Post-COVID-19 Clinical and Management Guidelines for Orthodontic Practices
JAE HYUN PARK, DMD, MSD, MS, PhD*
JANET H. KIM, DDS
ALAN KAI, DDS
LEAH ROGOWSKI, DMD
ANDY LIU, DDS
The COVID-19 global pandemic presents a unique set of challenges for the future of orthodontics. All aspects of the orthodontic practice have been impacted. Special considerations have been placed on procuring the proper personal protective equipment (PPE), ensuring the safety of all individuals, and operating under the legal ramifications of new regulations. As states allow dental practices to reopen, there have been numerous concerns and questions from clinicians about how they can best equip their practices with the necessary tools to succeed in this unprecedented time. Few of these recommendations have been specific enough to meet the needs of the orthodontic setting.
The disarray caused by the global transmission of COVID-19 has called into question current infection-control protocols of medical and dental practices. Identification of COVID-19 surface receptors shows COVID-19 virions have the potential to infect oral epithelial cells,1 placing oral health-care practitioners in the spotlight for minimizing the spread of disease.2 Although orthodontists perform many procedures that do not generate aerosols, proper attention must be paid to reducing sources of contamination in the orthodontic office.3 For many orthodontists, the majority of patients seen are children and teenagers, who are susceptible to COVID-19 infection.4 Furthermore, orthodontic offices are designed to accommodate large volumes of patients at a single time, potentially increasing the risk of transmission if patient safety protocols are not adhered to.
As new information surfaces every day, the recommendations and guidelines that practices follow will need to evolve as well. Considering the current, rapid change in our understanding of the characteristics and spread of COVID-19, coupled with the evolving regulatory aspects of reopening the economy, the recommendations presented here are intended to serve as a malleable framework of practical information for each individual orthodontic practice moving forward.
