JPO Interviews Dr. Charles H. Tweed, Part 3
This is the third and concluding installment of the Tweed Interview conducted by Dr. Sidney Brandt, Interviews Editor for JPO. The first two installments appeared in the December, 1967, and January, 1968 editions of JPO.
DR. BRANDT: The profession seems to be showing a decrease in its utilization of serial extraction procedures. Would you please tell us your latest thinking on this and whether you agree with my feeling that there is a lessening of serial extraction?
DR. TWEED: Well, it would be difficult for me to suggest that you were not correct in your appraisal. My only comment is that if that is true it is a pity that the profession is not aware of the tremendous benefits that can and do result from scientific serial extraction procedures. It is said one can lead a mule to water but one cannot make him drink.
Similar articles from the archive:
- JPO Interviews P. Raymond Begg January 1967
- JCO Interviews Robert M. Ricketts April 1970
- JCO Interviews Dr. Charles J. Burstone December 1972
DR. BRANDT: There have been some articles published which indicate that premature removal of deciduous teeth does not hasten the eruption of the permanent successor, but rather might retard the speed of eruption by laying down a more dense layer of bone. Has this been your finding?
DR. TWEED: I have rarely observed that in my 10 years of serial extraction procedures.
DR. BRANDT: Do you ever instruct an oral surgeon to scoop away any o£ the bone overlying the permanent teeth that you wish to erupt faster?
DR. TWEED: Not unless the patient presented what is known as a submerged deciduous tooth. In that instance I do.
DR. BRANDT: Your serial extraction sequence is started in the 7½-8½ year age group.
DR. TWEED: Correct.
DR. BRANDT: Are you guided on when to start serial extractions by the amount of bicuspid root formation? Is this any sort of criterion?
DR. TWEED: No.
DR. BRANDT: When the four deciduous first molars are removed, one can usually note little lingual movement of the mandibular incisors. Would it be fair to say that the bite does not close down very much?
DR. TWEED: It would not be fair to say that, because the bite, as a rule, does close-- varying from a little to considerable.
DR. BRANDT: Do you limit your practice to certain age groups?
DR. TWEED: Yes, from approximately 4-11 years of age. I do not wish to imply that when a patient reaches the age of 11½ he is shunted out o£ my office. Quite often there will be delayed eruption of teeth and some of these patients might reach the age of 14-15 before treatment is begun, but that does not occur too often.
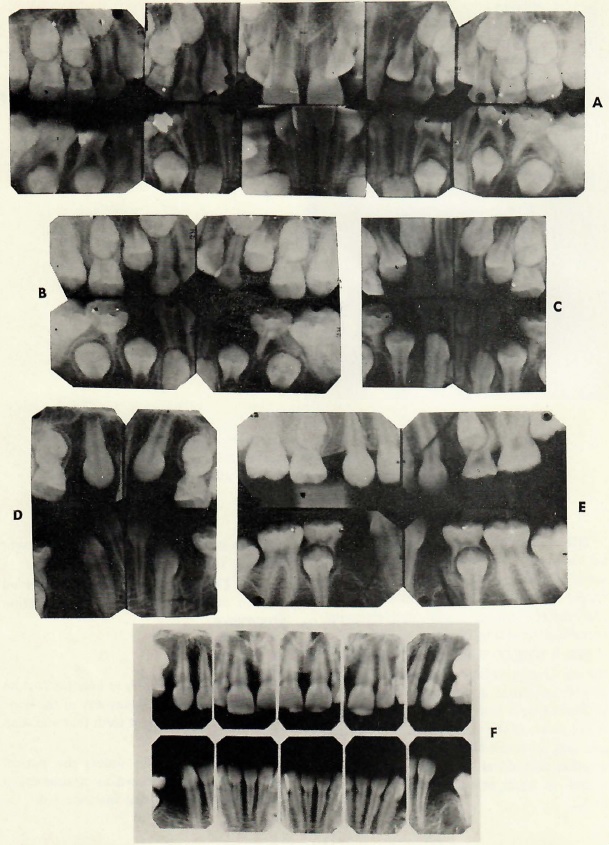
Fig. 1 Serial extraction sequence for patients 7 1/2-8 1/2 years of age with discrepancy between teeth and basal bone. A. At approximately 8 years old, extract four deciduous first molars. B. Let first bicuspids erupt through alveolar bone. C. When first bicuspids have erupted through alveolar bone, extract four first bicuspids and four deciduous cuspids. D. and E. If step C was 4-6 months prior to eruption of permanent cuspids, they usually migrate posteriorly into a good position. F. Mild irregularities of mandibular incisors correct themselves and these teeth tip lingually. (From Tweed: Clinical Orthodontics, The C.V. Mosby Co., St. Louis, MO. 1966)
DR. BRANDT: Thank you. And now let's go to some questions on proper retention as you see it. Some of our contemporaries reject the use of prolonged retention in any form, including soldered lower cuspid-to-cuspid units, Hawleys, etc. How do you control the transition of removing active appliances and applying retention? And please describe the instructions delivered to the patients.
