JCO INTERVIEWS
Thomas D. Creekmore, DDS, on Treatment Mechanics
DR. WHITE Tom, you once said that "teeth want to be straight". Could you amplify that remark for our readers?
DR. CREEKMORE When I said that in a previous JCO article, I wanted to point out that there are two times when you can see that teeth want to be straight.1 The first time is when a person loses the anterior deciduous teeth and the permanent incisors replace them. If there is enough space between the deciduous canines, then the teeth will ordinarily come in straight. But if there is not enough space, the teeth will be crowded. At this stage, if the deciduous canines are removed, the teeth will align themselves. If there is enough space, the teeth will tend to align correctly.2
The second time you see the teeth wanting to be straight is when the primary posterior dentition is being replaced by the permanent bicuspids and cuspids. Typically, the permanent posterior dentition is smaller than the primary dentition, and if there is sufficient space, the teeth will erupt in a good alignment. If there isn't enough space, then the last teeth that erupt will be crowded out of the normal arch.
So the teeth do want to be straight if they have enough space to align themselves. If there is not adequate space, clinicians can provide space artificially by moving the posterior teeth distally and/or moving the anterior teeth forward in nonextraction treatments, or by removing teeth such as bicuspids. When these techniques are used successfully, the teeth will usually erupt and align correctly.
Similar articles from the archive:
- Teeth Want to Be Straight November 1982
- JCO Interviews Dr. Thomas D. Creekmore on Torque May 1979
- JCO INTERVIEWS Dr. Birte Melsen on Adult Orthodontics October 1988
But that only happens on an intra-arch basis, and it has nothing to do with aligning the upper teeth to the lower teeth. Correctly positioning the upper teeth to the lower teeth with a coincident centric occlusion and centric relation is the hardest part of orthodontics.
DR. WHITE There seems to be a resurgence of interest in expansion therapy to make more space in the jaws. What is your opinion of this trend?
DR. CREEKMORE Right now we don't have the scientific data to say how good or bad it really is. The expansion principle takes us back over a hundred years, when the common concept in orthodontics was that people were entitled to all the teeth they had. Expansion didn't work too well then, and I have an idea that the renewed emphasis on nonextraction treatment at all costs will meet with equal limitations. But we will have to wait a little longer until good data are available and objectively evaluated. I do think that many patients who should be treated with the removal of teeth are being harmed due to the nonextraction craze.
DR. WHITE Just how different are the brackets we use today from the original edgewise brackets developed by Edward Angle?
DR. CREEKMORE I think the first brackets introduced by Angle were made of gold and were single .022" brackets without rotating wings. All the attachments--such as the eyelets that were placed to correct rotational deficiencies in the single edgewise brackets--had to be soldered onto the gold bands, so clinicians had to have a lot of patience and skill to work with these first brackets.
With the introduction of stainless steel, it became possible to use smaller brackets and wires. Simultaneously, orthodontists saw the evolution of the .018" bracket and rotational wings, as in the twin bracket that Barney Swain developed and the Steiner, Lewis, and Lang winged brackets. But essentially, there hasn't been a great deal of change in how the bracket and the wire work together to control teeth in three planes of space since Angle's original edgewise bracket.
DR. WHITE You mentioned Angle's single bracket and the twin bracket developed by Swain. You recently developed a bracket that incorporates the advantages of both types. Could you describe this bracket?
DR. CREEKMORE Angle mentioned the importance of a wide interbracket distance to decrease the wire's stiffness. Essentially, wire stiffness depends upon at least three factors: 1) the material--whether it is made of gold, stainless steel, nickel titanium, etc., will give different stiffness to an archwire; 2) the size of the wire; and 3) the length of wire between brackets--a feature that orthodontists don't always appreciate. Single brackets, compared to twin brackets, increase interbracket distance about 50%, which decreases a wire's stiffness by about a factor of three.3 This is roughly the difference in stiffness between stainless steel and nickel titanium.
