JPO Interviews Dr. Charles H. Tweed, Part 2
This is the second installment of the Tweed interview, which was conducted by Dr. Sidney Brandt, Interviews Editor of JPO. The first part appeared in the December 1967 issue.
DR. BRANDT: In your book you note that you have attained the objectives in your cases approximately 80% of the time. To clarify what your objectives are, would it be fair to say that you are pleased when active appliances are removed and the patient falls within the normal reading of the Tweed triangle?
DR. TWEED: Not always, Sid. I stated in my book that the diagnostic facial triangle is a guide for the young man, a very accurate one in more than 95% of cases, but in the final analysis, the eye is the deciding factor. However, if the patient complies with the angular requirements of the diagnostic facial triangle and your eyes tell you that the face is protrusive, then forget the triangle and follow good, common horse sense and move the denture further posteriorly.
Similar articles from the archive:
- JPO Interviews P. Raymond Begg January 1967
- JCO Interviews Robert M. Ricketts April 1970
- JCO Interviews Dr. Charles J. Burstone December 1972
DR. BRANDT: In line with that, with your treatment procedures, do you believe in overtreatment? By overtreatment I am referring to rotations, or general overtreatment in every aspect of treatment.
DR. TWEED: I think slight overtreatment is very desirable in most instances. However, one must be familiar with the growth trend classification. For instance, a Type C growth trend case would not require as much overtreatment as a Type B growth trend case. If the lower jaw is growing downward and forward more rapidly than midface, overtreatment would not be necessary. On the other hand, if the cephalometric records reveal that the patient presents a Type B growth trend with upper face or maxilla growing forward more rapidly than lower face or mandible, then by all means one should endeavor to overtreat the patient mesiodistally.
DR BRANDT: How much change occurs cephalometrically in your 80% successful cases that are a few years out of retention? Now, your successfully treated cases are seen several years out of retention. How much change occurs cephalometrically?
DR. TWEED: You recall, Sid, in reading my recently published treatment manual titled Clinical Orthodontics, that treatment objectives concerned FMIA, the most stable of the three angles comprising the diagnostic facial triangle. To fulfill the requirements of the diagnostic facial triangle it was necessary to attain an FMIA of 65° in all patients whose FMA angulations ranged upward from 30°; for patients whose FMA angulations ranged from 30° to 20°, the attainment of an FMIA of 68° was required to fulfill the angular requirements of the diagnostic facial triangle. In flat-angle cases whose FMAs ranged downward from 20°, it was deemed expedient not to exceed an IMPA greater than 94°. Therefore, the FMIA readings read from 68° when FMA read 20° to as much as 75° or more when FMA approached 12°. To answer your question. The FMIA angulation in the cases several years after treatment is quite stable. If there is a slight change in FMIA it improves, meaning an increase toward the 70° rather than a retrogression toward 65°. Anyone who has followed the growth processes of 100 children from 7 to 21 years is aware of the fact that on the average there will be a reduction of at least 5° in FMA. In unusual cases this reduction is as much as 12°.
One observes strange phenomena in some growing children following active treatment in which the angular requirements of the diagnostic facial triangle have been attained. For example, let us suppose the angular measurements of the patient following treatment read FMA 25°, IMPA 90°, FMIA 65°. Some one or two years later a new cephalogram is made, and after the FMA has flattened 2° to read 23°, quite often in such instances there will be a corresponding increase of 2° in IMPA, which will read 92°, with FMIA remaining constant at 65°. The reverse also seems true. If FMA increases 2° to 27°, the IMPA decreases to 88° and FMIA remains constant at 65°. Specifically: FMIA remains relatively stable, FMA and IMPA fluctuate during growth movements.
