JPO Interviews Dr. Irving D. Buchin
[show_img]62-jco-img-0.jpg[/show_img]
Irving Buchin is one of the world's most respected clinical orthodontists. He is an Instructor at the Tweed Foundation and Associate Professor of Orthodontics at the Boston University Graduate School of Dentistry. He is Chairman of the Qualifying Committee of the Northeastern Society of Orthodontists, Diplomate of the American Board of Orthodontics, Fellow of the American College of Dentists and Secretary of the Eastern Component of the Angle Society of Orthodontia. He has a total commitment to the treatment of the orthodontic patient and the advancement of the art and science of orthodontics.
JPO visited with Dr. Buchin in Forest Hills, New York, to find out his approach to the treatment of orthodontic cases and the management of and othodontic practice. This article is the first of two which will present a dialogue of that visit.
Case Load
Dr. Buchin, do you feel that an orthodontist should limit the number of patients in his practice?
Yes, he should restrict his practice. If he takes everyone who walks in, then he is just in business to get patients. By overloading himself, he limits what he can do for the patients, and he is going to be unhappy.
How Many?
Do you have a number of patients in mind that an orthodontist should carry?
I feel very strongly that an orthodontist should carry no more than 110 to 115 patients, as I assume he is providing complete optimum professional care. And I am being generous. Unless you are the type of person that closes both eyes and takes off the appliances when it comes time to finish the case, you are going to have problems if you accept more than 40 patients a year. No matter how you are practicing, you will have a certain number of holdovers and this will further add to your patient load. When you set out with certain objectives and you make yourmind up that you are going to reach those objectives, if at all feasible, you are going to have to work very hard. If you are willing to work five or more days a week, than perhaps, you can take on more than forty patients per year. This figure does not include the observation preorthodontic guidance patients. But, I do not want to work more than four or four and a half days a week. I want a day off so I can either teach, or do nothing, or think, or do organization work, or go shopping, or play golf, or spend time with my family. Then again, there are other factors. If you take on more than 115 patients, how can you x-ray them periodically? How can you sit down and think about the cases and know where you are going? How can you technically keep them on the right road? How can you supervise them adequately? I can tell you that with my practice, which is approximately 110 to 115 strapped-up patients, I have my hands full keeping every one with tight bands, wearing headgears, keeping the teeth clean and making changes which are necessary. Of course, the Tweed technique that I am using is a disciplined technique that requires chair time. Maybe with other techniques you can handle a larger number of patients, but I am not convinced that you can get better results. I decided years ago that I was going to practice for the greatest good for me individual, ratherthan for the greatest good for the greatest number. I have to suit my practice to my personality, not the other way around. Some of us should run General Motors, some are administrators and they make good administrators in their practices. And some are just the workers. I am just a worker.
Daily Work Schedule
What is your daily work schedule?
A routine day in my office will have approximately three to four patients who are brought in from 9:15 in the morning to 3 in the afternoon. They can bring their lunches to the office or go out to eat. Assemblages are constructed and inserted or major changes in the appliances are made. Routinely, approximately ten to twelve patients are brought in from 3 to 5:30 for regular adjustments. The majority of my patients leave the city for the summer, and consequently, June and September are particularly difficult months. June is spent in preparation for long adjustments and September in routine intraorals, cephs, evaluations of patients under treatment, as well as starting new patients.
Accepting Patients
What standards do you have for accepting a patient?
First, the patients should be mature enough so that you can work with them. Second, you must legitimately be able to help them. And third, you should not waste your time.
There are some problems that should not be treated. For example, one rotated tooth and a good face, or a minor habit which is not causing any pathology to the dentition. If a patient comes in with a deviate swallowing habit, I think he should get swallowing therapy first. If the child looks esthetically good and has a slight rotation of anterior teeth, I do not think you should treat him. The scarring of treatment could be worse than the slight improvement.
