Class II Correction with the Twin Force Bite Corrector
Molar distalization in Class II cases has been accomplished with various functional appliances, including fixed interarch appliances, such as the Herbst* and Jasper Jumper**, and fixed intra-arch appliances. The Twin Force Bite Corrector (TFBC)*** is a new fixed intermaxillary appliance with a built-in constant force for Class II correction.
This article presents two patients who were part of a long-term prospective study currently in progress at the University of Connecticut Department of Orthodontics. Each patient was treated with the TFBC to correct a skeletal Class II malocclusion due to a retrognathic mandible.
Appliance Design
Similar articles from the archive:
The TFBC is a fixed, push-type intermaxillary functional appliance with ball-and-socket joint fasteners that allow a wide range of motion and lateral jaw movement (Fig. 1). The two plunger/tube telescopic assemblies on each side contain nickel titanium coil springs that deliver a constant force. Measuring several appliances with a force gauge demonstrated an average full-compression force of approximately 210g.
The appliance is attached to the maxillary and mandibular archwires by hex nuts fastened mesial to the maxillary first molars and distal to the mandibular canines. At full compression, the TFBC postures the patient's mandible forward into an edge-to-edge occlusion.
Case Reports
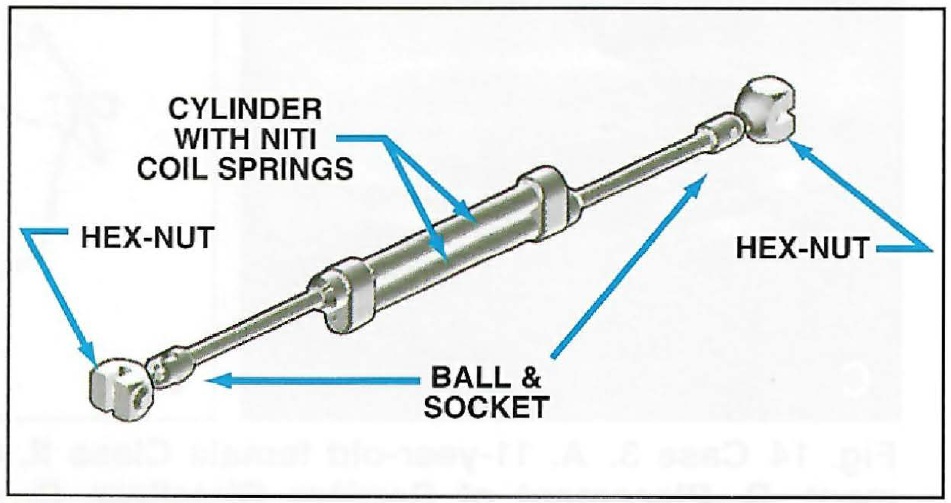
Fig. 1 Twin Force Bite Corrector (TFBC) in open
position.
Case 1, a 12-year-old prepubertal male, presented with the chief complaint of a deep bite. The diagnosis was a Class II malocclusion due to a retrognathic mandible, with an overbite of 100%, an overjet of 6mm, and a convex soft-tissue profile (Fig. 2). Crowding in both arches was mild. Pretreatment cephalometric analysis confirmed a Class II skeletal relationship (ANB = 4.5°, NAPg = 8.3°, AB(OP) = 1.9mm, AB(FH) = -13.7mm).
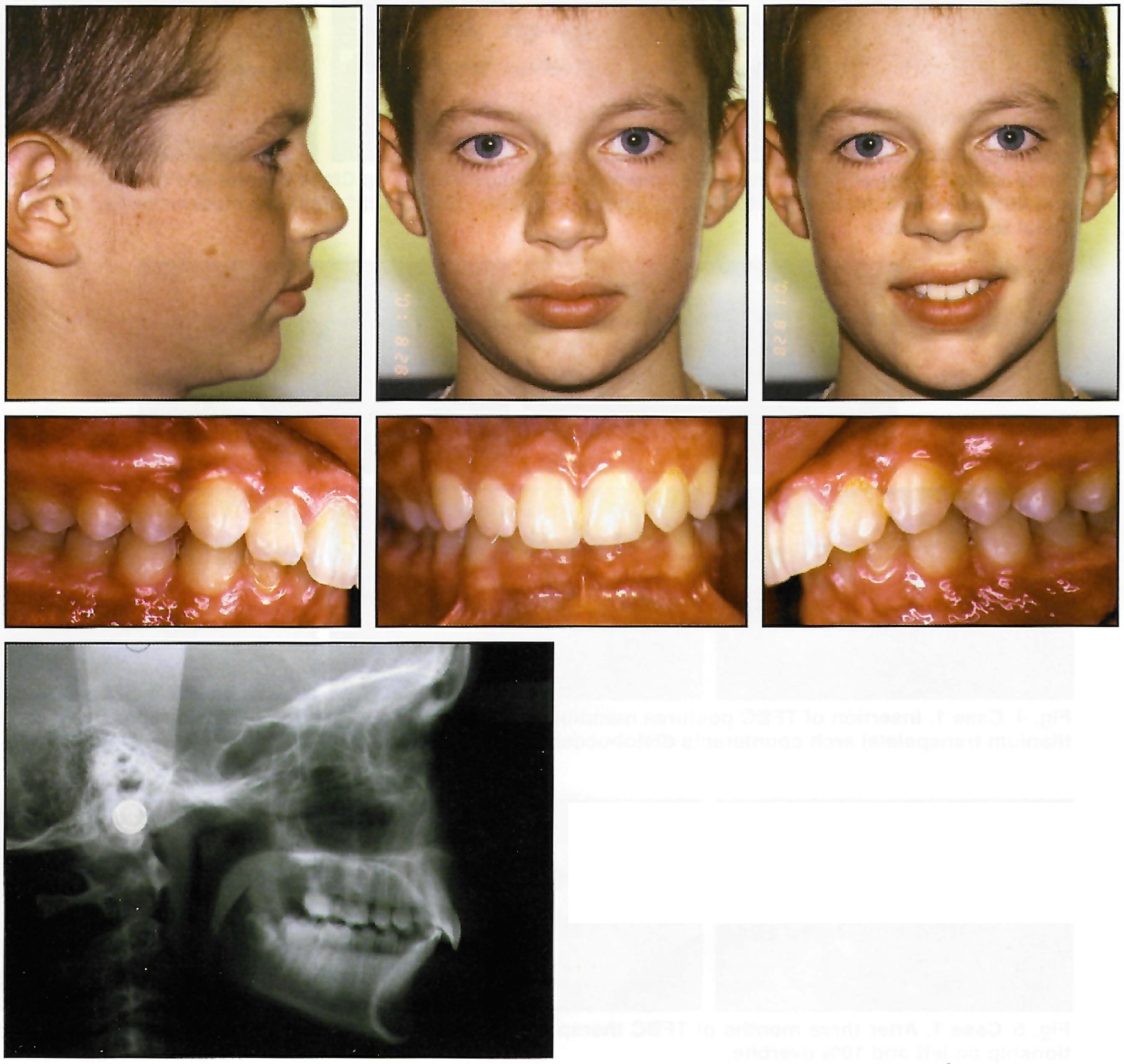
Fig. 2 Case 1. 12-year-old male patient with skeletal Class II malocclusion before treatment.