Back when we had only stainless steel wire, we would routinely make multilooped archwires to allow engagement of the brackets. The addition of a loop simply afforded more wire and subsequently more flexibility to the archwire. This is equivalent to increasing the interbracket distance.
The twin bracket at first offered better rotational control, which the single bracket couldn't match until rotational wings were added to it. Still, when a tooth is badly rotated and misaligned at the start of treatment, the rotational wing of a single bracket will interfere with the full engagement of an archwire, and some compensating bend or adjustment has to be made to engage the tie wing.
The twin bracket doesn't have that problem, so I developed a combination bracket, the Uni-Twin*, that could offer the best advantages of both types (Fig. 1). The bracket has the skeleton framework of a twin bracket, but the precision or working part of the bracket that is located in the center of the framework is no wider than a single bracket. The slot then widens considerably as it moves toward the edges of the twin bracket tie wings, and this feature allows the archwire to flex considerably, yet stay within the confines of the twin bracket. There is no interference with the archwire from rotational tie wings. This bracket ties like a typical twin bracket and rotates with the same efficiency of a twin bracket, but it offers all of the mechanical advantages of a single bracket--such as efficient torque delivery, reduced force within the bracket, and more wire flexibility.
DR. WHITE Tom, practically everyone today is using some kind of preadjusted appliance. Would you comment about the advantages and disadvantages of these systems?
DR. CREEKMORE In the first place, I think the main attraction of the preadjusted appliance is to simplify the orthodontist's work. There are basically two ways of positioning a tooth with an archwire: either place bends in the wire that will place the tooth where it needs to be, or build some features into the bracket that will do the same thing without the wire bends.
Larry Andrews was the first to do this on a commercial scale with the Straight-Wire Appliance**. He simply sought to make a system of brackets that could eliminate the 1st-, 2nd-, and 3rd-order bends orthodontists had to use. It was and is an absolutely valid concept. It may not necessarily make us do a better job, because it doesn't diagnose and treatment plan the case for us. But it does make the orthodontist's job easier by reducing the complexity of making archwires.4
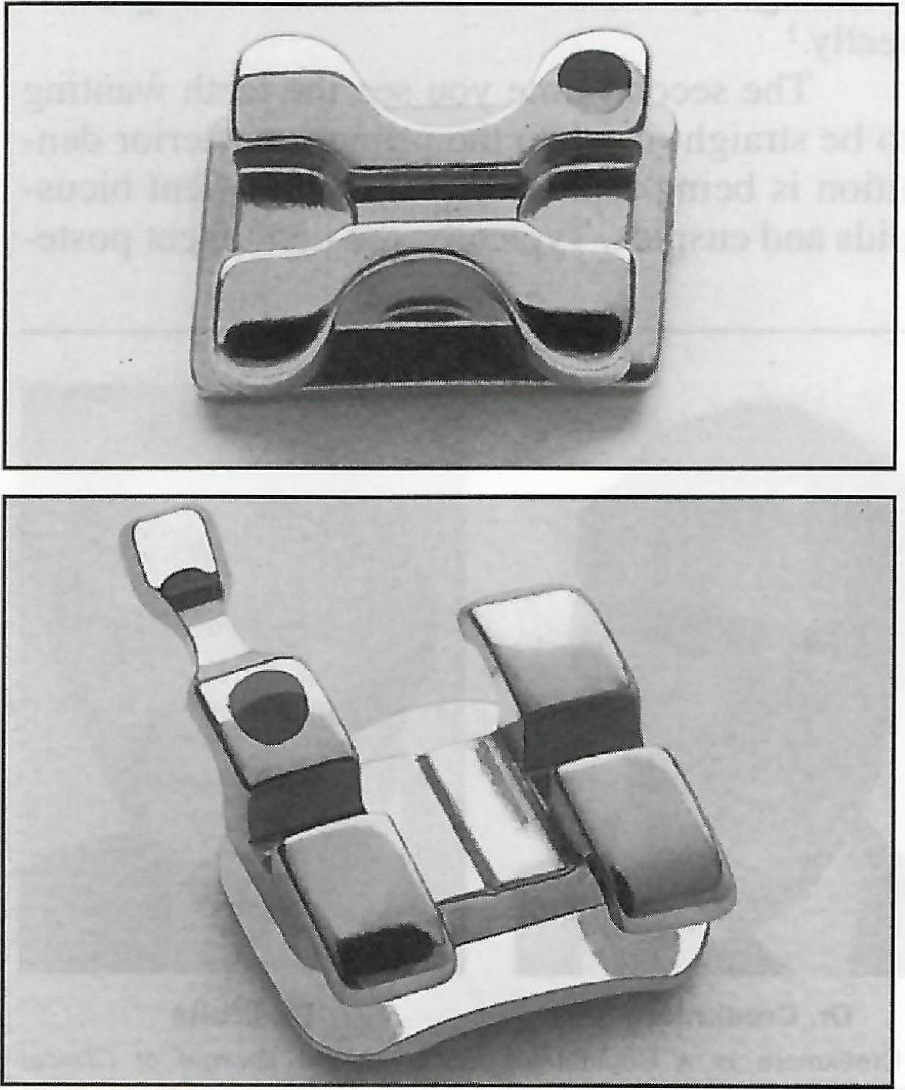
Fig. 1 Comparison of Mini Uni-Twin bracket (top) with conventional twin bracket.