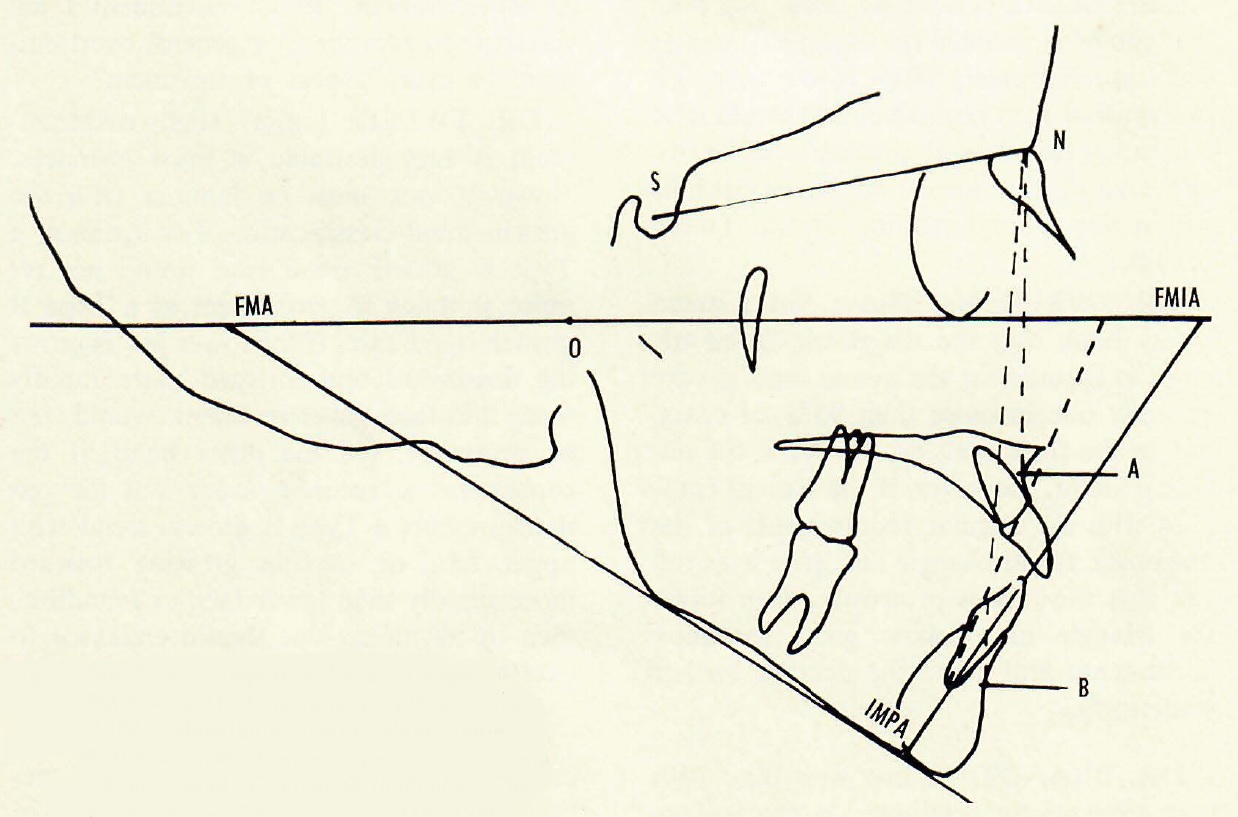
Fig. 1 The Tweed diagnostic facial triangle:
FMA--Frankfort mandibular plane angle
IMPA--Mandibular incisor plane angle
FMIA--Frankfort mandibular incisor angle
(from Tweed: Clinical Orthodontics, The C.V. Mosby Co., St. Louis, MO. 1966)
DR. BRANDT: What about the recrowding of lower incisors? Does this happen?
DR. TWEED: Sid, it certainly does. Unless one is completely acquainted with facial growth trends, many of our beautiful cases will develop irregularities in the mandibular incisor area, the reason being that in Type C growth trend cases the mandible or lower face is growing forward at a more rapid rate than midface or maxilla. The mandibular incisal cutting edges strike the lingual surfaces of the maxillary incisors, and one of two reactions will occur. If the patient has flaccid, loose lips, the maxillary incisors will be tipped forward, often improving maxillary incisor inclinations in the treated cases, which are often left too vertical. On the other hand, if the lips are thin and strong, and the orbicularis oris is well developed, the mandibular incisors moving forward more rapidly than maxillary incisors will strike the lingual surfaces of the maxillary incisors. The tense lips will prevent the maxillary incisors from tipping forward, and the result will be that the mandibular incisors will be tipped lingually. This will oftentimes result in the development of irregularities in the incisal segment. For this reason I feel a knowledge of growth trends is important, because in these children who present Type C growth trends, the mandible is at times moving forward much more rapidly than maxilla to the extent that ANB changes from 5° to 1 ° or 2° in a period of two years. It is good procedure to place a mandibular cuspid-to-cuspid lingual bar retainer to prevent the mandibular incisors from tipping lingually and developing rotations and irregularities. The lingual bar should be worn until the cessation of active growth. In girls it will be less than in boys, but I would say that it would be in the neighborhood of 18 years of age before one would dare to remove that cuspid-to-cuspid lingual bar.