Practice Modifications
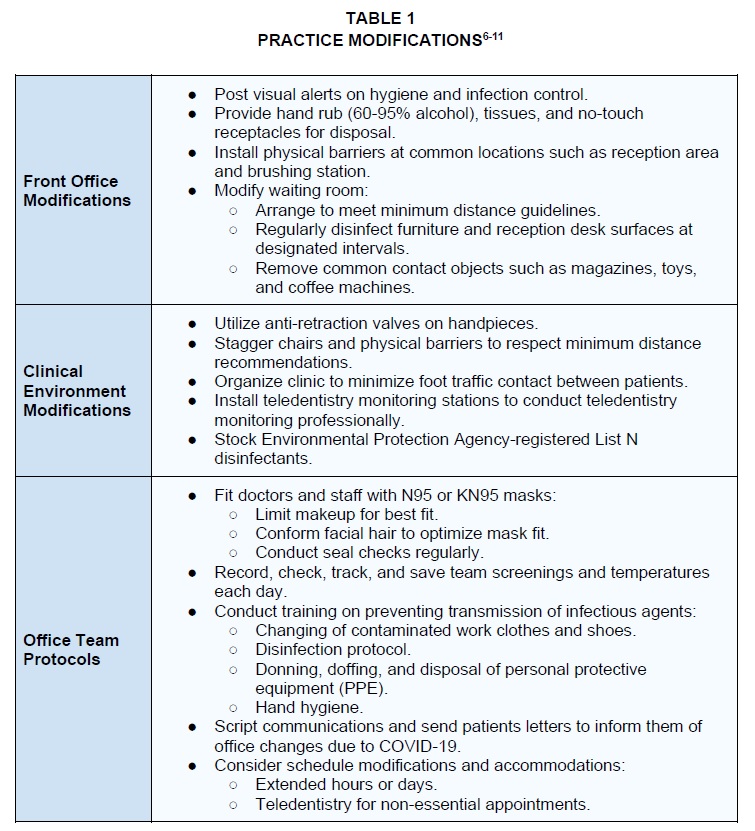
In the context of the COVID-19 pandemic, many orthodontists will find themselves asking what modifications to their practices must be made to meet new Occupational Safety and Health Administration requirements for infection control. These modifications are intended to
maximize not only the safety of staff, but also the safety of patients and parents who enter the practice. A sample employee screening log has been provided by the AAO.5 Table 1 shows practice modifications that include physical office changes as well as additional training for staff procedures.6-11
Clinical Modifications
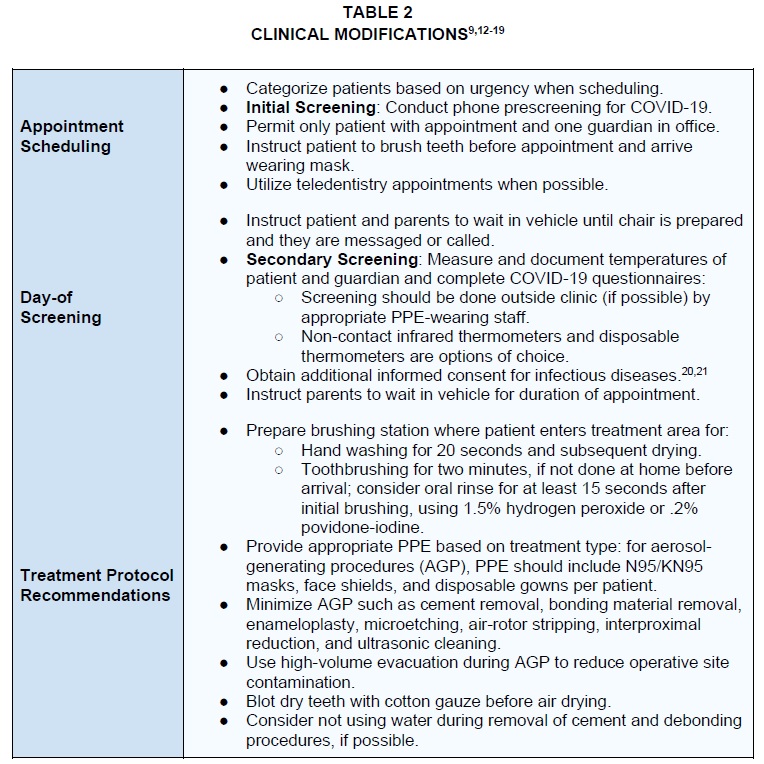
Modifications to patient treatment are designed to minimize the risk of COVID-19 spread in the office (Table 2).9,12-19 Many of these recommendations are related to prudent screening of patients as a form of risk assessment, as well as to minimize chairside viral contamination from patients with subclinical infections. The AAO has provided sample COVID-19 questionnaires and has updated its informed-consent recommendations to include the transmission of infectious diseases.20,21
Patient Categorization
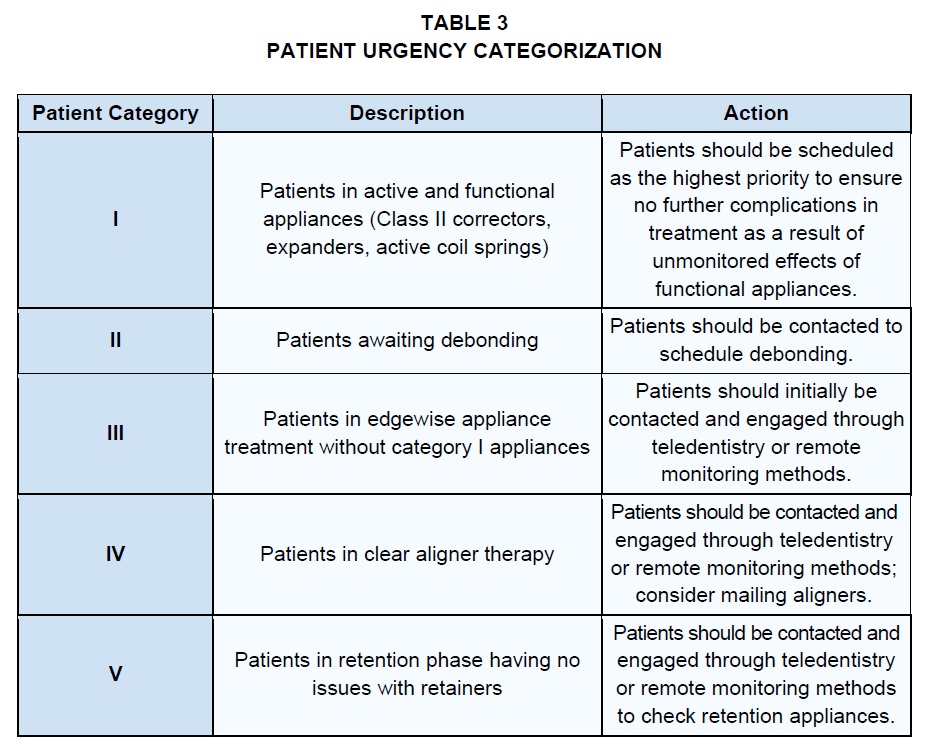
Many patients are anxious to be treated after not being seen during the initial COVID-19 pandemic shutdown. The authors recommend a patient urgency classification for all active patients to provide a clear rationale for the order in which they should be scheduled (Table 3). Although true medical emergencies are rare in the orthodontic office, lack of patient monitoring and the possibility of broken appliances could extend treatment time.22 True orthodontic emergencies take precedence in these classifications; the orthodontist should decide whether emergencies should be resolved palliatively or comprehensively, since the complete resolution of orthodontic emergencies often requires the use of aerosol-generating procedures (AGP).
