A New Non-Surgical Approach for Extreme Dolichocephalic Malocclusions, Part 2: Case Selection and Management
The two most important aspects of orthodontic treatment to patients are probably esthetics and speed. Lingual brackets and clear brackets have helped with the esthetic demands, but some patients want even less visible treatment modalities. And while new wire and bracket technologies have reduced treatment times, many patients would like to have treatment be faster yet.
During the past few years, two techniques have been introduced that promise to address both these concerns. This article will report on a treatment approach combining the two.
Periodontal-Surgical Treatment
Corticotomy-assisted orthodontics was developed to increase the rate of tooth movement and thus reduce treatment time.1-7 The original procedure, involving single-tooth osteotomies or corticotomies, was introduced by Kole in 1959.1 It was thought the teeth moved faster because the resistance of the cortical bone was reduced by the surgical procedure. Frost found that surgical healing occurred mainly as reorganizing activity and accelerated bone turnover at the surgical site; he called this "regional accelerated phenomenon" (RAP).4,5 RAP is essentially a temporary burst of localized soft- and hard-tissue remodeling to rebuild the surgical site to a normal state.6
Similar articles from the archive:
Drs. Thomas and William Wilcko, using computed tomography, discovered that rapid tooth movement following corticotomies was due to reduced mineralization of the alveolar bone housing the involved teeth.8 Two-year follow-up CT scans revealed that the alveolar bone had adequately remineralized. The patients had experienced virtually no root resorption, no loss of vitality, no loss of alveolar bone, and no periodontal pocketing.
It became apparent to the Wilckos that their patients could benefit from alveolar augmentation in conjunction with a decorticating procedure.9-14 The augmentation would not only improve the alveolar crestal height, but could also increase the thickness of alveolar bone and reduce dehiscences and fenestrations. Where crowding of the teeth had compromised the labial alveolar bone, the augmentation might make the alveolar bone healthier.
The technique developed by the Wilckos, called the Wilckodontics* system or Accelerated Osteogenic Orthodontics* (AOO), is similar to a single-tooth corticotomy, except that it is extended to all the teeth to be moved during orthodontic treatment.8 The procedure begins with comprehensive fixed orthodontic treatment, followed by a full-thickness flap, then decortication of the alveolar bone housing the teeth to be moved. A resorbable bone-graft augmentation is placed over the surgical site, and the soft-tissue flap is closed. Following the surgical procedure, orthodontic adjustments are made weekly to take advantage of the RAP, which lasts only three or four months. The rate of tooth movement then returns to normal once the bone has sufficiently healed.
Invisalign Therapy
I hypothesized that the Invisalign** approach to tooth movement could be utilized during this window of accelerated tooth movement. The Invisalign system is a series of clear removable appliances, similar to the clear plastic retainers that have been described by many authors.15-18 Although these plastic retainers have been modified to effect minor tooth movements, full orthodontic treatment remained impractical because of the problem cited by Kesling in 1945: the prohibitive labor costs involved in making the setups.19 It was not until the advent of modern computerization that full treatment became realistic.
In the Invisalign system, if a case is suitable for treatment, the casts are scanned, a three-dimensional model is created, and the computer performs virtual treatment using CAD-CAM technology. The clinician accesses this treatment plan over the Internet and modifies it until it is acceptable. In essence, Invisalign is like doing a setup on a computer.
Align Technology fabricates a series of the clear plastic retainers, or "aligners", that sequentially move the teeth at a rate of .25-.33mm every 14 days. The aligners should be worn at least 20 hours per day, but are taken out for meals and for brushing and flossing. The number of aligners needed for a particular case depends on the extent of tooth movement required. I have found that the length of treatment with the Invisalign approach is similar to that with fixed appliances.
Self-Treatment
Having taken both the Wilckodontics and Invisalign seminars, the possibility of combining the two approaches intrigued me. I could not prescribe this combination treatment for my patients, however, until it had proven safe and effective. Having experienced increased crowding that made it difficult to maintain proper oral hygiene, I decided to treat myself using both techniques simultaneously.
Before treatment, I had a good Class I occlusion and an acceptable overbite and overjet, but I had minor crowding, especially of the mandibular arch, along with a midline shift and a maxillary left lateral incisor rotation (Fig. 1). Align Technology projected my treatment to last 14 months if the aligners were changed as usual, every two weeks. Knowing that I had only three to four months to complete the treatment, I decided (with the company's acquiescence) that I should change the aligners every three days.