DR. BRANDT: Do you discuss this with parents at all?
DR. TWEED: I sure do.
DR BRANDT: At what point?
DR. TWEED: Right from the beginning. I talk an hour to my parents and acquaint them with the importance of growth trends and the problems faced by the orthodontist. The parents also know they must follow instructions in all matters concerning their child's orthodontic treatment. The child must continue to wear this cuspid-to-cuspid lingual bar until I feel that it should be discontinued. At the end of eight to 12 months of retention, a new maxillary retainer is made. The new maxillary retainer is equipped with a biteplane and a light elastic used to replace the labial bar, which will permit the maxillary incisors to tip slightly forward as the mandibular incisors strike the lingual surfaces of these teeth.
DR. BRANDT: To clarify treatment, please tell us about the 20% of cases in which your total objectives are not completely attained. What happens in most of these 20%?
DR. TWEED: If I gave the impression that in the 20% of children for whom I could not fulfill the angular requirements of the diagnostic facial triangle--that their teeth looked just as bad as when I started--that was the wrong impression. There are times when patients present as much as a 20mm arch-length discrepancy, and obviously one cannot comply with the requirements of the diagnostic facial triangle. I will remove all four first premolar teeth, but I hesitate to remove more than four teeth. These 20% of the cases that we are speaking about are usually those individuals whose growth trends are Type B. In Type B growth trend cases it seems impossible to move B point forward, and the total correction must be made by moving the maxillary denture posteriorly. In many instances those patients for whom I have not completely fulfilled my desired requirements have beautiful dentures, and some have lovely faces, as I will demonstrate to you during your visit with me. It doesn't mean that the time has been wasted or that the child has received no benefit from her orthodontic treatment. In fact, some of these patients have good facial esthetics. Another point that I would like to impress upon the young man is regular observation and guidance of patients during and following retention. Why? To follow the growth processes of each patient and observe the aftermath of orthodontic treatment. A couple of years ago one of the students asked Francee, my indispensable assistant, how Dr. Tweed kept patients from coming back following the placing of retainers. He remarked, "We were taught at school, after you retain a patient charge them $5 every time they come back, and soon they will drop out of the practice." Miss Francee was aghast and mentioned the fact that wasn't one of our problems. Our problem is getting them back, because we like to follow each patient. The fact of the matter is, Sid, I have patients 55 years old who still come in to see me. When they visit with me I find time to take complete records. At the moment I am resuming my task of collecting 100 nonextraction cases and 100 extraction cases treated by me 25 years ago or longer. This permits me to observe the aftermath of my early treatment efforts. It is very heartwarming to see many of these patients with their lovely mouths and all of their teeth so many years after their treatment. At times the picture is quite the opposite, which makes one regret he started such a project.
DR. BRANDT: Have you gotten any more done on that? In your book you noted that you had this project approximately 25% completed. Is this any farther along, and have you any comments on what you have found to date?
DR. TWEED: The project is not further along, Sid, for the reason that I have been in the hospital for major surgery twice in the last year. Completing the details involved in preparing my book was quite a task, and I'm just recovering my health and have only begun to line up more of my former patients for complete records. I hope in the next three years I will be able to complete the project. My immediate ambition is to be able to have 100 nonextraction cases lined up on one bench and 100 extraction cases on another, and to be able to suggest that anyone interested can examine the display and draw their own conclusions. And I am sure one will find the extraction cases 20, 25, and 30 years later are much nicer than the nonextraction cases.
DR. BRANDT: Just to go back to the topic of stability. What is your opinion about the influence or influences of the muscles and musculature on the stability of a treated malocclusion?
DR. TWEED: I feel it is very important to the orthodontist. So much so, that I refer each one of my patients that comes to me for an examination to the therapist for the correction of any abnormal tongue, lip, sucking, or swallowing habits--for to me, unless such habits are corrected, the face cannot develop normally and as beautifully as would be the case if the individual were free from the adverse effects of these influences.
DR. BRANDT: How about other than tongue and lip--the muscles of mastication and some of the other musculature that's hidden? Do you think that these influence the stability of the treated malocclusion? And I could carry that just a step further--do the orthodontists alter any of their characteristics or change their balance?
DR. TWEED: Some questions I can't answer. Obviously, perversion of musculature has a bearing on the success of orthodontic therapy. One observes individuals who have had polio that has affected the musculature of one side of the face, with serious impairment of function. I would not attempt to answer the question of how much one can change musculature as a result of orthodontic treatment procedures.