Patient Communication
Communication scripts are highly recommended to ensure clear communication of office protocol and the changes that have been made to reassure patients that they are valued and that their safety is of the highest priority. The ADA has provided a “Return to Work Interim Guidance Toolkit” that includes a sample letter to emphasize the office’s commitment to maintaining up-to-date modifications in infection control and changes to office scheduling, appointments, and policies.23 All patients should be required to bring their own face masks for the protection of themselves and others. A prescreening questionnaire for COVID-19 should be conducted at the time of the appointment scheduling.20,23,24 On the appointment day, the patient is to wait in the car until instructed to enter. The patient will again be asked to complete the COVID-19 questionnaire and will undergo a temperature check.23 Treatment should be postponed if the patient reports any signs or symptoms consistent with COVID-19.25 Before entering the treatment area, the patient will be instructed to brush (if not already done at home), utilize an oral rinse, and exercise the handwashing protocol. Additional people entering the clinic area should be restricted to those essential for the patient’s physical or emotional well-being and care.
Teledentistry is a useful strategy for minimizing face-to-face contact, avoiding unnecessary trips to the office, and assessing orthodontic progress.26,27 Video conference calls can be used to determine the urgency of an appointment, address non-urgent needs, and provide a platform for virtual consultations, clear aligner checks, and retention checks. Such appointments can also be completed virtually, outside of clinic hours. Resolving non-urgent needs through teledentistry is highly recommended because it promotes social distancing and reduces the risk of unnecessary exposure.
Importance of Social Distancing
In view of COVID-19’s high infection rate and lack of definitive treatment, social distancing and isolation have become best practices in preventing the spread of the virus.28 Nevertheless, social distancing is only as effective as the risk attitudes of the susceptible population. Risk-averse attitudes will limit the spread of infectious disease, but they can be offset by more lax attitudes.29,30 It is essential to continue social distancing in the workplace environment even after lockdown and stay-at-home orders are lifted. A systematic review found that effective social distancing in the workplace resulted in a median reduction of 23% in the peak influenza attack rate.30
The AAO’s interim guidelines state that dental operatories should implement social distancing protocols by seating patients at least six feet apart.31 These recommendations pose challenges to orthodontic offices because they will not be able to operate at full capacity by utilizing all their chairs. To compensate for the increased patient demand and lost treatment time, offices may need to extend clinic hours and prepare additional staff for the initial few months after reopening.32
Infection Control
As our understanding of COVID-19 transmission has improved significantly in parallel with the progression of the pandemic, clinical protocols have evolved to maximize the chances that we can reenter practice safely and effectively. While orthodontists may not be performing as many AGP as their other dental colleagues are, it is still ultimately important to understand the rationale behind updated safety guidelines.
Dental white coats are frequently contaminated in the chest, pocket, and sleeve regions by splatter from blood, aerosols, or saliva, posing the risk of cross-contamination between patients.33 Because of the possibility of contamination of clinic attire, the authors recommend that doctors and staff arrive at the clinic in street clothes, change into clinic attire for the workday, and change out of clinic attire before leaving the office.