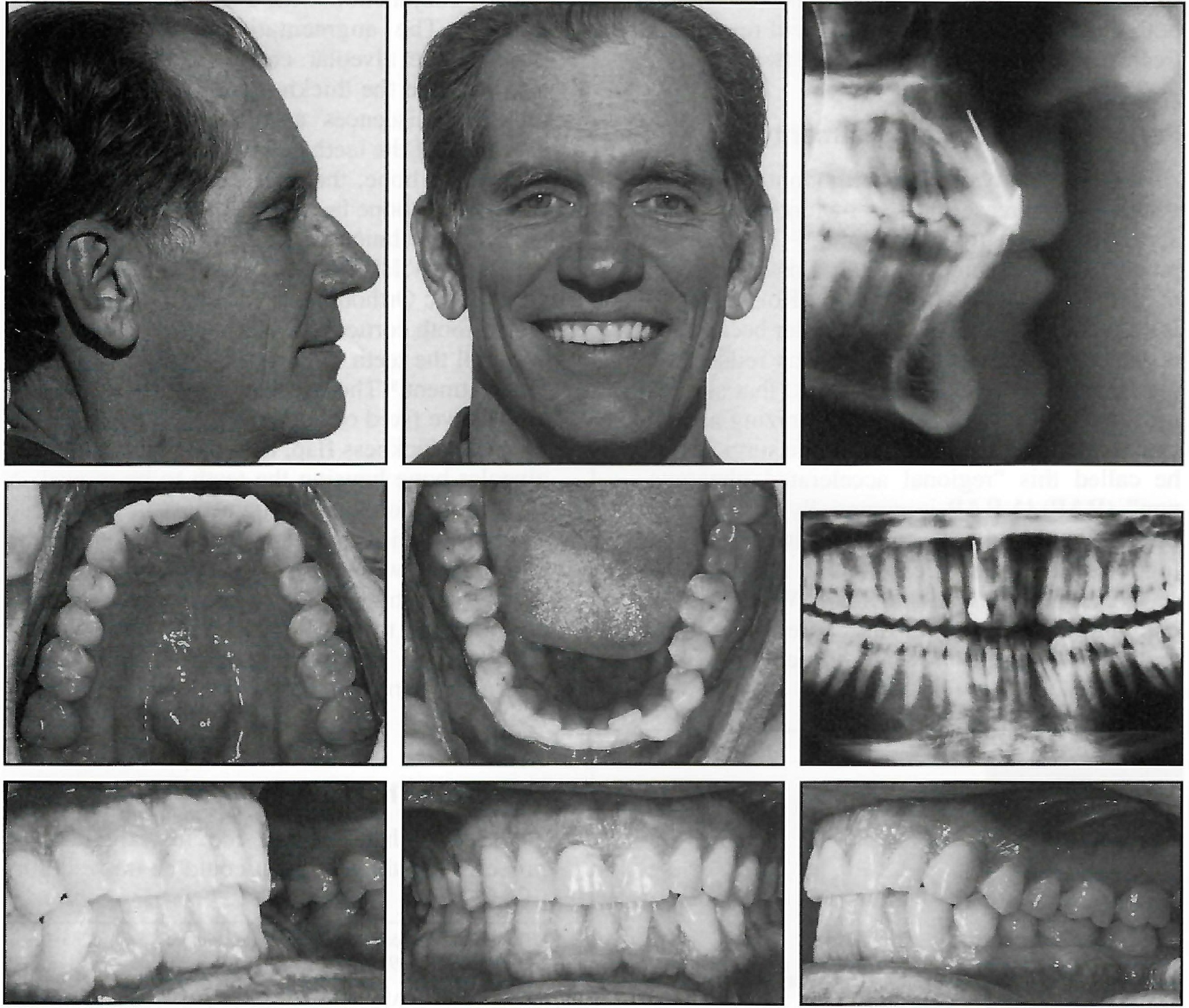
Fig. 1 Patient before treatment.
I had the AOO procedure performed by a local oral surgeon from the mandibular right to left canine. After 10 days of uneventful healing, I started the Invisalign therapy (Fig. 2).
The accelerated rate of tooth movement proved comfortable for the mandibular teeth, but since the surgery was not performed on the maxillary left lateral incisor, that particular tooth was sore for most of the treatment period. I was much more comfortable eating with the appliances in place than without them. The aligners caused no soft-tissue irritation, however, after I smoothed the edges with an emery board. My speech was compromised for only a short time. In fact, most of my patients had no idea I was wearing the aligners, even though they were inches away.
Eight weeks later, the soft-tissue profile remained unchanged, and the buccal occlusion, which did not need correction, was essentially the same (Fig. 3). The mandibular incisors were not tipped while being aligned, the crowding was corrected, and the overbite remained the same. The dental midlines were coincident. The maxillary arch was aligned, although slightly more rotation of the left lateral incisor would have been desirable. The lingual surfaces of both dental arches became stained, presumably from eating with the aligners in place, but there was no sensitivity of any teeth after treatment was completed.