DR. BRANDT: May we discuss a few specific problems that trouble so many of us practitioners? For example, if you had completed a diagnosis with models, x-rays, photographs, cephalometrics, or any other diagnostic tools you wish, and you found the patient in the mixed dentition, Class I molar relationship with a low FMA reading and crowded upper and lower incisors, what would you do? Would you start serial extraction procedures?
DR. TWEED: Sid, first of all I would have to have some more information. What is the arch-length deficiency? Is it 1mm or is it 10mm?
DR. BRANDT: Well, let's assume that it is somewhere in between, somewhere around 5 or 6mm where there is definite crowding and there seems to be a definite imbalance between basal bone and tooth structure.
DR. TWEED: If the tooth-basal bone discrepancy is 6mm or more, I certainly would begin a serial extraction procedure and eventually remove all four first premolars prior to any active treatment.
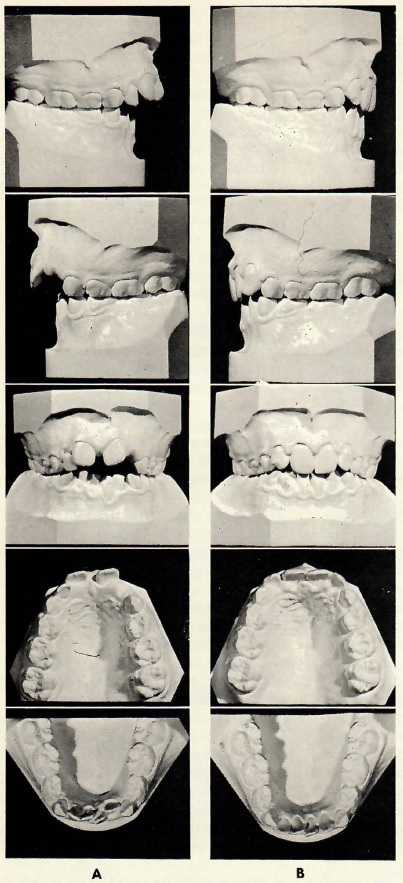
Fig. 2 A. Malocclusion resulting from thumb-sucking. Observe the beginning gum recession of the left mandibular central incisor. B. Same patient 10 months after stopping thumb-sucking. No appliances were used. (From Tweed: Clinical Orthodontics, The C.V. Mosby Co., St. Louis, MO. 1966).
DR. BRANDT: Supposing it was a Class II, division 2 malocclusion?
DR. TWEED: Individuals with Class II, division 2 malocclusions as a rule present pronounced pogonions that will increase in size during the remainder of the growth period. Whether treated as extraction or nonextraction cases has little effect on the size of pogonion. If one does not remove dental units there will be a development of irregularities of the teeth following discontinuance of retention, and the patient will have received little benefit from treatment. In addition, pogonion remains prominent. On the other hand, if teeth are removed and care is taken in treatment, and the mandibular incisor and cuspid irregularities corrected, leaving these teeth as far forward as functional balance will permit, the patient will at least get some benefit from treatment efforts. The overabundance of pogonion will be the same in either instance. Surgical reduction of pogonion can be accomplished later if warranted. In borderline discrepancy cases of 2 or 3mm, the orthodontist should take a long second look before the decision is made to remove dental units.
I do think the orthodontic profession has been a bit remiss in not investigating surgical procedures for these types of individuals. I do know of several instances where there has been a sizable surgical reduction of the pogonion that has benefited the patient tremendously.
DR. BRANDT: Now I want to ask you a few things about actual tooth movement. Would you be good enough to describe your torquing technique? And in that you might think about answering how you decide when there is sufficient torque. Is there a critical cephalometric angle that helps you arrive at your decision, or is it purely on clinical evaluation, or both?
DR. TWEED: Sid, you bring up an important point. Torque can be both good and bad. The diagnostic facial triangle analysis is completely meaningless if root apices of the mandibular incisors are displaced. Every effort at our command is made to maintain the position--the original positions--of these root apices. When torque displaces mandibular root apices, either labially or lingually, the diagnostic facial triangle as a treatment guide becomes meaningless. I can recall one young man in my office years ago who really thought his patient was responding beautifully to treatment. He had torqued the incisor root apices through labial cortical plate. "Look, Dr. Tweed, what I have done so fast for my patient. She has an FMIA of 79°." When I finally moved the root apices back to where they belonged, she had an FMIA of 44°. Torque in the incisor areas--both maxillary and mandibular--is very important. For instance, in Class II, division 1 cases there is usually an extrusion of both mandibular and maxillary incisors. An effort is always made to parallel the long axes of the maxillary incisors with the anterior curvature of hard palate and intrude these teeth. A tremendous amount of lingual root torque, together with high-pull headgear, is necessary to accomplish such movement. Torque is used in the buccal segments to correct buccolingual inclinations of these teeth in typical, classical Class III cases. When anchorage is prepared in the mandibular arch, slight progressive lingual crown torque is placed into the archwire from cuspids to terminal molars to enhance anchorage if slight mobility of mandibular molars is discerned. The torque is never enough to move these anchor molar teeth into abnormal axial inclinations.