Although orthodontic practices perform relatively fewer AGP per patient, the complete elimination of aerosols is impossible.34 Regardless of handpiece speed or the presence or absence of water coolant, aerosols are still produced in the orthodontic setting and can be inhaled and deposited in the conducting airways and terminal bronchi of the lungs.35 Therefore, proper PPE is necessary depending on the health status of the patient and whether AGP will be performed. Well-fitted N95 masks and disposable gowns are recommended to prevent inhalation and contamination, respectively, during AGP. Many clinicians are concerned about the limited supply and variable costs of masks, both surgical and N95. The Centers for Disease Control and Prevention has published a protocol for disinfecting and reusing masks in crisis shortage situations, but does not condone the use of disinfected N95 masks for AGP.36 Face shields are recommended to prevent contamination of operator masks or autoinoculation from face touching.37,38
Concerning preoperative oral rinses, many clinicians have inquired about the use of .12% chlorhexidine gluconate (CHX) rinse, which is readily available and demonstrates reduction of microbial activity.16 It should be noted, however, that CHX does not demonstrate virucidal activity, and the ADA does not recommend its use to reduce the likelihood of COVID-19 transmission.15 Furthermore, although 1.5% hydrogen peroxide and .2% povidone-iodine rinses have shown virucidal activity in vitro,13 inactivation of virions in the oral cavity has no effect on virions in the respiratory tract. Therefore, while oral rinses are promising for the reduction of viral activity in the oral cavity, they by no means eliminate the risk of COVID-19 transmission.15
Orthodontic offices produce significant sources of cross-contamination through the reuse of materials such as archwires and brackets.39 Orthodontic archwires should not be reused unless they have been sterilized. Other potential sources of patient-patient contamination are bands that have been tried in, photography mirrors and retractors, burs, and markers. Special care should be taken to ensure these items are properly sterilized before reuse. Disposable supplies are another alternative.
Human Resource Management
Even though a health-care worker knows there is an inherent risk involved with patient care, it is the orthodontist’s duty to minimize this risk. Employers may screen employees for symptoms consistent with COVID-19 and may request daily temperature checks before entering the workplace.40 Because the information obtained in such screening, including the employee’s temperature, is considered a medical record, the employer must maintain the confidentiality of this information.40
To accommodate the backlog of appointments, many offices will opt to extend their hours. It is important to understand new Department of Labor regulations when doing so. Under the Federal Fair Labor Standards Act, any employee who works more than 40 hours a week must be paid time and one-half unless characterized as exempt.41 An employee is exempt only if earning more than $47,476 per year, or $913 per week, and if performing duties in one of several categories.41 For example, an employee may be considered exempt if he or she regularly aids in management functions or supervises two or more full-time employees.41
Some employees may request sick leave or paid expanded family leave under the Families First Coronavirus Response Act passed on March 18.42 Active employees of covered employers are eligible for42:
- Two weeks (up to 80 hours) of paid sick leave at the employee’s regular rate of pay when the employee is unable to work because of being quarantined and/or experiencing COVID-19 symptoms and seeking medical diagnosis.
- Two weeks (up to 80 hours) of paid sick leave at two-thirds the employee’s regular rate of pay when the employee is unable to work because of the need to care for an individual subject to quarantine, or to care for a child under age 18 whose school or childcare provider is closed or unavailable for reasons related to COVID-19.
- Up to an additional 10 weeks of paid expanded family and medical leave at two-thirds the employee’s regular rate of pay when an employee who has been employed for at least 30 calendar days is unable to work because of the need to care for a child whose school or childcare provider is closed or unavailable for reasons related to COVID-19.
Employers with less than 50 employees may be exempt from this ruling as long as they meet one of these three conditions42:
- Sick leave would cause “the small employer’s expenses and financial obligations to exceed available business revenue and cause the small employer to cease operating at a minimal capacity.”
- Sick leave would “pose a substantial risk to the financial health or operational capacity of the small employer because of their specialized skills, knowledge of the business, or responsibilities.”
- The employer “cannot find enough other workers who are able, willing, and qualified, and who will be available at the time and place needed, to perform the labor or services the employee or employees requesting leave provide, and these labor or services are needed for the small employer to operate at a minimal capacity.”
The Department of Labor requires employers to document and retain files for four years proving the employer falls under one of these criteria.42 If an employer is still not exempt, there are tax credits available to help offset this financial burden.43
Bringing Employees Back
Orthodontists should proceed with caution when bringing staff back upon reopening their practices, especially if not all employees will be asked to return to work initially. Proper documentation of objectives and rationale for bringing back certain employees—such as seniority, skills, or quality reviews—is necessary to avoid perceived discrimination.43 This is not a time to weed out unwanted employees; every decision must be methodical and documented.43
Because of their passive income during unemployment, the fear of potential exposure, and the lack of childcare, employees may not readily agree to return to work.43 Some states have laws against collecting unemployment if a worker has potential job offerings and is willingly turning down employment.43 In cases where there are no such laws, practice owners are forced to either rehire and retrain new employees or incentivize their employees to return.