Case 2, an 11-year-old male, was also classified as a skeletal Class II due to a retrognathic mandible (Fig. 8). Excessive overbite and overjet were noted, along with mild crowding in both arches. Pretreatment cephalometric analysis also depicted a skeletal Class II relationship (ANB = 4.6°, NAPg = 9.5°, AB(OP) = 2.9mm, AB(FH) = -4.9mm).

Fig. 8 Case 2. 11-year-old male patient with end-on Class II molar relationship and excessive overjet before treatment.
The treatment objectives in both cases were to improve the skeletofacial and soft-tissue relationships by maximizing differential jaw and dentoalveolar changes, using a biomechanical force system with predictable side effects. Treatment began in each patient with banding of the maxillary molars, using palatal sheaths to allow future placement of transpalatal arches. The maxillary and mandibular arches were then bonded with .022" × .028" brackets (Nanda prescription***). Brackets with -6° torque were placed on the mandibular incisors to minimize proclination.
Alignment was carried out on light nickel titanium archwires. Wire sizes were progressively increased to .019" × .025" stainless steel in the maxillary arch and .021" × .025" stainless steel in the mandibular arch (Fig. 3, Fig. 9). The heavy stainless steel archwires were needed to avoid deflection after insertion of the TFBC. Both the maxillary and mandibular archwires were cinched distal to the first molars to prevent space opening and flaring, and to allow both arches to move as complete dental units.

Fig. 3 Case 1. After eight months of treatment, patient shows full-cusp Class II molar and canine relationships and 80% deep bite. Maxillary .019" × .025" and mandibular .021" × .025" stainless steel archwires are cinched distal to first molars.
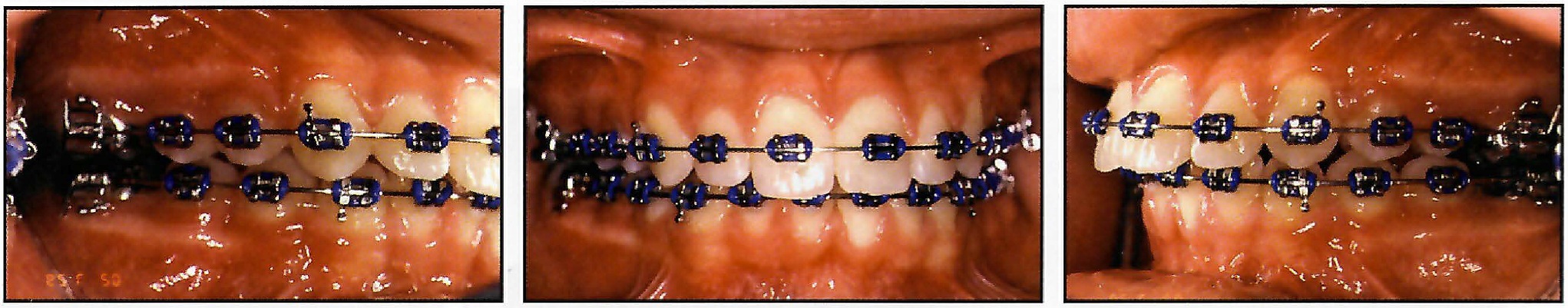
Fig. 9 Case 2. After 10 months of treatment, patient is end-on Class II subdivision left, with mandibular midline deviating to left. Maxillary .019" × .025" and mandibular .021" × .025" stainless steel archwires are cinched distal to first molars.
Upon appliance delivery, a passive .032" beta titanium transpalatal arch was inserted to counteract the buccal forces applied by the TFBC. The TFBC was attached to the archwires mesial to the maxillary first molars and distal to the mandibular canines, posturing the mandible forward into an edge-to-edge occlusion (Fig. 4, Fig. 10).