DR. BRANDT: I think the profession would appreciate a clarification of distal movement of maxillary teeth. As you know, this is somewhat controversial. You describe distal movement of the maxillary denture, usually recommended in those individuals having favorable growth trends A or C. Specifically, how far do you move these maxillary teeth? Where do the molars go? And does the maxillary dentition ever slide forward again either during treatment or after retention?
DR. TWEED: Sid, the necessity of moving the maxillary denture distally applies in the main to Type B growth trend cases. In Type C growth trend cases where the mandible or lower face is growing forward more rapidly than maxilla or midface, it is obvious that distal movement of the maxillary teeth is not so appreciable. In Type A growth trends in which middle and lower face are growing forward in unison, there are times when there is considerable distal movement of the maxillary teeth that must be made. I allude to those cases in which B point does not move forward appreciably during treatment. The cases that require distal movement of the maxillary denture are usually those individuals who are cursed with a Type B growth trend. In these types of cases, the third molars are removed before any attempt is made to move the maxillary denture distally. How much? It would be a guess if I venture to tell you how much we can move the maxillary denture distally. I would say a matter of 3-4mm. In these most difficult of all cases to treat, it is not unusual to move the maxillary incisors bodily distally the breadth of a maxillary incisor, maintaining normal axial inclinations of these teeth.
DR. BRANDT: Your book illustrates various types of headgears for the variety of malocclusions. I know you vary the amount of tensions in these headgears. Just for general information, how do you measure the tension? Do you have any special formula or instrument for that?
DR. TWEED: Sid, I have never measured the pressures we use for headgears, but I would surmise that the amount of pressure would vary from 12-16 ounces.
DR. BRANDT: Now I would like to get onto another problem that we run into so often. Do you find tooth movement in open-bite cases different from tooth movement in closed-bite cases? If so, how?
DR. TWEED: Sid, if I understand you correctly, the procedure that I advocate in open-bite cases is utilizing vertical intermaxillary elastics in the anterior quadrant of each dental arch, and in a closed bite I open the bite by uprighting of the molars in the buccal segments using intermaxillary elastic mechanics. I would like to say a word about open-bite cases. There are two kinds of open-bite conditions. I think it is important to the young man to be able to differentiate between them. One observes an open bite that begins at the second molars, with a "piece of pie" shaped opening of as much as a half-inch in the incisal area. My advice is to take a long second look at the throat. If the patient is devoid of gagging reflexes, beware. It has been my observation that when this type of open bite occurs, it is the result of an abnormal swallow over which the patient has no control. In such cases, it is impossible for the individual to swallow normally. This condition can result from faulty surgical procedures in the removal of tonsils, or may also be the result of polio or some serious childhood disease that paralyzed the throat muscles.
In these cases, correcting archform and rotation of teeth as well as closing the bite with intermaxillary vertical elastic force is done with ease. Not so maintaining closure. The reason being that during the first stage of deglutition, the bolus of food is driven back into the fauces by the pressure of the tongue against the hard palate. After leaving the tongue, the bolus passes on. The glossopalatini, which are the constrictors of the fauces, contract behind the bolus. The pharyngopalatini then contract, pulling the pharynx upward over the bolus, and come nearly together, the uvula filling up the slight interval between them. By these muscular actions the food is prevented from passing into the nasal part of the pharynx or regurgitating back into the mouth. Whenever the glossopalatini and the pharyngopalatini are mutilated or paralyzed to the extent that the fauces do not close during the act of swallowing, the base of the tongue must be pressed against the hard and soft palate to prevent the bolus of food from regurgitating back into the mouth. When the tongue must substitute for normal throat muscle function, the tongue is forced between the maxillary and mandibular cutting edges to maintain a seal. The tongue in such position becomes a fulcrum, and the upward and backward pull of the masseter muscles usually everts the body of the mandible as well as intruding the incisors.