However, there are several limitations with all preadjusted appliances when we expect teeth to be perfectly aligned without bends in the archwires. Even with perfect bracket placement and the use of "full-size" archwires, the same prescription will not deliver the teeth to the same positions in different malocclusions, due to play between the archwire and the bracket slot and to force diminution. These limitations have not been readily recognized by the profession, because when bending archwires to align the teeth, bends are accentuated until the teeth are aligned to the orthodontist's satisfaction. Thus, the bends include play and force diminution. This is also why the size of the wire vs. the size of the slot is not so important.
There is always play between the archwire and the archwire slot, even with "full-size" wires, due to manufacturing tolerances.5 Tolerances of .018" X .025" slots range from .0182" to .0192" with a midrange of .0187", and the .018" dimension in archwires is actually made .0178". This results in about 3° play in each direction from center. For example, if one central incisor is tucked under and the other is procumbent, a full-size wire would not deliver these crowns any closer than 6° to each other. Play in each direction increases to about 6° with an .017" X .025" wire and to about 12° in an .016" X .022" wire.
Force diminution becomes important as the archwire continues to work in the slot. The longer any wire works, the less force it exerts on a tooth. When the delivered force diminishes to a point that is no longer large enough to move the tooth, progress stops--not because the wire has taken a permanent set, but simply because the force is no longer great enough to move the tooth. Force diminution is especially evident in the torquing and leveling planes. As yet, no one has quantified force diminution.
What this means is that any prescription of a preadjusted appliance, with brackets perfectly positioned, just will not deliver the same finished result to different patients with different kinds of malocclusions.
Another important factor that will limit the usefulness of the preadjusted appliance is bracket positioning. Most orthodontists still do this important work directly in the mouth, which invites them to misplace the brackets from exactly where they need to be to deliver the teeth to optimum positions. If the bracket is misplaced, then wire adjustments or bracket replacement at a different position will become necessary.
DR. WHITE How can we overcome some of these limitations?
DR. CREEKMORE The next generation of preadjusted appliances will improve efficiency by customizing the brackets for 1st-, 2nd-, and 3rd-order movements according to the amount of play and force diminution inherent in each appliance.6 For instance, by measuring the inclination of the labial surfaces of the incisor crowns to the archwire plane with a special torquing template, and knowing that my appliance has about 4° play plus force diminution, I can determine how much torque will have to be placed in the brackets to achieve that 3rd-order movement, depending on which direction the teeth will be moved. Because of these measurements, I may decide to use a Roth prescription for extraction cases. For nonextraction cases, I may use an Andrews prescription for the maxillary teeth and an Alexander prescription for the mandibular teeth.