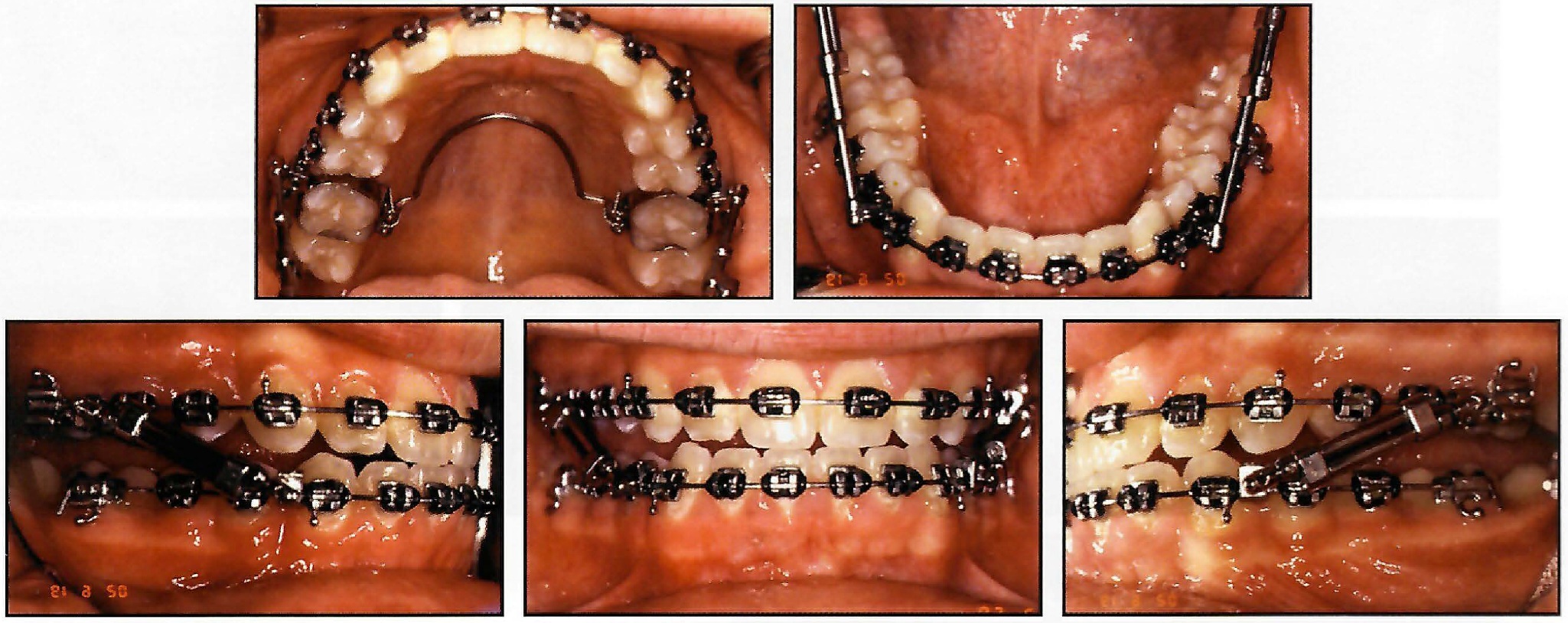
Fig. 4 Case 1. Insertion of TFBC postures mandible forward into edge-to-edge occlusion; passive .032" beta titanium transpalatal arch counteracts distobuccal forces of TFBC.
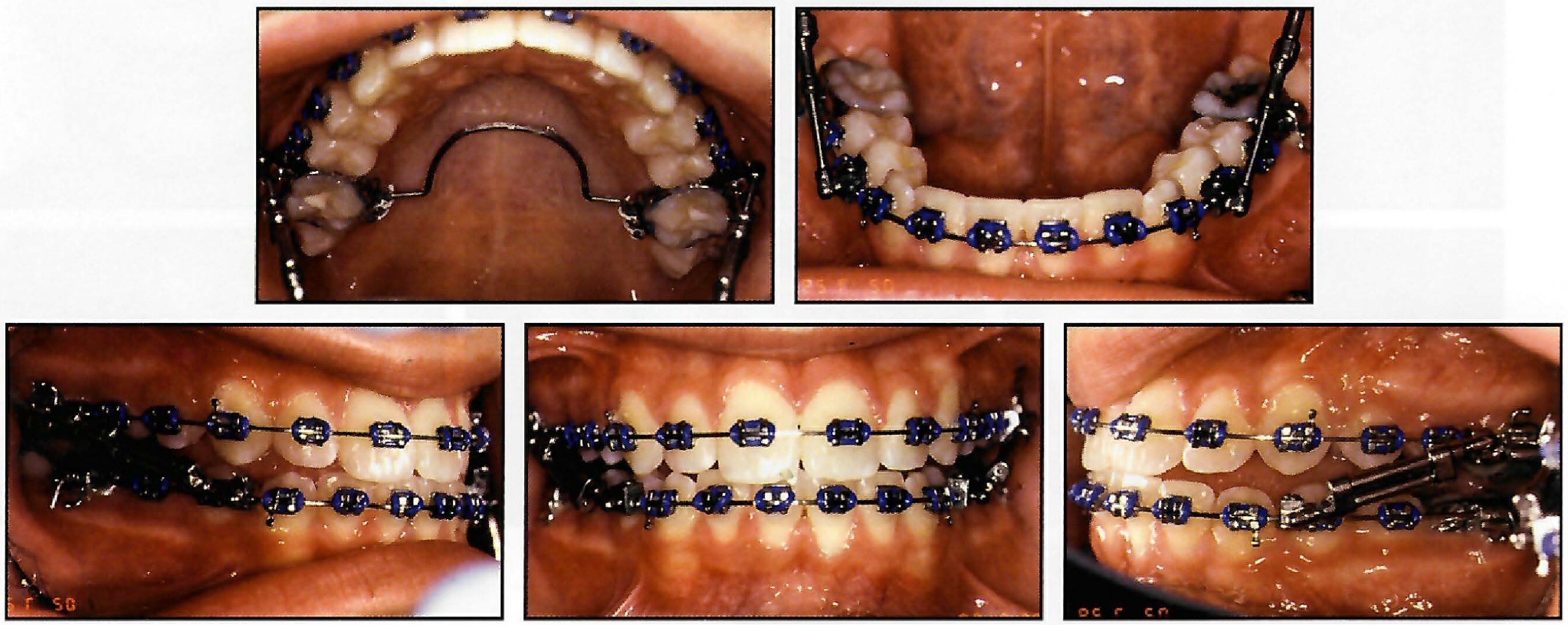
Fig. 10 Case 2. Insertion of TFBC postures mandible forward into edge-to-edge occlusion; passive .032" beta titanium transpalatal arch counteracts distobuccal forces of TFBC.