Fig. 2 Upper and lower aligners (trimmed and smoothed for comfort).
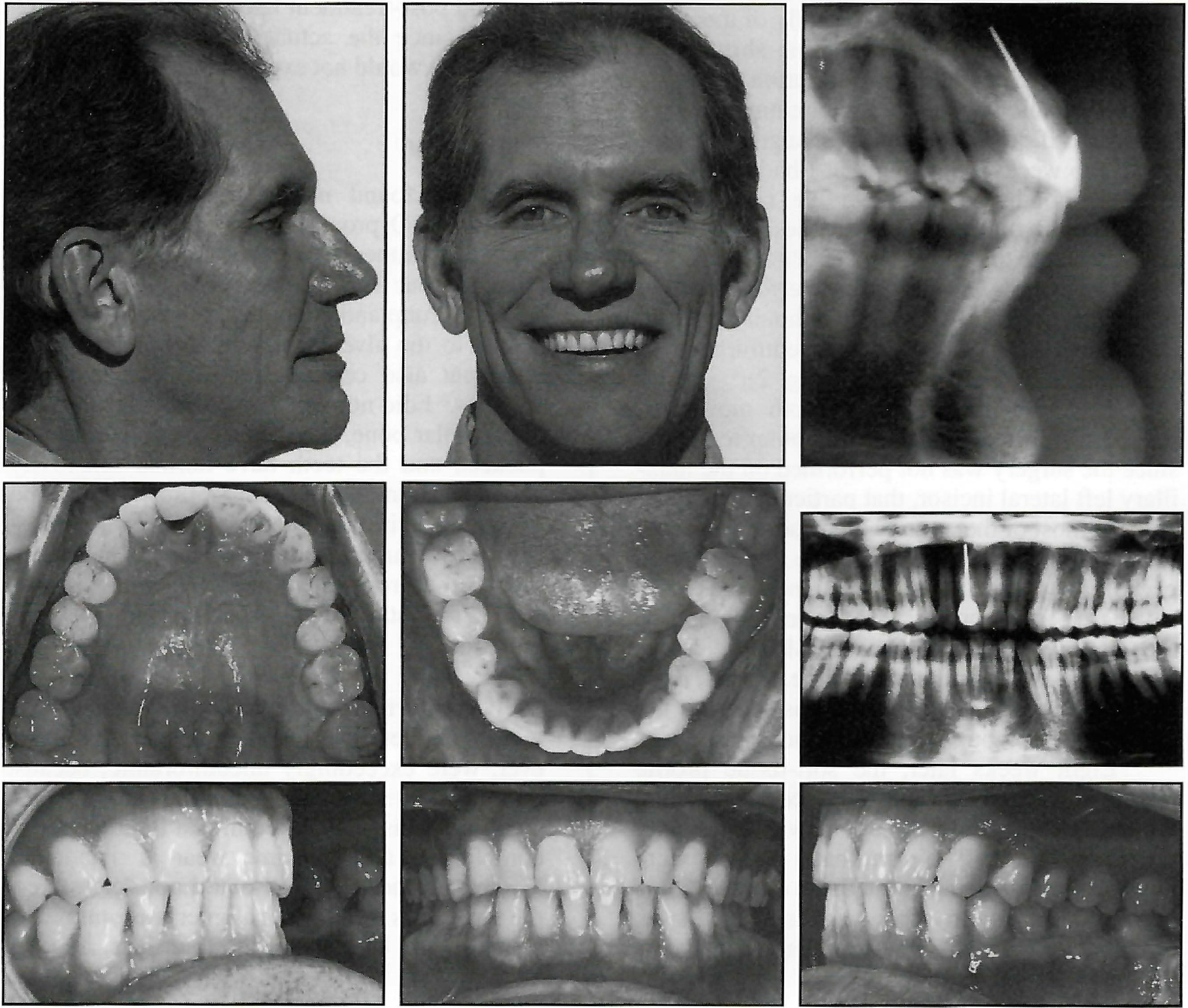
Fig. 3 Patient after surgery and eight weeks of Invisalign therapy.
Radiographically, the incisors that were moved showed no evidence of tipping or root resorption, although the mandibular left incisor appeared more tapered than before treatment. There was essentially no difference between the pre- and post-treatment lateral cephalograms. Of course, since the actual tooth movement was minor, one would not expect to see much change.