DR. WHITE The idea of having a highly individualized, customized appliance will appeal to many orthodontists, but how large an inventory of brackets do you have to maintain?
DR. CREEKMORE I want to address that issue, because it's not as difficult to customize the appliance as it may seem. Since practically all of the various prescriptions differ mainly in the anterior teeth, I have a complete inventory of Roth-prescription Mini Uni-Twin brackets. Then all I have to add is a small inventory of maxillary anterior brackets with Andrews prescription for maxillary teeth and mandibular incisor brackets with Alexander prescription. This gives me a variety of brackets to handle most situations, yet without the inventory expense we have with molar bands.
Besides the prescriptions I mentioned before relative to extraction and nonextraction cases, for a Class II, division 2 patient, I might select Roth central incisor brackets with 12° torque to deliver lingual root torque and Andrews lateral incisor brackets with 3° torque to deliver labial root torque to properly align the incisors without bends in the archwire. All of these brackets are compatible because they are the same Mini Uni-Twin brackets, but the different prescriptions let us mix and match for what particular teeth need.
To solve the bracket placement problem, we use an instrument I developed called the Slot Machine***that places these correctly selected brackets exactly where they should be with an indirect bonding technique (Fig. 2). These prescribed brackets are noted on the patient's chart so that if one is lost, it can be easily replaced from the inventory box with a minimum of fuss.
DR. WHITE Why do you think so many prescriptions have developed for preadjusted appliances?
DR. CREEKMORE It's because of the way different orthodontists work. Originally, Andrews used the averages he had measured from untreated, normal Class I occlusions to build his appliance. Over time, different orthodontists found Andrews's prescription wasn't satisfactory for the types of mechanics and wires they used. Ricketts, for instance, used a lot of .016" X .016" wires in .018" brackets. To deliver 7° of torque with this small a wire would necessitate having a bracket with 22° of torque. The same is true if you use an .022" bracket and finish with an .018" X .025" wire. There will be 16° of play between the bracket and the archwire, and the expected amount of torque will not be reached without a high-torqued slot. If you use one of these popular prescriptions, you may have to use the sequence of wires suggested by the developer, since the brackets will reflect a particular orthodontist's experience and prejudice about treatment mechanics. Incidentally, these high torques are only effective if the incisors are being retracted. If the incisors are moved forward and/or depressed, as in many nonextraction cases, the incisors will procline excessively.
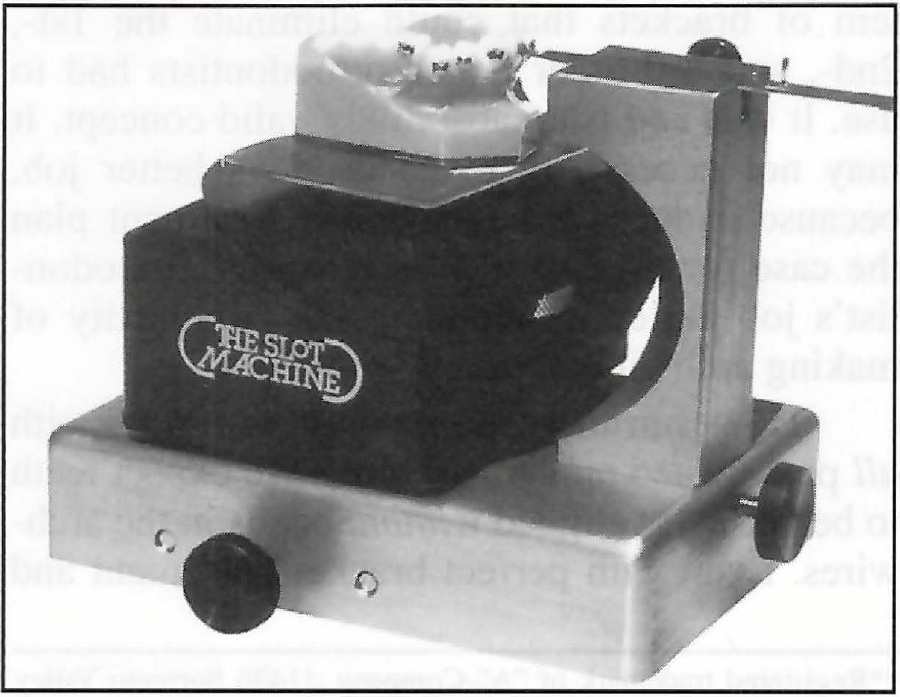
Fig. 2 The Slot Machine.