You have to remember, I have a different approach to this question. I have been influenced by people like Bob Strang and Charlie Tweed who have preached about conducting their practices in a personal professional relationship where rapport between the patient and the orthodontist is important in motivating the patient to cooperate for good orthodontic results. This implies a good personal relationship between the doctor and the patient, which I am not certain you can achieve as well in a time-saving, efficiency-planning type of practice.
Qualifying Patients
What do you mean when you say that you qualify a patient?
Qualifying patients is a very important thing. It is a step that is tied in with diagnosis and treatment planning. Before taking an irreversible action, such as the removal of teeth, you must be certain that you can fulfill your treatment objectives. That means you may need the patient's help or cooperation. Qualifying a patient is his demonstration or performance for you that determines his dependability in carrying out your tasks. For example, you may decide that you should take out upper second molars. Before you do that, you must qualify the patient as to whether he will wear headgear. If you take out the upper second molars and the patient does not wear the headgear, the third molars drop down to the second molar position, the first molars are not moved back and all that you end up with is two less teeth. If the patient does a good job of wearing headgear to the first molars for about two months, then you know that he is dependable. Then go ahead and take out the upper second molars. You will get a good result. That is one way of qualifying a patient orthodontically, based upon cooperation. But I also want to be sure that the patient will fulfill obligations such as using his toothbrush, and keeping his month clean, showing up for appointments, and being on time. This too is qualifying a patient.
Ceph Analysis
What do you look for in a cephalometric film?
I look at the overall pattern, first. In other words, I start off by saying, "Is this a good face, a good skull?" You notice that I start off by looking at the face. The skull and the angles themselves are nothing more than a scaffold for what I wish to end up with--and that is a good face.
Mandibular Plane
Are the palatal or mandibular plane of any importance in your evaluation?
All of the relationships are important to analysis and I do not want to choose any one more than the other. My orientation is based upon the Tweed Diagnostic Triangle, the relationship of the facial line to the anterior part of the profile, and the ANB difference. I do not want to single out any specific criterion mat I am influenced by, but, if I were to do so, it would be the FMIA. But here again, I have broken a few rules although the great majority of beautiful faces have FMIA of 60° or more.
Cant of Occlusal Plane
Do you check the cant of the occlusal plane?
It is only in the past two years that I have made a careful evaluation of the changes in the occlusal plane as a consequence of treatment. Tipping of the plane is to be avoided in average to high FMA, but I am not concerned too greatly if it tips in low FMA problems.
Deep Bite
What is the role of deep overbite in analysis?
Deep overbite is only one of the criteria that I take into consideration as to whether to extract or not. But, I will extract in a deep overbite case. Though it is an important consideration, it would not prevent me from removing teeth if other considerations indicate it.
Individual Norm
Are you now analyzing toward an individual norm rather than an average norm?
No, I am not.
Tweed Analysis
Do you follow Dr. Tweed's analysis, extracting automatically where the IMPA is greater than 96°?
Nothing is done automatically in diagnosis or treatment planning. However, I go along, basically, with Dr. Tweed's evaluation of the IMPA, and I consider other factors, which he does as well. But let us not misquote him. I think that he says that the great majority of cases where the IMPA is over a certain amount, whether it is 96 or 95, he will extract. However, the great majority means that there are exceptions. In these exceptions, we use our judgement and experience to decide which rules to break. It is not fair to predicate conclusions on the basis of exceptions. Certainly one is not eager to remove teeth in flat angle cases regardless of the IMPA. In my office, on the great majority of cases which will present themselves with over 96 IMPA, you can rest assured that I will take teeth out if the other considerations indicate it: e.g., FMIA, FMA, anchorage requirements, ANB difference, overbite, facial aesthetics, etc. The great exceptions would be, for example, if I had a child with a potential for a large chin point, a large nose, and the facial line falls through or forward of the lingual surface of the lower anteriors, I may feel that for that particular patient, the dentition was well-oriented to the pattern. If me patient had an FMA of 19 or 18°, or less--a flat angle case--I try to avoid extraction procedures.
Role of Esthetics
What do you feel is the role of esthetics in case analysis?