At each monthly visit, the appliance was removed from the mandibular attachments on both sides by loosening the hex nuts. A centric relation registration was then taken. After three months, each patient showed a Class I molar relationship. The TFBC and the transpalatal arch were then removed (Fig. 5, Fig. 11).
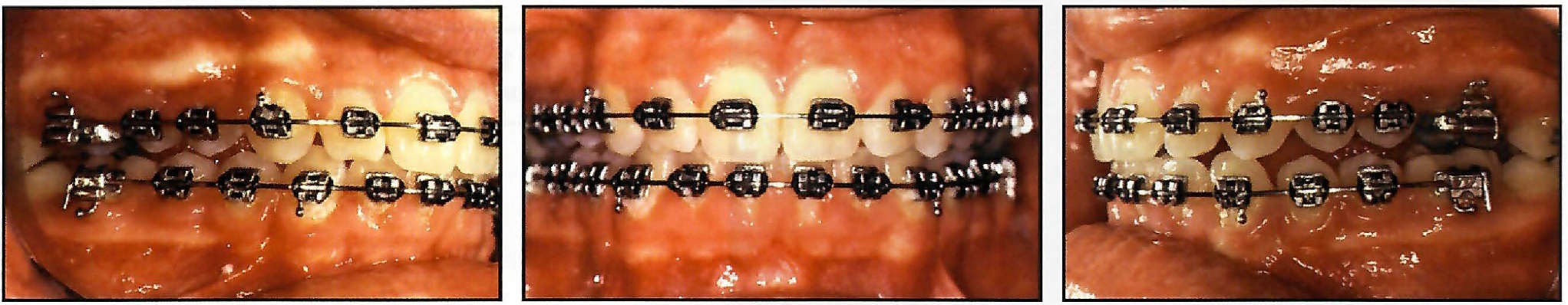
Fig. 5 Case 1. After three months of TFBC therapy, patient is Class I on right side, with slight Class II relationship on left and 10% overbite.

Fig. 11 Case 2. After three months of TFBC therapy, patient shows super-Class I molar relationships and coincident midlines.
A new .017" × .025" stainless steel mandibular archwire was placed, and the patient was instructed to wear 3.5oz intermaxillary elastics from the maxillary canines and first premolars to the mandibular first and second premolars. The elastics, worn for three months, had Class II vectors to maintain the correction and allow the posterior occlusion to settle. After finishing, the brackets were debonded, and a maxillary wraparound Hawley retainer and mandibular 3-3 bonded lingual .0175" braided-wire retainer were placed.
A functional Class I occlusion was obtained in both patients, with ideal overbite and overjet (Fig. 6, Fig. 12). The coincident midlines were maintained, and both skeletal and soft-tissue discrepancies were improved. Most important, both patients' chief complaints were corrected, and our primary treatment objectives were met.

Fig. 6 Case 1. After 23 months of treatment, note improved soft-tissue profile, Class I molar and canine relationships, coincident midlines, and ideal overbite.