Don't confuse the type of open-bite condition just described with the usual type observed by all orthodontists who deal with children and their thumb, finger, and tongue bad habits. When the open bite is confined to the incisal area and the teeth in the buccal segments are in occlusion from the cuspids posteriorly, the problem is one of discontinuing some bad habit. If the patient is young enough and first molars are in Class I occlusion, discontinuance of the habit will result in self-correction of the open-bite condition.
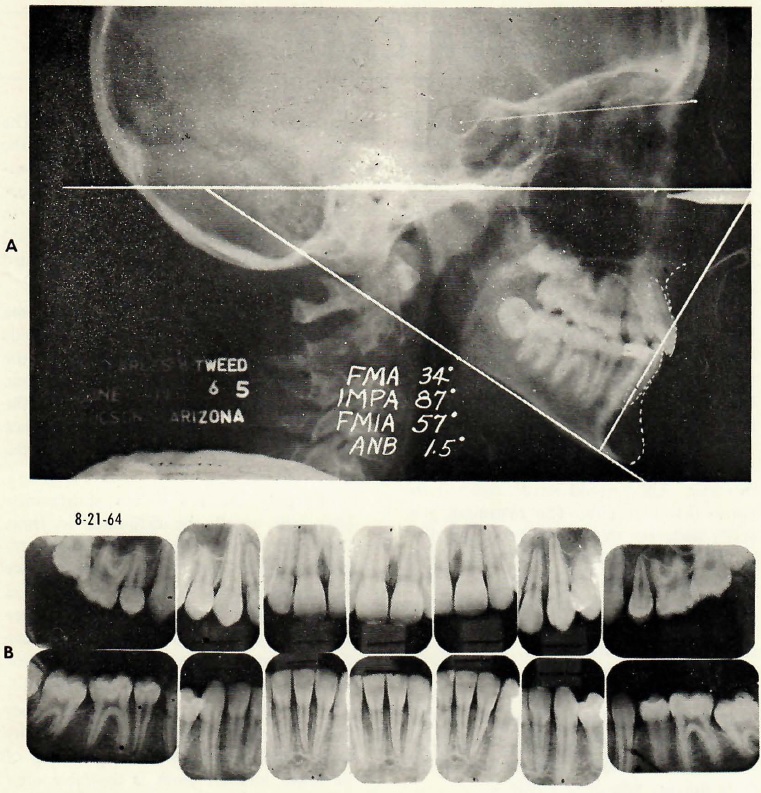
Fig. 3 Typical post-treatment radiographs. (From Tweed: Clinical Orthodontics, The C.V. Mosby Co., St. Louis, MO. 1966)
DR. BRANDT: Let me tie in another problem associated with tooth movement, and that is root resorption. Would you care to comment on its incidence, what you think causes root resorption, and any other comment you may have on this great problem?
DR. TWEED: In the early days of my practice, when it was necessary for me to retain my patients after seven months of treatment and then resume treatment following their return to Tucson after the summer months, I observed that I had a minimum of root resorption. This suggested that it would be in order to endeavor to find out when root resorption begins, what caused it, etc. I was prompted to select 25 patients whose buccal segments were x-rayed every two weeks from the date appliances were placed. My observations were that beginning root resorption varied in different individuals. For instance, I found that underweight or average-weight children demonstrated less root resorption than obese children. I observed that length of treatment had a bearing on root resorptions. Also that tooth movement that torqued tooth roots against the cortical plates was conducive to root resorption. Macroscopically, I rarely detected root resorption prior to the seventh month of treatment. Thereafter it seemed to increase in intensity in proportion to length of treatment time and the age of the patient. At the time of this experiment I was using round .022" gold archwires, and I have a definite feeling that the jiggling permitted on these teeth by the use of a frail wire had a lot to do with root resorption. One of the most satisfying developments of the past 15 years of my orthodontic career has been the minimum of root resorption in my practice. I attribute this to the fact that I have limited my practice to mixed dentition treatment and, in addition, to a change in mechanics in which I have practically eliminated jiggling of the teeth by using less round wire and more rigid square wires to binds groups of teeth into stabilizing units that do not permit jiggling. Since I have decreased treatment time by limiting my patient load to less than 100 patients, I can honestly say that root resorption has been no problem in my practice during the last 15 years. I refer my readers to the two volumes on Clinical Orthodontics recently published in which I included after-treatment intraoral x-rays.