Facial esthetics is one of the most important considerations and does not play a secondary role in patient evaluation. Of paramount importance is the health of the investing tissues. But, I do not think that this becomes our big criterion since most of the children who come to see us have fairly good investing tissues. I always look at the patient's face and say, "Can I improve it? Can I keep it the way it is, or can I, perhaps, make it look worse?"
Cosmetic Surgery
What do you feel is the place of cosmetic surgery?
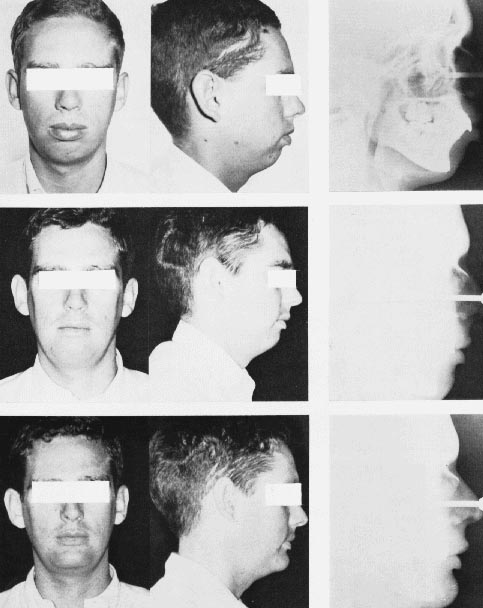
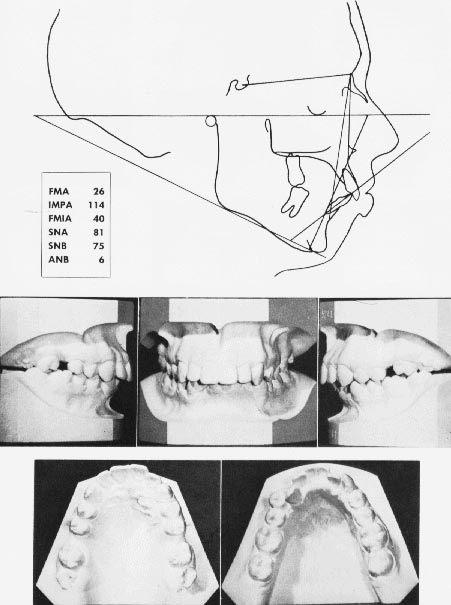
I have seen marvelous things that can be done and I have had many of these in my practice--rhinoplastics, genioplastics, bone grafts. I am a great believer in esthetics. The job is only half done when we get the teeth back and the patient does not have a well balanced face. Here is a case that is interesting and in which the plastic surgeon--in this instance, Dr. Richard Boise Stark of New York--made a great esthetic improvement for my patient after I had done everything that I could for him orthodontically.
I get a great many transfer cases and this was one of those. It was a tough one. I worked very hard and he was an excellent patient. We got a real satisfactory result. Not perfect. But look at the original condition and I think you will agree that we got the teeth back quite well. Look at the cephs. They tell you some of the story. Even though the cephs look good, look at the middle photos of the case at the conclusion of orthodontic movement. It was at this point that I referred my patient for a genioplasty. An iliac bone graft was made from the left hip. You can see it in the cephs and on the tracing. Now look at the final photographs. This is the kind of esthetic improvement that cosmetic surgery can accomplish.
Extraction Percent
In what percent of cases do you extract teeth?
About 80%. This is an approximation and probably varies from year to year. But, we must remember that when an orthodontist first opens his office, the percentage of extractions will be less because he doesn't get as many extreme problems. I am referring to an area where there are many orthodontists. He will get a more diversified type of case selection. A man who has been in practice a longer time, will get a different type of case sent to him. He will get more extreme types. I feel that in this office, the percentages perhaps would be higher on extractions.
Discrepancy
How much total discrepancy would cause you to extract?