Some employers have offered disaster relief pay, while others have offered a higher wage for a predetermined amount of time in return for working under these harsh conditions. Doctors who have extended their hours but have a reduced patient load may implement split schedules allowing staff to work fewer days. Finally, orthodontists should consider letting some employees work remotely by answering calls, ordering, or billing.43 Special consideration will need to be given to employees who are hesitant to return because of underlying mental illness or medical conditions that make them susceptible to COVID-19.43 It is important to listen to each employee’s concerns and make reasonable accommodations if possible.40
A general desire not to work until after the pandemic without a preexisting medical condition can be treated as a resignation.43 Other employees may desire to work but will be unable to because of a loss of childcare.43 In these instances, it may be prudent to allow employees to take their allotted time off, work remotely, or work different hours.43 CEDR Solutions suggests holding positions for such employees until they can return, since discrimination laws protect the childcare status of potential new hires.43
Financial Management
According to Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, there will be an inevitable second wave of COVID-19 in the fall when the weather cools.44 Dr. Robert Redfield, director of the Centers for Disease Control and Prevention, stated that this second wave could be even more catastrophic than the first because of the combined impact of annual seasonal influenza.45 Amid such extreme uncertainty, orthodontic practices need to develop sustainable financial plans.
Orthodontists’ primary revenue comes from initial payments (patient down payments, paid-in-full accounts, and initial insurance payments) and contracts receivable (patient monthly payments and insurance continuation payments).46 Even considering the lack of patient starts during the pandemic, an orthodontist may not have immediately felt a drop in cash flow, since more than half of the practice’s monthly collections probably come from contracts receivable.46
Moving forward, orthodontic offices should be prepared for a strain in cash flow caused by the lack of new starts as well as additional expenses in personal protective equipment and disposables, advertising, marketing, and consulting.47 Cain Watters & Associates anticipates that “assuming the practice returns to average start levels in the third month after the shutdown, the overall profit will still be 25% lower than pre-shutdown levels,” and advises doctors to “continue to be mindful of expenses and overall cash flow as the practice returns to a state of normalcy.”46 The successful post-shutdown orthodontic office will differentiate itself from other practices through creativity, flexibility, and communication.48,49
Cash-flow management goals:
- Proactively increase new patient numbers.
- Bring current patients back on schedule.
- Maximize collection of accounts receivable.
Hindrances to achieving these goals:
- Reduced volume due to elevated safety and distancing measures.
- Reduced volume due to patients’ safety concerns.
- Reduced volume due to patients’ financial burdens during this time.
Financial strategy suggestions:
- Review the AAO’s financial management resources related to COVID-19 for detailed information on unemployment benefits, small business loans, the Paycheck Protection Program, Economic Injury Disaster Loans, and more.50
- Draft a cash-flow plan; a template can be found in Cain Watters & Associates’ “90 Day Cash Flow Plan for Reopening Your Orthodontic Practice.”46
- Set up an online payment system.48
- Establish an office policy to collect at the time of the treatment and stop billing later.51
- Make full efforts to collect patient and other accounts receivable51:
- Missing charges (failure to post charges results in unnoticed delinquent receivables).
- Unfiled or delinquent insurance claims.
- Delinquent patient payments, including declined charges or failed transactions from credit card auto-payments; if necessary, consider reducing monthly payment amounts and/or extending payment periods rather than asking for lump sums to catch up.
- Provide flexible payment options for new patients, such as extended paid-in-full discounts.51
- Make use of the downtime to strengthen the cash-flow monitoring system by cleaning up and organizing the ledgers51:
- Identify missing charges or contracts that need to be posted.
- Reconcile auto-payments with the ledgers.
- Redefine adjustment types.
- Write off any small balances.
- Train and work with staff to produce more accurate practice financial reports.
Marketing strategy suggestions48,49:
- Draft a marketing plan.
- Review the “AAO Guide: Start Strong When Re-Opening.”52
- Tell people your office is open to see patients by sending out text messages and e-mails and posting on the practice website, social media, and review sites.
- Inform your main referrers that you are open for business.
- Design an upbeat “Welcome Back” atmosphere in the reception area.
- Plan for strong summer promotions and reward systems.
- Increase marketing efforts related to safe practices and patient safety measures.
- Make use of the downtime to strengthen your online presence:
- Social media.
- Search engine optimization.
- Refreshing and updating the website.
- Paid advertising (such as pay-per-click).