Discussion
Hajji found no differences between the RAP or AOO procedure and traditional nonextraction treatments, except that treatment was three to four times faster in the corticotomy-assisted group and B point increased significantly due to the alveolar augmentation.20 My self-treatment also corroborated the claims of the Wilckos.8 I did not take any CT scans to evaluate the alveolar bone, but there were no periodontal pockets, and the teeth have normal sensitivity. My occlusion has remained much the same, since the Invisalign treatment was programmed only for the anterior tooth movements needed to relieve the crowding. Since my treatment proceeded so fast, I did not experience any posterior intrusion.
I found that the surgical areas were relatively comfortable during Invisalign tooth movement. The teeth that were not operated on, however, were exceedingly uncomfortable, because both aligners were changed at the same accelerated rate. This system requires a high degree of compliance, and full-time wear is mandatory. Without further testing, I could not determine if the three days of wear per aligner was optimal, or if this should be increased to four days.
FOOTNOTES
- *Trademark and patent held by Wilckodontics, Inc., 6066 Peach St., Erie, PA 16509.
- **Trademark of Align Technology, Inc., 881 Martin Ave., Santa Clara, CA 95050.
REFERENCES
- 1. Kole, H.: Surgical operations on the alveolar ridge to correct occlusal abnormalities, J. Oral Surg. 12:515-529, 1959.
- 2. Suya, H.: Corticotomy in orthodontics, in Mechanical and Biological Basics in Orthodontic Therapy, ed. E. Hosl and A. Baldauf, Huthig Buch Verlag, Heidelberg, Germany, 1991.
- 3. Bell, W.H. and Levy, B.M.: Revascularization and bone healing after maxillary corticotomies, J. Oral Surg. 30:640-648, 1972.
- 4. Frost, H.M.: The regional accelerated phenomenon, Orthop. Clin. N. Am. 12:725-726, 1981.
- 5. Frost, H.M.: The biology of fracture healing: An overview for clinicians, Clin. Orthop. 248:283-293, 294-309, 1989.
- 6. Yaffe, A.; Fine, N.; and Binderman, I.: Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery, J. Periodontol. 65:79-83, 1994.
- 7. Chung, K.R.; Ko, S.J.; and Oh, M.Y.: Corticotomy-assisted orthodontics, J. Clin. Orthod. 35:331-339, 2001.
- 8. Wilcko, M.T. and Wilcko, W.M.: Lecture, Chicago, 1999.
- 9. Wilcko, M.T. and Wilcko, W.M.: Rapid orthodontics with alveolar reshaping: Two case reports of decrowding, Int. J. Period. Restor. Dent. 21:9-19, 2001.
- 10. Rummelhart, J.M.; Mellonig, J.T.; and Gray, J.L.: A comparison of freeze-dried bone allograft in human periodontal osseous defects, J. Periodontol. 60:655-663, 1989.
- 11. Mellonig, J.T.: Decalcified freeze-dried bone allograft as implant material in human periodontal defects, Int. J. Period. Restor. Dent. 6:41-55, 1984.
- 12. Schwartz, Z.; Mellonig, J.T.; Carnes, D.L.; DeLa Fontaine, J.; Cochran, D.L.; Dean, D.D.; and Boyd, B.D.: Ability of commercial demineralized freeze-dried bone allograft to introduce new bone formation, J. Periodontol. 67:918-926, 1996.
- 13. Meffert, R.M.; Thomas, J.R.; and Hamilton, K.M.: Hydroxyapatite as an alloplastic graft in the treatment of human periodontal osseous defects, J. Periodontol. 56:63-73, 1985.
- 14. Callan, D.P. and Rohrer, M.D.: Use of bovine-derived hydroxyapatite in the treatment of edentulous ridge defects: A human clinical and histologic case report, J. Periodontol. 64:575-582, 1993.
- 15. Sheridan, J.J.; LeDoux, W.; and McMinn, R.: Essix retainers: Fabrication and supervision for permanent retention, J. Clin. Orthod. 27:37-45, 1993.
- 16. Ponitz, R.J.: Invisible retainers, Am. J. Orthod. 59:266-272, 1971.
- 17. McNamara, J.A.; Kramer, K.L.; and Juenker, J.P.: Invisible retainers, J. Clin. Orthod. 19:570-578, 1985.
- 18. Rinchuse, D.J. and Rinchuse, D.J.: Active tooth movement with Essix-based appliances, J. Clin. Orthod. 31:109-112, 1997.
- 19. Kesling, H.D.: The philosophy of the tooth positioning appliance, Am. J. Orthod. 31:297-304, 1945.
- 20. Hajji, S.S.: The influence of accelerated osteogenic response on mandibular crowding, thesis, St. Louis University, 2000.



