two to seven years after treatment. Of the 22 patients evaluated thus far during the retention period, 20 have shown stable relationships or improved settling of the occlusion, lending credibility to the TFBC as an effective appliance for stable Class II correction.
FOOTNOTES
- *Registered trademark of Ortho Organizers, 1822 Aston Ave., Carlsbad, CA 92008; www.orthoorganizers.com.
REFERENCES
- 1. Campbell, E.: A prospective clinical analysis of a push-type fixed intermaxillary Class II correction appliance, thesis, University of Connecticut, Farmington, 2003.
- 2. Rothenberg, J.; Campbell, E.S.; and Nanda, R.: Class II correction with the Twin Force Bite Corrector, J. Clin. Orthod. 38:232-240, 2004.
- 3. Madone, G. and Ingervall, B.: Stability of results and function of the masticatory system in patients treated with the Herren type of activator, Eur. J. Orthod. 6:92-106, 1984.
- 4. Uhde, M.D.; Sadowsky, C.; and BeGole, E.A.: Long-term stability of dental relationships after orthodontic treatment, Angle Orthod. 53:240-252, 1983.
- 5. Hellekant, M.; Lagerström, L.; and Gleerup, A.: Overbite and overjet correction in a Class II, division 1 sample treated with Edgewise therapy, Eur. J. Orthod. 11:91-106, 1989.
- 6. Lavergne, J. and Petrovic, A.: Discontinuities in occlusal relationship and the regulation of facial growth. A cybernetic view, Eur. J. Orthod. 5:269-278, 1983.
- 7. Boley, J.C.; Mark, J.A.; Sachdeva, R.C.; and Buschang, P.H.: Long-term stability of Class I premolar extraction treatment, Am. J. Orthod. 124:277-287, 2003.
- 8. Elms, T.N.; Buschang, P.H.; and Alexander, R.G.: Long-term stability of Class II, Division 1 nonextraction cervical facebow therapy: I. Model analysis, Am. J. Orthod. 109:271-276, 1996.
- 9. Pancherz, H.: The Herbst appliance--its biological effects and clinical use, Am. J. Orthod. 87:1-20, 1985.
- 10. Wieslander, L.: Intensive treatment of severe Class II malocclusions with a headgear-Herbst appliance in the early mixed dentition, Am. J. Orthod. 86:1-13, 1984.