Anything from 4mm of discrepancy, in my office, is an extraction case, other factors not prohibiting it. Let me say this, I eyeball the case unless it is a question of a borderline case. But, where the discrepancy is greater than 4mm, I will extract. I know that others may go up to 5mm, but this has to do with concepts of anchorage, with faces, and perhaps with the degree of patient cooperation we can get. In some cases, if the ANB difference is very large, or the facial pattern is poor, or there are other extenuating circumstances, the extraction choice may even be predicated on a 3mm discrepancy.
Compromise
Where the total discrepancy is greater than the width of a bicuspid on each side, how do you attain your treatment objectives?
We have to compromise our objectives. But frankly, I do not think that the degree of compromise should be such that it is a crutch to lean on or an excuse for faulty mechanics. If I have to compromise where I need more room, I will use various techniques--stripping of lower anterior teeth, rotating of lower canines--to decrease the amount of arch length that we will require. I try not to do it at the expense of facial esthetics. In other words, I will accept a slight crowding in the low anterior region rather than create a bimaxillary protrusion. You will note that I do not expand the arches to create room for alignment of the teeth. Also, excessive distal retraction of molars often impacts the wisdom teeth, which only results in an extraction case when the patient is eighteen or nineteen years old.
Tooth Size Discrepancy
What about a discrepancy of tooth size?
I might take out second premolars in one jaw and the first premolars in the other to adjust a discrepancy. I also strip.
Molar Extraction
What about molar extractions?
I do not do too many of them. I am opposed to eight teeth extractions--first bicuspids and first molars. I am willing to fight for what I want to attain, but, to end a patient up with eight less teeth at the age of 14 is something that I would not want done for my child. If I would not want it done for my child, I do not want it done for my patients.
No Routine Band Removal
Do you remove appliances for caries checks when a dentist requests it?
No, I do not. I think that there is a definite avenue here where we have to work with the dentist. But someone has to assume command. Who should it be? It should be the orthodontist because he is seeing the patient frequently. The dentist is not. But, at the same time, the dentist should fulfill his responsibility of recall and consultation with the orthodontist. Once a mouth is cleaned up, then it is up to the orthodontist. Before cementation, I use sodium fluoride gel if I find that the family dentist has not done so or if he does not believe in it. I do it myself. If the child has a high caries index, keep the bands on as short a period of time as possible and take certain precautions in putting the assemblage in. Do not cement a half dozen bands at one time. Cement two at a time and recement the upper anterior bands and anchor molars during treatment. Also, make sure that the patients follow through with your prescription of no taffy, butterscotch, caramel, chewing gum, or refined sweets. And make certain that they brush their teeth. Have them come into your office with an assigned office toothbrush to see that they brush their teeth and appliances properly. I take great pains in the care of the teeth, but I do not remove appliances for periodic check-ups.
Periodic X-Rays
Do you take periodic x-rays?
After the summer, as a rule, I take six intraoral x-rays on every patient (one upper anterior, one lower anterior, and a buccal segment of the four sides) and a progress cephalometric x-ray. I look for any degree of root resorption. By taking these films, I have found things that would surprise you--an area around damaged anterior teeth, calcification of a canal, a residual root. Taking progressive x-rays is one of the most rewarding routines that is exercised in my practice.
Root Resorption
What do you do when you find root resorption? Does it change what you planned to do?
Usually not, but, pathology can change my treatment plan. Let me say this, if I had an extensive amount of root resorption, I would stop what I was doing, take further records and call the parents in for consultation, as well as notification of the family dentist. Minor blunting does not mean anything, because the tooth is still healthy without any detriment to its overall longevity. But again I say, use torquing procedures properly and do not utilize round wires extensively for retraction of anterior teeth. This causes the root apices to move against the labial cortical plate and perhaps results in root resorption. I also routinely record the resorption and I will ask the patient if he is wearing the elastics and headgear as I instructed. I will point out that the roots are blunted and that they should be careful to do exactly as I tell them. But frankly, root resorption is not a problem in my practice since its incidence is of relatively minor occurrence.