DR. TWEED: As a rule, in my office, retention varies from none at all to as much as 4 or 5 years. As a general rule, when active treatment has been completed, the retaining devices of my choice are two Hawley retainers, a maxillary and a mandibular. The Hawley retainer has attachments-- the labial bar circles the four anterior teeth, cuspid clasps are soldered to the labial bar to engage the labial surfaces of the cuspids and molar clasps are placed as near the gum level as possible and placed immediately mesial to and against the mesial surface of the drastically tipped maxillary molars. If I have not mentioned it, the bite plane is also included in the maxillary unit. In the mandibular retainer the usual procedure is a labial wire around the four mandibular incisors. The wire is usually .020 round that goes up and over the contact. Included in the mandibular retainer are molar stops to prevent the retainer from impinging on soft tissues together with clasp-like wires that go up and over the contacts of the cuspid and bicuspid and act as little clasps to stabilize the retainer and prevent the patient from playing with it with his tongue. Now, as a rule, these retainers are worn for approximately six months at which time both retainers are taken away from the individual and a new mandibular cuspid-to-cuspid lingual bar retainer replaces the mandibular Hawley. A new maxillary retainer equipped with a bite plane and attachments to allow the wearing of an elastic around the labial of the four maxillary incisors is made. The new maxillary retainer is worn at night only after the ninth month. As I mentioned before, length of retention varies from no retention whatsoever to from 3 months to as much as 4 or 5 years depending upon the problems that have been faced.
DR. BRANDT: Now, if I understand that correctly, when the maxillary and mandibular retainers are issued, they are worn for 6 months full time, day and night.
DR. TWEED: Correct.
DR. BRANDT: The retainer is a factor in holding the bite well opened. Once the retainer is discontinued have you found that the opened bite maintains itself?
DR. TWEED: As a rule, yes. One of the reasons for over-treatment that we just discussed was that one must figure on a slight relapse in the degree of overbite following the termination of retention. But, as a rule, it is not great.
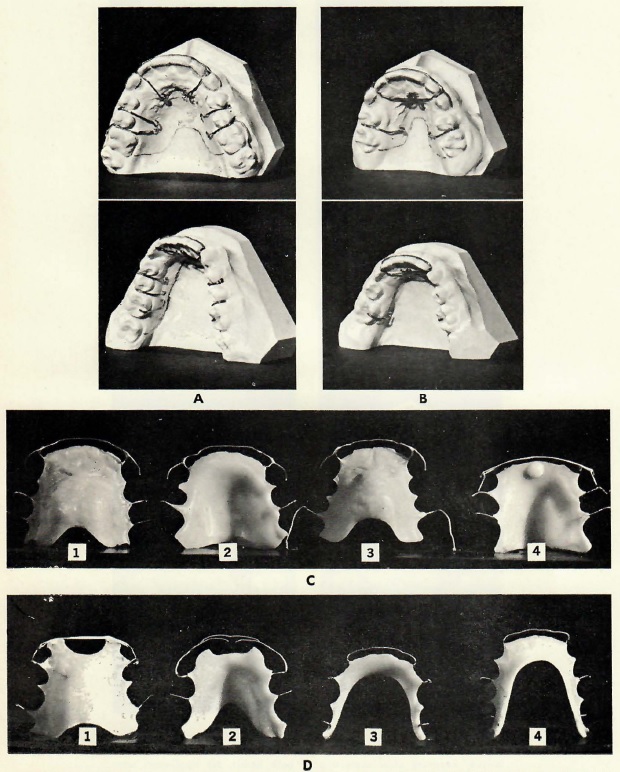
Fig. 2 Examples of retainers used with the Tweed Technique. (From Tweed: Clinical Orthodontics, The C.V. Mosby Co., St. Louis, MO. 1966)
DR. BRANDT: How about Class II Division 2 cases?
DR. TWEED: In Class II Division 2 cases in my practice, I find it advisable to continue the wearing of the maxillary retainer with a bite plane at night for perhaps 2 or 3 years.
DR. BRANDT: How do you feel about selective grinding or equilibration?
DR. TWEED: I am all for selective grinding or equilibration following treatment and after the denture has settled. But I do not think the teeth should be appreciably equilibrated immediately following active treatment.
DR. BRANDT: Do you think the orthodontist should do this or should this be referred back to either the dentist or the periodontist?