DR. WHITE But you have always advocated filling the bracket with wire as often as possible.
DR. CREEKMORE Well, it seems foolish to go to all the trouble of having a prescription that will deliver teeth to accurate positions and then not use the proper size wire that it needs to achieve that movement. I have always used full-size archwires--.018" X .025" wires in .018" X .025" brackets--without problems.4
DR. WHITE Does this lead to irregularities of alignment?
DR. CREEKMORE No, it does not. Some clinicians have alluded to irregularities in the alignments if full-size wires are used, but no one has ever shown this to be true. The solution for getting the preadjusted appliance to perform correctly is to use the right archwires and correctly position the right slots, which we do with the Slot Machine. Another complaint about using a full-size archwire is that it is too stiff and too difficult to put into the slots, but an .018" X .025" nickel titanium wire is more flexible than an .014" stainless steel wire. Also, an .018" wire is not really .018"; it is .0178". And the .018" X .025" bracket is somewhat larger than those dimensions. So the boundaries of the brackets give us an appliance that accepts a so-called full-size archwire much easier than most people think.
DR. WHITE Why has the use of lingual brackets declined so much, and what future do you see for this technique?
DR. CREEKMORE The reason it declined was that lingual orthodontics was introduced before we really learned how to use the technique. The media flurry in 1981 and 1982 caused the profession to accelerate the use of the appliance, but there is a fairly steep learning curve with lingual orthodontics that we weren't prepared for.
The lingual anatomy, archforms, and inclination needs are so different from those experienced with a facial appliance that people became confused; instead of seeing teeth correctly align, they began to see them misalign. Many of those original cases ended up being treated with facial appliances. Everyone thought it was going to be easy, but it didn't turn out that way at all.
The Ormco Task Force continued working with the appliance to develop strategies to solve all of the problems, and by 1985 or 1986, they had done that. By that time, so many people had been burned, they didn't want anything to do with lingual appliances.
I started working with an occlusally inserted lingual appliance in 1982 and didn't finish with it until about 1986. But I still had to develop a way to correctly place the brackets, and that was the original purpose of the Slot Machine--to orient the lingual bracket to the labial surface of the tooth.7
Right now there is a resurgence of interest in the lingual appliance in Europe and South America, and the quality of work being done with lingual appliances is extraordinarily high. It is a viable technique, but there is no doubt that it is more difficult. It requires a precise indirect bonding technique, it is less efficient because of the diminished interbracket distance, and it is more expensive--but it is viable. Only time will tell if orthodontists and the public will again develop a greater interest in the technique. I like to use it myself, but I have spent a lot of time developing the features that the technique needs to be done successfully.
DR. WHITE In the April 1983 issue of JCO, you became the first orthodontist to report on a patient treated with an implant.8 What future do you see for implants in orthodontics today?
DR. CREEKMORE I see a lot of advantages for implants and onplants in orthodontics. Implants as anchors are basically bother-free. They don't get sore. They don't hurt. They don't do anything but stay in place. The main problem is in finding a good spot to place implants in the maxilla and the mandible. There just aren't that many good locations, and that is the appeal of the onplants. They can be placed with a less invasive technique, at more sites, and can be removed easily at the conclusion of treatment.