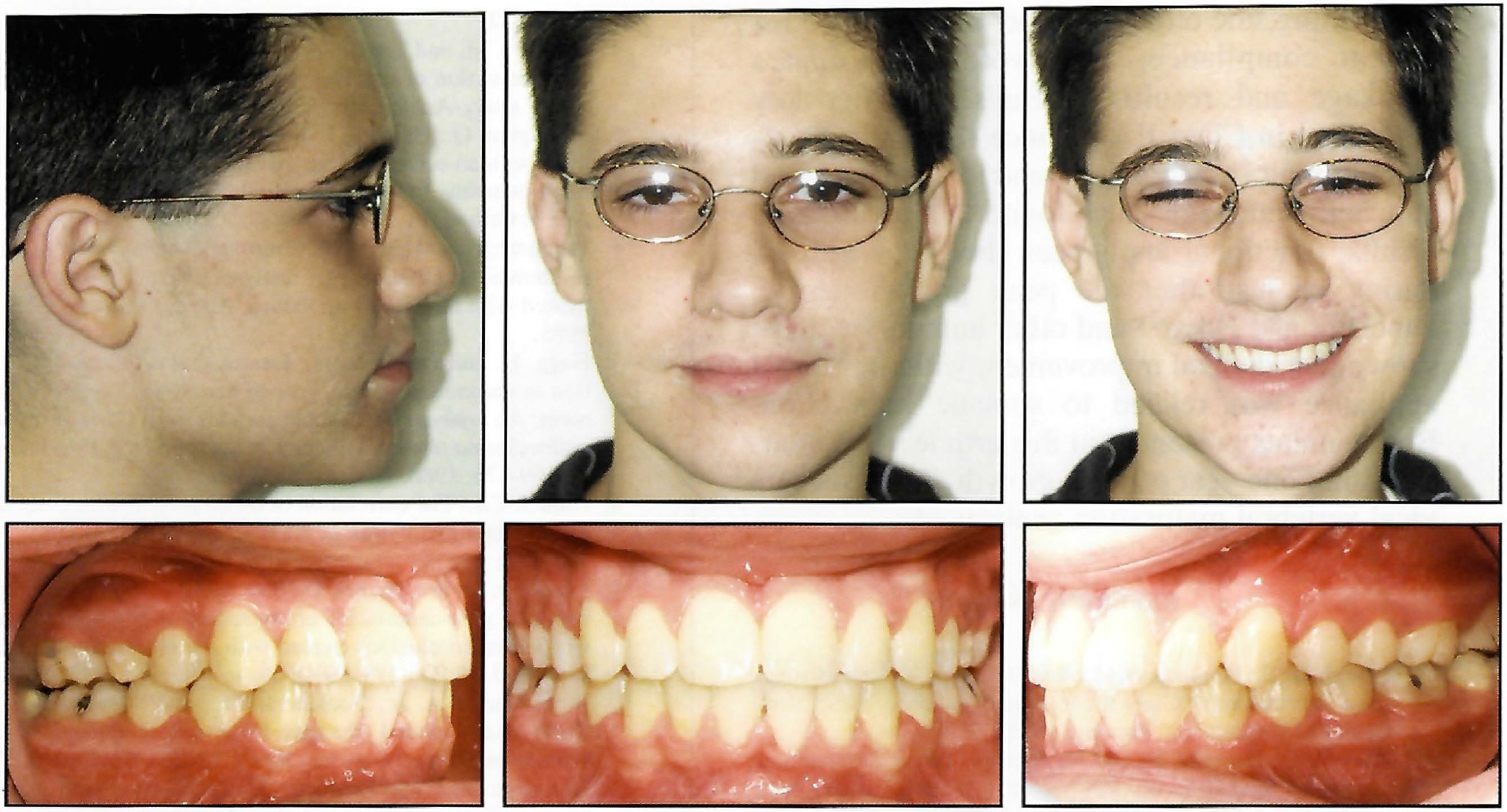
Fig. 12 Case 2. After 24 months of treatment, note orthognathic soft-tissue profile, Class I molar and canine relationships, coincident midlines, and ideal overbite.
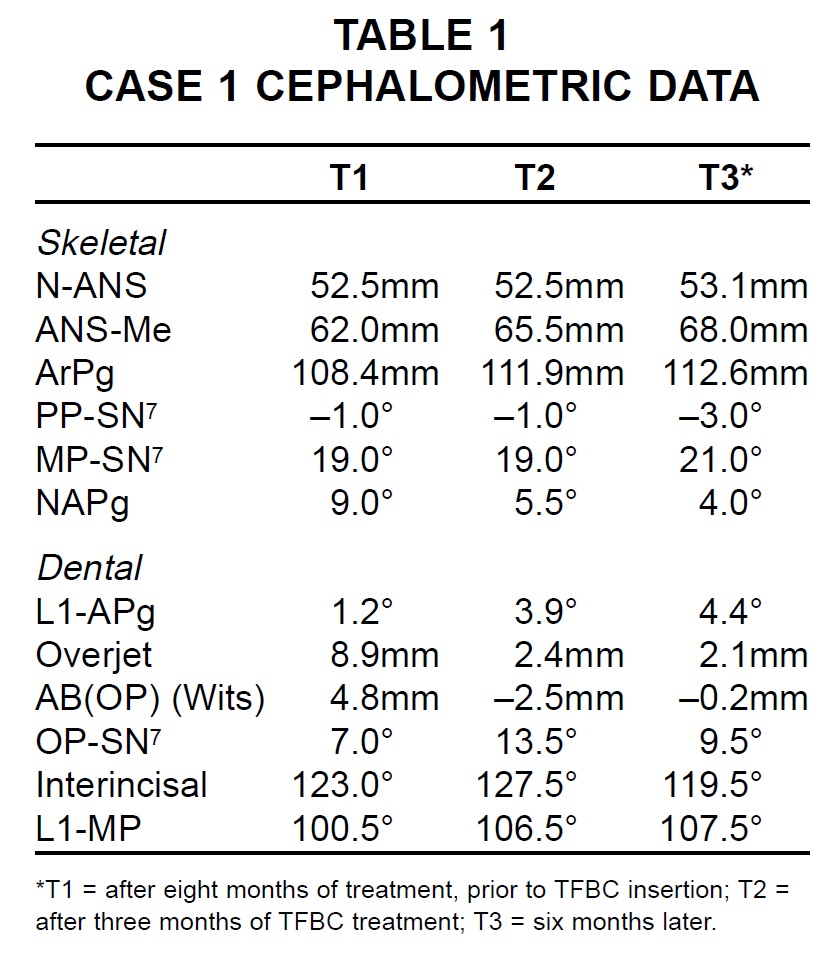
Total treatment duration for Case 1 was 23 months. Superimpositions of the cephalometric tracings showed skeletal changes, with overjet reduced from 8.9mm to 2.1mm and the angle of convexity improved from 9.0° to 4.0° (Fig. 7; [table=1]Table 1[/img]).