DR. TWEED: Personally, I don't think that many orthodontists are qualified to scientifically equilibrate a denture and that includes myself. I am very careful to whom I send my patients for equilibration. We have one outstanding periodontist in this town, Dr. Leonard Weiner, who does any equilibration that I feel is necessary.
DR. BRANDT: Do you ever use positioners?
DR. TWEED: No! Not for the past 10 or 12 years.
DR. BRANDT: Now a few queries that concern so many of us and I sort of term these quickly questions although they do not have to be answered in such a fashion. My first question is about tongue thrust and reverse swallowing, but I think you have answered this before. What do you think of the various means offered for the correction of tongue thrusting, the treatment thereof, and their effect upon the stability of the treated malocclusion?
DR. TWEED: Sid, do you mean mechanical appliances, like lingual bars and rakes?
DR. BRANDT: Yes, either associated with or differentiated from speech therapy.
DR. TWEED: I have personally never used such devices. I depend completely upon my speech therapist to correct any habits such as sucking habits. The patient is observed over a long period of time and, if I observe there has been a relapse or a recurrence of the habit, the patient is referred to the speech therapist for further treatment.
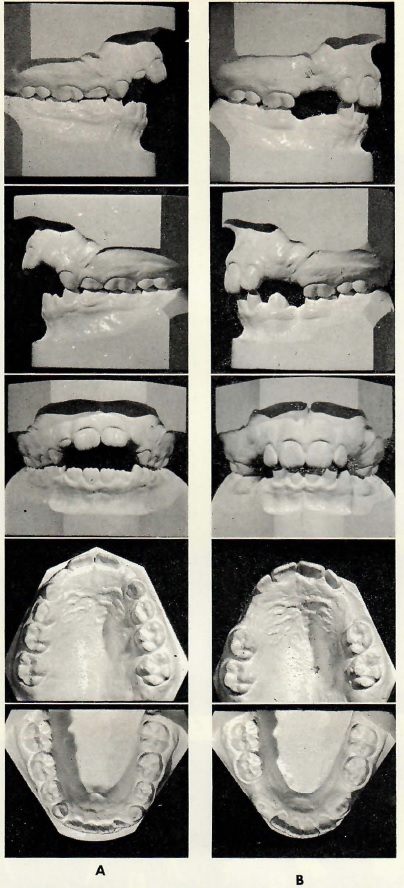
Fig. 3 A. Malocclusion resulting from thumb-sucking and reverse swallow. B. Recovery after correction of both habits. No appliances were used. (From Tweed: Clinical Orthodontics, The C.V. Mosby Co., St. Louis, MO. 1966)
DR. BRANDT: You are also, of course, aware of the growing interest in splitting the palate and attaining rapid palatal expansion. What are your thoughts and recommendations on this procedure?
DR. TWEED: I think at times it's a very excellent procedure, particularly in these narrow palate cases, accompanied by mouth-breathing.
DR. BRANDT: In considering growth, do you think the orthodontist can favorably affect these growth trends with early treatment?
DR. TWEED: You're speaking about classification of growth trends? No, I do not.
DR. BRANDT: Would you correct a unilateral 1st molar cross-bite in an early mixed dentition?
DR. TWEED: I do. Routinely.
DR. BRANDT: How do you do it mechanically?
DR. TWEED: With appliances and cross-bite elastic force.
DR. BRANDT: How about diastemas between upper centrals? Would you ever attempt just to close that space and no other major tooth movement?
DR. TWEED: Sid, do you mean without surgical removal of the frenum?
DR. BRANDT: Yes sir. If a patient presented with a diastema between the two upper central incisors and apparently no frenectomy was necessary, would you attempt to close that space and no other major tooth movement at all?
DR. TWEED: I wouldn't until I had thoroughly explained to the patient that she'd perhaps have to wear a retainer for several years and possibly for the rest of her life.
DR. BRANDT: Good, that's the answer that I expected would come out. If you do order a frenectomy do you ever place the bands on the upper anteriors first?
DR. TWEED: I have, but as a rule I do not.
DR. BRANDT: I'd like to discuss light wire technique with you. The comments on this technique in your book were not very flattering. However, it does appear that treatments like the Begg technique are here to stay. One of the first things that comes to my mind is how would you account for so many edgewise practitioners becoming devotees of light wire?
DR. TWEED: My comments on the Begg technique were not complimentary. There was nothing personal in my remarks. I consider Dr. Begg a gentleman. When Dr. Begg presented a clinic of about 40 cases some 10 years ago at one of the large meetings in the East and assured his listeners that length of treatment time varied from 4 to 8 or 10 months the profession including myself was impressed and amazed because some of these cases were difficult adult malocclusions to treat. Obviously many orthodontists were impressed even though no cephalograms nor after-treatment intra-oral x-rays were included in the clinic. Many orthodontists were interested in larger practices and more income and, forgetting that an excellent professional service rendered is infinitely more important than any fee involved, flocked to take the Begg course.