- Implement two-way texting.
- Offer virtual consultations, which can facilitate starts and make up for reduced patient volume.
- If using paper charts, convert the practice to digital to reduce risks of cross-contamination.
Discussion
Documentation will continue to be vital to the success of a practice at this time. Not only will offices need to carry out special procedures relevant to the COVID-19 pandemic, but they must also meticulously document their actions for safety, continuity of care, and legal protection.
Clinicians should keep in mind that the information provided here is general guidance and by no means replaces expert advice from lawyers, accountants, practice consultants, or marketing specialists. It should be noted that certain recommendations may not be valid in the future, as regulations and guidelines are subject to change based on changes in the pandemic trend, market environment, and decisions of federal and local authorities. This content should be understood within the context of each office’s unique practice environment and philosophy.
*Dr. Park is Professor and Chair and Drs. Kim, Kai, Rogowski, and Liu are residents, Postgraduate Orthodontic Program, Arizona School of Dentistry & Oral Health, A.T. Still University, 5835 E. Still Circle, Mesa, AZ 85206. Dr. Park is also a Contributing Editor of the Journal of Clinical Orthodontics and an International Scholar, Graduate School of Dentistry, Kyung Hee University, Seoul, Korea; e-mail: jpark@atsu.edu.
ACKNOWLEDGMENT: The authors would like to thank Ms. Jenifer Vetter for preparing the manuscript.
REFERENCES
1. Xu, H.; Zhong, L.; Deng, J.; Peng, J.; Dan, H.; Zeng, X.; Li, T.; and Chen, Q.: High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa, Int. J. Oral. Sci. 12:8, 2020.
2. Izzetti, R.; Nisi, M.; Gabriele, M.; and Graziani, F.: COVID-19 transmission in dental practice: Brief review of preventative measures in Italy, J. Dent. Res., doi.org/10.1177%2F0022034520920580, April 17, 2020, accessed May 10, 2020.
3. Kalra, S.; Tripathi, T.; and Rai, P.: Infection control in orthodontics, J. Orthod. Endod., orthodontics-endodontics.imedpub.com/infection-control-in-orthodontics.php?aid=6958, July 29, 2015, accessed May 14, 2020.
4. Dong, Y.; Mo, X.; Hu, Y.; Qi, X.; Jiang, F.; Jiang, Z.; and Tong, S.: Epidemiology of COVID-19 among children in China, Pediat. 145:e20200702, 2020.
5. American Association of Orthodontists: COVID-19 daily employee screening log, assets-prod-www1.aaoinfo.org/assets-prod-www1/2020/05/Ortho-Staff-Temperature-log-with-clear-form-button.pdf, accessed May 10, 2020.
6. Society of American Gastrointestinal and Endoscopic Surgeons: N95 mask re-use strategies, www.sages.org/n-95-re-use-instructions, accessed May 10, 2020.
7. Centers for Disease Control and Prevention: Facial hairstyles and filtering facepiece respirators, www.cdc.gov/niosh/npptl/pdfs/FacialHairW-mask11282017-508.pdf, accessed May 11, 2020.
8. American Association of Orthodontists: Covid-19 resources for orthodontists, www1.aaoinfo.org/covid-19, accessed May 14, 2020.
9. Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; and Ren, B.: Transmission routes of 2019-nCoV and controls in dental practice, Int. J. Oral Sci. 12:9, 2020.
10. Centers for Disease Control and Prevention: Coronavirus disease 2019 (COVID-19) social distancing, www.cdc.gov/coronavirus/2019-ncov/-prevent-getting-sick/social-distancing.html, accessed May 5, 2020.
11. Environmental Protection Agency: List N tool: COVID-19 disinfectants, cfpub.epa.gov/giwiz/disinfectants/index.cfm, accessed May 10, 2020.
12. Centers for Disease Control and Prevention: Infection control guidance for healthcare professionals about coronavirus (COVID-19), www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control.html, April 24, 2020, accessed May 10, 2020.
13. Eggers, M.; Koburger-Janssen, T.; Eickmann, M.; and Zorn, J.: In vitro bactericidal and virucidal efficacy of povidone-iodine gargle/mouthwash against respiratory and oral tract pathogens, Infect. Dis. Ther. 7:249-259, 2018.
14. American Dental Association Center for Professional Success: COVID-19 frequently asked questions, success.ada.org/en/practice-management/patients/coronavirus-frequently-asked-questions, April 16, 2020, accessed May 13, 2020.