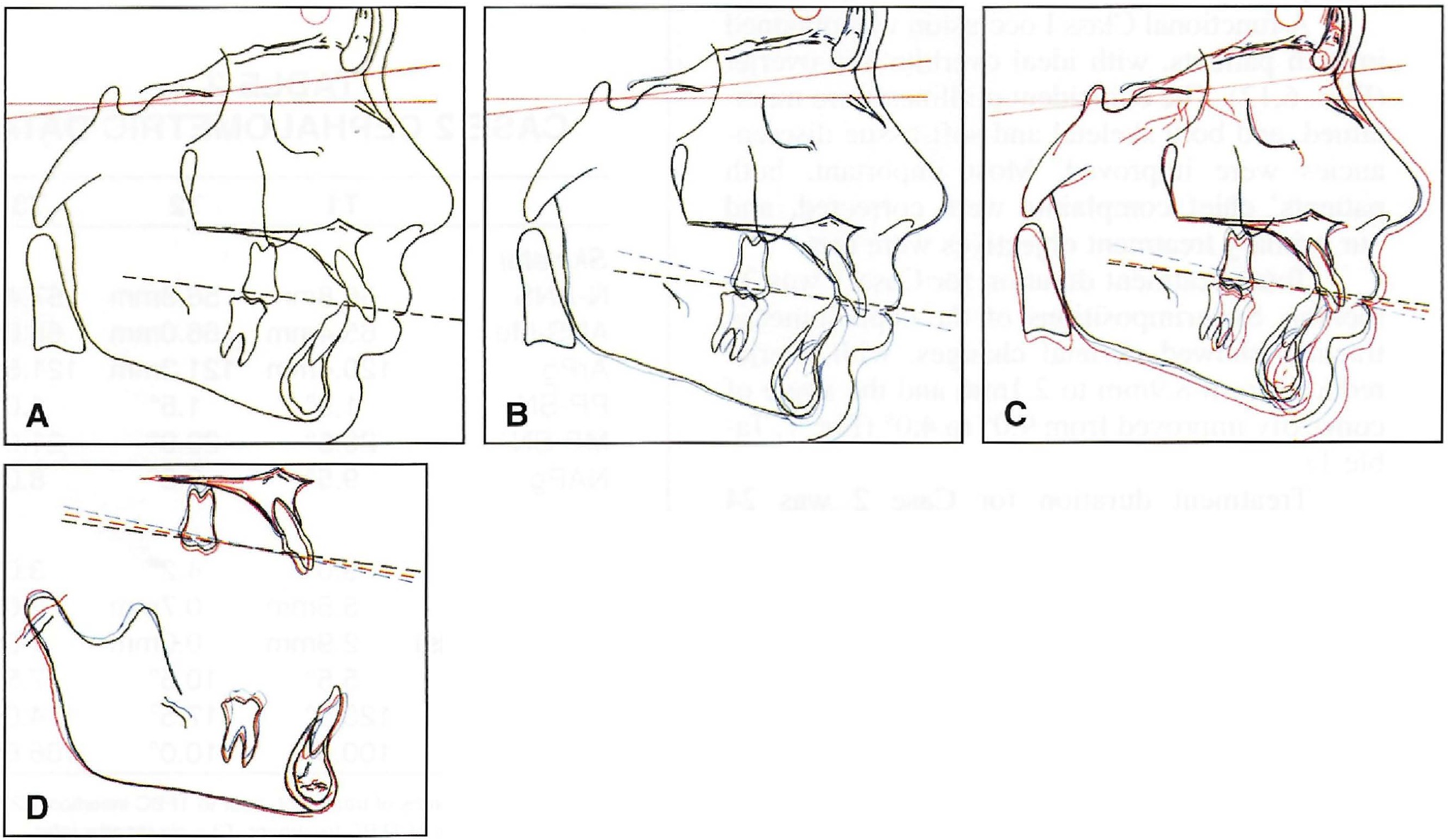
Fig. 7 Case 1. Cephalometric tracings and superimpositions. A. T1 (black), prior to TFBC insertion. B. Superimposition of T2 (blue), after TFBC removal. C. Superimposition of T3 (red), six months later. D. Maxillary and mandibular superimpositions. Note canting of occlusal plane between T1 and T2, with slight relapse at T3. Also note maxillary incisor retraction and mandibular molar advancement and incisor proclination. Growth is shown at articulare, with greatest amount occurring between T1 and T2.