It was interesting to note that at the Foundation Meeting in New York in 1962, the average length of treatment time by those using the light wire and Begg technique was approximately 30 months as compared to Dr. Begg's treatment time of 4 to 10 months. This should have demonstrated the difficulties of the Begg technique in the hands of all those who, unlike Dr. Begg, are not master technicians and who must depend upon positioners to complete their treatment. Yes, Sid, I realize many edgewise practitioners have gone Begg in recent years. You of course realize that there are also many disillusioned with the Begg technique who are attending the courses given here in Tucson under the auspices of the Foundation. Each applicant accepted to take the course must bring the complete records of 5 treated cases and frankly, among other things, the members of the teaching staff are alarmed by the extent and prevalence of root resorption occasioned by the use of uncontrolled light wire forces. In addition, the consistency with which B point drops down and back often detracting from rather than enhancing facial ethetics demonstrates that treatment mechanics of the light wire technique are violating the inherent directional growth vector of the mid and lower face of a large percentage of the patients being treated with that mechanism.
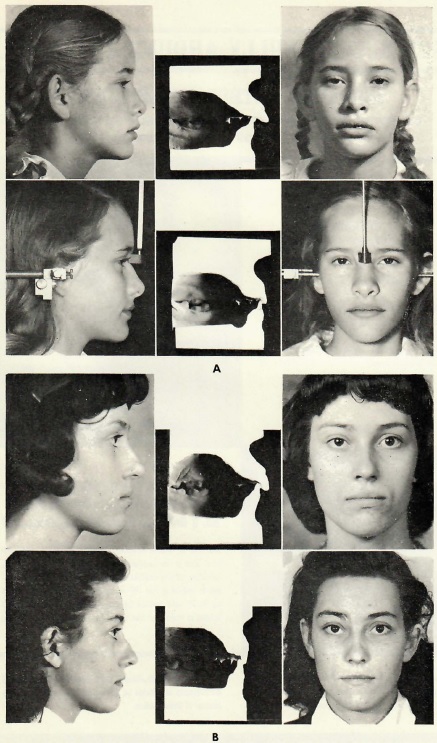
Fig. 4 Dr. Tweed's concept of improvement in facial esthetics through orthodontic treatment and its relationship to the uprightness of mandibular incisors on basal bone. (From Tweed: Clinical Orthodontics, The C.V. Mosby Co., St. Louis, MO. 1966)
DR. BRANDT: What advice would you give to practicing orthodontists who are considering changing their treatment procedures to light wire?
DR. TWEED: If the individual is of age and is able to analyze both appliances and he feels that perhaps there are advantages other than money in changing to the light wire, who am I try to dissuade him?
DR. BRANDT: What contribution, if any, do you think Dr. Begg made to orthodontics?
DR. TWEED: I think that Dr. Begg has made an important contribution to orthodontics. The development of his highly resilient light wire I think has been a major contribution to orthodontics that will be remembered by the profession.
DR. BRANDT: Dr. Tweed, we have now covered a rather wide range of subjects in this past hour and a half. If a young man considering orthodontics as a career were listening he might very well flinch at the number of problems and uncertainties facing our specialty. Would you recommend orthodontics as a specialty and why?
DR. TWEED: Sid, that is the age-old story and question that is passed on from one generation to another. My grandfather's theme song was the same one my father sang to me-- it goes as follows: "I'm glad that I'm not going to have to live the life that you're going to have to lead for the next forty years." My father told me the same story. And, in honesty, I at times sing the same story to my grandchildren, but I really don't believe it. I think the world is getting better, that progress is being made and that there will always be room for wonderful, sincere young men in the healing professions in the future. Government may make regulations that we feel are severe, unless we correct some of the laxities in our profession. Perhaps if we spent a little more time endeavoring to improve our professional services rather than expending so much effort in the mad race for more dollars, we could fulfill our obligation to our profession as well as the public. Sid, the orthodontic profession is one of the most lovely professions that I know of. If I had my life to live over I'm sure I would want to be an orthodontist and if I could rub Aladdin's lamp and pass on a good wish to all young men it would be that their professional lives be as soul satisfying and as beautiful to them as mine has been to me.
DR BRANDT: Dr. Tweed, thank you most sincerely for giving your time and expressing your thoughts so frankly and honestly. The readers of the JPO will be equally grateful when they read what you have told me.
On a personal note, this has been a most rewarding experience, and I shall never forget spending this time with you.
DR. TWEED: And thanks, Sid, I too have enjoyed this experience.