15. American Dental Association Center for Professional Success: COVID-19 transmission and emergency care Q&A, success.ada.org/en/practice-management/patients/digital-events/covid-19-transmission-and-emergency-care-q-and-a, accessed May 13, 2020.
16. Harrel, S.K. and Molinari, J.: Aerosols and splatter in dentistry: A brief review of the literature and infection control implications, J. Am. Dent. Assoc. 135:429-437, 2004.
17. Jacks, M.E.: A laboratory comparison of evacuation devices on aerosol reduction, J. Dent. Hyg. 76:202-206, 2002.
18. Toroglu, M.S.; Haytac, M.C.; and Koksal, F.: Evaluation of aerosol contamination during debonding procedures, Angle Orthod. 71:299-306, 2011.
19. Bonetti, G.A.; Zanarini, M.; Parenti, S.I.; Lattuca, M.; Marchionni, S.; and Gatto, M.R.: Evaluation of enamel surfaces after bracket debonding: An in-vivo study with scanning electron microscopy, Am. J. Orthod. 140:696-702, 2011.
20. American Association of Orthodontists: Supplemental health questionnaire orthodontic treatment in the era of COVID-19, assets-prod-www1.aaoinfo.org/assets-prod-www1/2020/05/Supplemental-Health-Questionnaire-COVID19-rev2-fill-sec.pdf, accessed May 13, 2020.
21. American Association of Orthodontists: Informed consent for the orthodontic patient risk and limitations of orthodontic treatment, assets-prod-www1.aaoinfo.org/assets-prod-www1/2020/04/Informed-Consent-English-2020-fillable-secure.pdf, accessed May 10, 2020.
22. Melo, A.C.; Carneiro, L.O.; Pontes, L.F.; Cecim, R.L.; Mattos, J.N.; and Normando, D.: Factors related to orthodontic treatment time in adult patients, Dent. Press J. Orthod. 18:59-63, 2013.
23. American Dental Association: Return to work interim guidance toolkit, success.ada.org/~/media/CPS/Files/Open%20Files/ADA_Return_to_Work_Toolkit.pdf, May 7, 2020, accessed May 12, 2020.
24. Alharbi, A.; Alharbi, S.; and Alqaidi, S.: Guidelines for dental care provision during the COVID-19 pandemic, Saudi Dent. J. 32:181-186, 2020.
25. Centers for Disease Control and Prevention: Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings, www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html, accessed May 8, 2020.
26. Occupational Safety and Health Administration: Guidance on preparing workplaces for COVID-19, osha.gov/Publications/OSHA3990.pdf, March 2020, accessed May 10, 2020.
27. Jampani, N.D.; Nutalapati, R.; Dontula, B.S.; and Boyapati, R.: Applications of teledentistry: A literature review and update, J. Int. Soc. Prevent. Comm. Dent. 1:37-44, 2011.
28. Qamar, M.A.: COVID-19: A look into the modern age pandemic, J. Pub. Health, link.springer.com/content/pdf/10.1007/s10389-020-01294-z.pdf (preprint), posted May 11, 2020.
29. Maharaj, S. and Kleczkowski, A.: Controlling epidemic spread by social distancing: Do it well or not at all, BMC Pub. Health 12:679, 2012. 30. Ahmed, F.; Zviedrite, N.; and Uzicanin, A.: Effectiveness of workplace social distancing measures in reducing influenza transmission: A systematic review, BMC Pub. Health 18:518, 2018.
31. American Association of Orthodontists: Interim orthodontic PPE summary based on current CDC and OSHA guidelines, assets-prod-www1.aaoinfo.org/assets-prod-www1/2020/05/PPE-FLOWCHART.pdf, accessed May 10, 2020.
32. Levin, R.: The orthodontic recovery strategic timeline (webinar), Orthod. Pract. Insights, www.ghorthodontics.com/html/orthodontic-practice-insights.htm#, accessed May, 6, 2020.
33. Priya, H.; Acharya, S.; Bhat, M.; and Ballal, M.: Microbial contamination of the white coats of dental staff in the clinical setting, J. Dent. Res. Dent. Clin. Dent. Prospects 3:136-140, 2009.
34. Rautemaa, R.; Nordberg, A.; Wuolijoki-Saaristo, K.; and Meurman, J. H.: Bacterial aerosols in dental practice: A potential hospital infection problem? J. Hosp. Infect. 64:76-81, 2006.