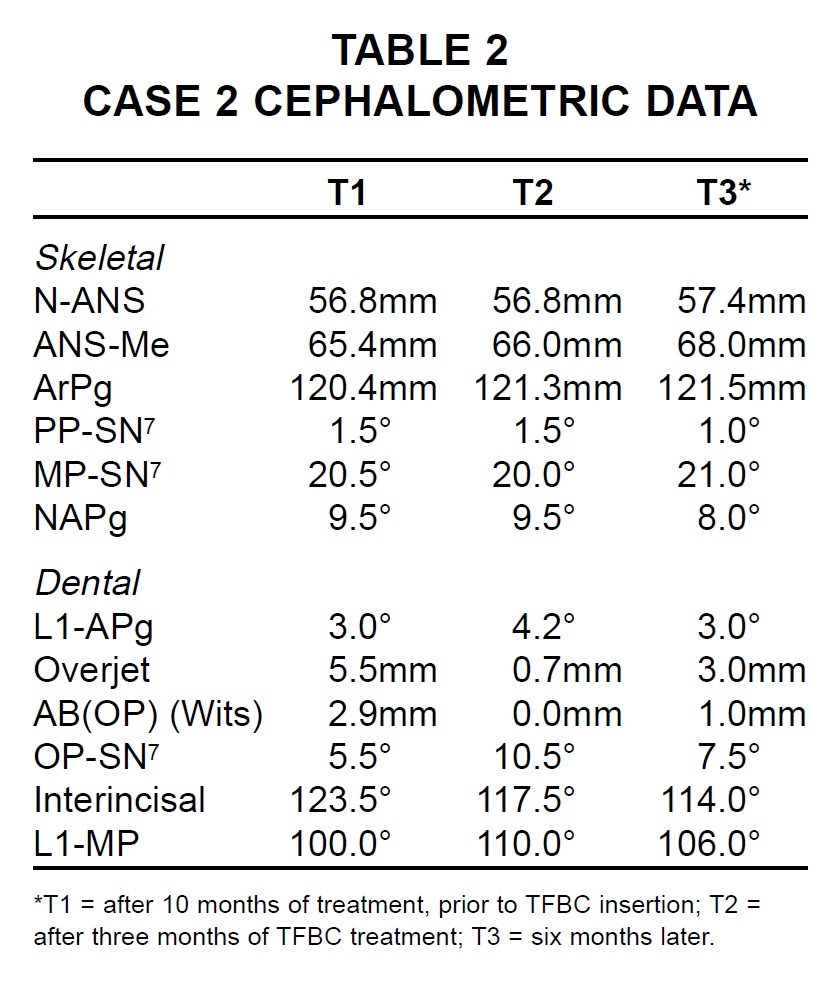
Treatment duration for Case 2 was 24 months. Most of the correction was dentoalveolar; the vertical dimension did not increase appreciably, and the mandibular plane angle remained unchanged (Fig. 13; [table=2]Table 2[/img]).). The angle of convexity and AB(OP) were favorably reduced, and the changes noted at T2 settled during the finishing period.
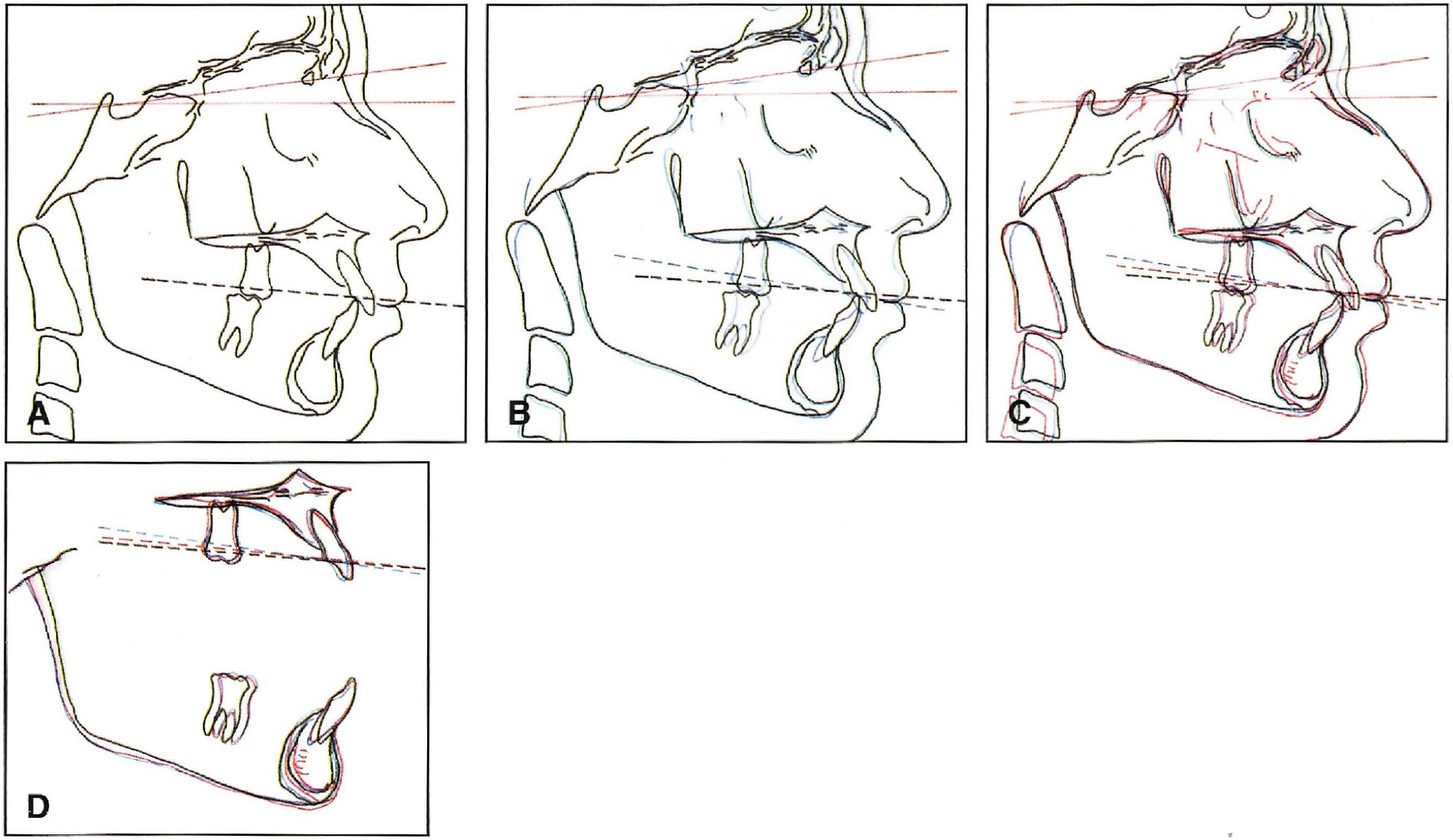
Fig. 13 Case 2. Cephalometric tracings and superimpositions. A. T1 (black), prior to TFBC insertion. B. Superimposition of T2 (blue), after TFBC removal. C. Superimposition of T3 (red), six months later. D. Maxillary and mandibular superimpositions. Note canting of occlusal plane between T1 and T2, with slight relapse at T3. Also note maxillary incisor retraction and mandibular molar advancement and incisor proclination.