Teeth are not particularly good anchors because of their mobility, and they don't always move in the directions we want them to move. Sometimes the anchor teeth will move as much as the target teeth. However, with implants or onplants as unmovable anchors, we should be able to plan the movements of the teeth with more precision. Even more important may be their use in relocating the jaws one to another, as in a long-face syndrome where you would want to move the mandible up toward the maxilla with a vertical force anchored to bones instead of teeth.
DR. WHITE So you see the potential of implants and onplants as anchors to reshape the jaws skeletally?
DR. CREEKMORE Why not? We are changing the relationship of the maxilla to the mandible with the Herbst† and other functional appliances that are anchored to the teeth. Why can't we do that with anchors that won't move the teeth into unfavorable positions? We can use implants to move teeth dentoalveolarly, so why not use them to reposition the jaws vertically, horizontally, anteriorly, and posteriorly? I think they have terrific potential.
DR. WHITE How do you stand on distal movement of maxillary molars to correct Class II malocclusions and to increase maxillary arch length?
DR. CREEKMORE I think it has limitations. Distal movement of the maxillary molars is difficult mechanically, and the movement of mandibular molars is even harder. Also, when we distally position molars, we encroach upon the space reserved for the second and third molars. I think there are definite anatomical limits to how far these teeth can be repositioned distally without some harmful sequelae. Some orthodontists have suggested removing maxillary second molars to avoid this encroachment, but even with that, the technique is still probably less efficient than removing maxillary bicuspids, retracting the anterior teeth, and moving the molars into a full Class II relationship with reciprocal anchorage. The bicuspid represents only 7-8mm of tooth structure, whereas the second molar represents 10-12mm.
DR. WHITE Do you see any relationship be tween extractions and TMJ dysfunction?
DR. CREEKMORE With all of the anxiety about the effect of extractions on the TMJ, no one has yet proven that extractions have anything to do with TMD. Extractions don't make patients susceptible to periodontal problems. Facial esthetics are not compromised by extractions when orthodontists are prudent about their selection of teeth to extract and the mechanics they employ. Certainly, you don't take teeth out on everyone, and I can recall two patients for whom I opened space for two additional bicuspids. They needed six bicuspids instead of four. The need is for correct diagnosis, not for some rationale to justify a nonextraction formula. There is nothing wrong with doing extractions when they are needed.
DR. WHITE Do you think we need to take another look at our popular cephalometric analyses?
DR. CREEKMORE Yes. The analyses are based on average tooth positions for average jaw relationships, which means teeth will be positioned correctly if the jaw relationships are average. But when the jaw relationships differ from average, the analyses suggest positions for the teeth that will be too retrusive in high ANB angle cases and too protrusive in low ANB angle cases.9
If you look at all the popular analyses and treatment-planning guides used today--the Tweed triangle, the Steiner analysis, the Williams APo line, or the Ricketts VTO--you will notice they have one feature in common. All of them first position the mandibular central incisors cephalometrically for an average jaw relationship, and then build the rest of the treatment around those teeth.
DR. WHITE So you think our conventional analyses wrongly design treatment around the mandibular incisor, which is really the dentition's compensating mechanism?
DR. CREEKMORE That's right. Casko,10 Mc Namara,11 and others have studied esthetic, normal Class I occlusions and have found normal jaw relationships, as measured by the ANB angle, to vary from -3° to 8°, and mandibular incisors to vary in their relationship to the APo line from -3mm to 6mm. That doesn't mean there is a big target and if the teeth are positioned within that 9mm range, they will be OK. Lower incisors lingual to the APo line are found in low ANB angle or low-convexity relationships, whereas lower incisors labial to the APo line are found in high ANB angle or high-convexity relationships.