35. Day, C.J.; Price, R.; Sandy, J.R.; and Ireland, A.J.: Inhalation of aerosols produced during the removal of fixed orthodontic appliances: A comparison of 4 enamel cleanup methods, Am. J. Orthod. 133:11-17, 2008.
36. Centers for Disease Control and Prevention: Decontamination and reuse of filtering facepiece respirators, www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/decontamination-reuse-respirators.html, April 30, 2020, accessed May 10, 2020.
37. Perencevich, E.N.; Diekema, D.J.; and Edmond, M.B.: Moving personal protective equipment into the community, face shields and containment of COVID-19, JAMA, jamanetwork.com/journals/jama/fullarticle/-2765525, April 29, 2020, accessed May 10, 2020.
38. Rebmann, T.; Carrico, R.; and Wang, J.: Physiologic and other effects and compliance with long-term respirator use among medical intensive care unit nurses, Am. J. Infect. Control 41:1218-1223, 2013.
39. Oshagh, M.; Hematiyan, M.R.; Mohandes, Y.; Oshagh, M.R.; and Pishbin, L.: Autoclaving and clinical recycling: Effects on mechanical properties of orthodontic wires, Ind. J. Dent. Res. 23:638-642, 2012.
40. Equal Employment Opportunity Commission: What you should know about COVID-19 and the ADA, the Rehabilitation Act, and other EEO laws, www.eeoc.gov/wysk/what-you-should-know-about-covid-19-and-ada-rehabilitation-act-and-other-eeo-laws, May 7, 2020, accessed May 13, 2020.
41. Hegarty, G.: Will new overtime rules affect you, success.ada.org/en/practice-management/dental-practice-success/fall-2016/will-new-overtime-rules-affect-you, accessed May 10, 2020.
42. U.S. Department of Labor: Families First Coronavirus Response Act: Employee paid leave rights, www.dol.gov/agencies/whd/pandemic/ffcra-employee-paid-leave, accessed May 10, 2020.
43. CEDR HR Solutions: How to reopen your business after coronavirus, www.cedrsolutions.com/healthcare/employer-reopen-guide, accessed May 13, 2020.
44. Chavez, N.: Another wave of coronavirus will likely hit the US in the fall. Here’s why and what we can do to stop it, Cable News Network, www.cnn.com/2020/05/02/health/coronavirus-second-wave-fall-season/index.html, May 2, 2020, accessed May 14, 2020.
45. Yan, H. and Andrew, S.: You asked, we’re answering: Your top coronavirus questions, Cable News Network, www.cnn.com/interactive/2020/health/coronavirus-questions-answers/?fbclid=IwAR0mg7y0b0KoJRFpF4Q3LLhpayGHtxPVTmEl5VqtvWabAjPH9EiPpVEnEro, accessed May 14, 2020.
46. Cain Watters & Associates: 90 Day cash flow plan for reopening your orthodontic practice, pcsortho-104d1.kxcdn.com/wp-content/uploads/2020/04/cwa-90-action-plan-Worksheet-4.21.20_final.pdf, accessed May 15, 2020.
47. Bentson, C.: Trends for the next decade, practice modality options, valuation norms, AAO annual virtual conference, aaoinfo.digitellinc.com/aaoinfo/sessions/2703/view, May 3, 2020, accessed May 15, 2020.
48. Leach, B.: Effective marketing in the new normal, AAO annual virtual conference, aaoinfo.digitellinc.com/aaoinfo/sessions/2533/view, May 3, 2020, accessed May 16, 2020.
49. Werner, A.: Preparing the orthodontic practice for coronavirus, Orthod. Prod., www.orthodonticproductsonline.com/treatment-products/accessories/infection-control/preparing-orthodontic-practice-coronavirus-covid-19, March 4, 2020, accessed May 14, 2020.
50. American Association of Orthodontists: Financial resources related to the COVID-19, www1.aaoinfo.org/covid-19/financial-resources-related-to-the-covid-19, accessed May 14, 2020.
51. Shoemaker, J.: Examining your financial fitness & cash flow strategies, AAO annual virtual conference, May 3, 2020, aaoinfo.digitellinc.com/aaoinfo/sessions/2503/view, accessed May 14, 2020.
52. American Association of Orthodontists: Start strong when re-opening, www1.aaoinfo.org/start-strong-resources-for-successful-re-opening, accessed May 13, 2020.