Both patients exhibited similar dental results, with an improvement in the molar and canine relationships, a reduction in overjet, an increase in mandibular incisor proclination, and steepening of the occlusal plane. Skeletal changes for both patients resulted in a decrease in AB(OP) and NAPg. Both patients also exhibited soft-tissue improvements, including an increased incisor display at rest. The changes remained stable for at least six months after appliance removal and have been maintained during retention.
Discussion
Campbell first used the TFBC in a prospective longitudinal study at the University of Connecticut Department of Orthodontics.1 The skeletal and dentoalveolar changes of 22 patients were compared to skeletally age-matched controls from the Denver Growth Study. Results included decreases in ANB, NAPg, AB(OP), AB(FH), and overjet. Occlusal plane measurements were derived from the height of the maxillary first molar buccal tubes and the premolar brackets.
The keys to success in Class II treatment are limiting side effects, minimizing the need for patient compliance, and avoiding appliance breakage and resulting delays. Another key ingredient in Class II appliance therapy is treatment timing.2-4 Malmgren and colleagues5 and Pancherz and Hagg6 have found that for optimal results, functional appliances should be utilized during or just after the peak growth period. Pancherz and Hagg6,7 and other authors4,8-12 have shown that skeletal improvement with the Herbst appliance was related to somatic maturation. Both patients presented in this article were treated within one year of peak growth, based on cervical vertebral maturation analysis.2-4
FOOTNOTES
- *Trademark of Dentaurum, Inc., 10 Pheasant Run, Newtown, PA 18940.
- **American Orthodontics, 1714 Cambridge Ave., Sheboygan, WI 53082.
- ***Ortho Organizers, Inc., 1619 S. Rancho Santa Fe Road, San Marcos, CA 92069. Twin Force Bite Corrector is a trademark.
REFERENCES
- 1. Campbell, E.: A prospective clinical analysis of a push-type fixed intermaxillary Class II correction appliance, thesis, University of Connecticut, Farmington, 2003.
- 2. Franchi, L.; Baccetti, T.; and McNamara, J.A. Jr.: Mandibular growth as related to cervical vertebral maturation and body height, Am. J. Orthod. 118:335-340, 2000.
- 3. Baccetti, T.; Franchi, L.; and McNamara, J.A. Jr.: An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth, Angle Orthod. 72:316-323, 2002.
- 4. O'Reilly, M. and Yanniello, G.J.: Mandibular growth changes and maturation of cervical vertebrae: A longitudinal cephalometric study, Angle Orthod. 58:179-184, 1988.
- 5. Malmgren, O.; Omblus, J.; Hagg, U.; and Pancherz, H.: Treatment with an orthopedic appliance system in relation to treatment intensity and growth periods: A study of initial effects, Am. J. Orthod. 91:143-151, 1987.
- 6. Pancherz, H. and Hagg, U.: Dentofacial orthopedics in relation to somatic maturation: An analysis of 70 consecutive cases treated with the Herbst appliance, Am. J. Orthod. 88:273-297, 1985.
- 7. Hagg, U. and Pancherz, H.: Dentofacial orthopaedics in relation to chronological age, growth period and skeletal development: An analysis of 72 male patients with Class II division I malocclusion treated with the Herbst appliance, Eur. J. Orthod. 10:169-176, 1988.
- 8. Hunter, C.J.: The correlation of facial growth with body height and skeletal maturation at adolescence, Angle Orthod. 36:44-54, 1966.
- 9. Pancherz, H. and Fackel, U.: The skeletofacial growth pattern pre- and post-dentofacial orthopaedics: A long-term study of Class II malocclusions treated with the Herbst appliance, Eur. J. Orthod. 12:209-218, 1990.
- 10. McNamara, J.A. Jr.; Bookstein, F.L.; and Shaughnessy, T.G.: Skeletal and dental changes following functional regulator therapy on Class II patients, Am. J. Orthod. 88:91-110, 1985.
- 11. Von Bremen, J. and Pancherz, H.: Efficiency of early and late Class II division I treatment, Am. J. Orthod. 121:31-37, 2002.
- 12. Baccetti, T.; Franchi, L.; Toth, L.R.; and McNamara, J.A. Jr.: Treatment timing for Twin-block therapy, Am. J. Orthod. 118:159-170, 2000.