Conversely, the position of the maxillary incisors varies much less. What is found in esthetic faces, regardless of the jaw relationship, is that the maxillary central incisors will be nicely positioned in the premaxilla, 3-8mm in front of the NA line. When the ANB angle is 6° in an esthetic Class I patient, the mandibular incisors will compensate for this large discrepancy be tween the mandible and maxilla and will be positioned forward on the mandible, toward the higher part of the range. When there is less maxillomandibular discrepancy, the mandibular incisors will be found farther lingually to compensate. This is opposite to the recommendations in the Steiner analysis, for example.
DR. WHITE How do you determine where to place the anterior teeth in your treatment plan?
DR. CREEKMORE Some of the analyses can be modified to incorporate these findings. Any analysis, such as the Tweed triangle, that is based only on the angulation of certain teeth cannot be valid, because angulations do not denote anteroposterior position. The Steiner analysis can be modified by using the measurement of the lower incisor to NB and subtracting the measurement of Po to NB--referred to as the Holdaway ratio--which should equal the ANB angle. For example, in a 2° ANB angle case, the lower incisor would be 2mm forward of Po relative to NB. For a 6° ANB angle, the incisor would be 6mm forward of Po re NB. For a -2° ANB, the incisor would be 2mm behind Po re NB.
Analyses that use the lower incisor to the APo line can be modified so that the lower incisor to APo measurement equals the convexity. For example, in a 6mm convexity case, the lower incisor would be 6mm anterior to the APo line. For a 2mm convexity, the lower incisor would be 2mm anterior to APo. For a -2mm convexity, the lower incisor would be 2mm lingual to APo.
Radney observed in his well-treated cases that the maxillary incisors were centered in the premaxilla and the incisal edges of the lower incisors were consistently aligned with the line NA, regardless of the jaw relationship.12 The Radney Modified Analysis, by positioning the lower incisors relative to the line NA--not NB or APo--will automatically position the lower incisors on the mandible to compensate for variable jaw relationships, and will also position the upper incisors 4-5mm anterior to the line NA.
Perhaps some of the blame for extracting too many teeth and retracting teeth too far in the face is due to inaccurate goals advocated as ideal by our cephalometric analyses. We need to stop using averages, expand our view of what is normal, and treat to an ideal for the individual.
DR. WHITE Tom, JCO and its readers thank you for reminding us to challenge some of our cherished presumptions and to consider patients' individual needs rather than preconceived formulae.
REFERENCES
- 1. Creekmore, T.D.: Teeth want to be straight, J. Clin. Orthod. 16:745-764, 1982.
- 2. Creekmore, T.D.: Physiologic drift, J. Clin. Orthod. 9:749-773, 1975.
- 3. Creekmore, T.D.: The importance of interbracket width, J. Clin. Orthod. 10:530-534, 1976.
- 4. Creekmore, T.D.: The new torqued appliance, J. Clin. Orthod. 7:553-573, 1973.
- 5. Creekmore, T.D.: JCO Interviews on torque, J. Clin. Orthod. 13:305-310, 1979.
- 6. Creekmore, T.D. and Kunik. R.L.: Straight wire: The next generation, Am. J. Orthod. 104:8-20, 1993.
- 7. Creekmore, T.D.: Lingual orthodontics-Its renaissance, Am. J. Orthod. 96: 120-137, 1989 (winner of B.F. and Helen Dewel Award for best clinical article of 1989).
- 8. Creekmore, T.D.: The possibility of skeletal anchorage, J. Clin. Orthod. 17:266-269, 1983.
- 9. Creekmore, T.D.: Where teeth belong in the face and how to get them there, lecture, AAO annual meeting, Denver, 1996.
- 10. Casko, J.S. and Shepherd, W.B.: Dental and skeletal variation within the range of normal, Angle Orthod. 54:5-17, 1984.
- 11. McNamara, J.A. Jr. and Ellis, E. III: Cephalometric analysis of untreated adults with ideal facial and occlusal relationships, Int. J. Adult Orthod. Orthog. Surg. 3:221-231, 1988.
- 12. Radney, L.: Personal communication, 1996.