CASE REPORT
Extraction Treatment of a Gummy Smile with Lingual Orthodontics and Skeletal Anchorage
Excessive gingival display, or a “gummy smile,” is a nonpathological, multifactorial condition in which more than 3-4mm of gingival tissue is exposed in smiling.1,2 Because gummy smiles are perceived as esthetically unappealing, they are a common motivation for patients to seek orthodontic treatment.
The associated anterior vertical excess often requires surgical correction by anterior segmental surgery, Le Fort I impaction, or segmental Le Fort I surgery with differential impaction.3,4 If a patient is unwilling to undergo surgical treatment, an orthodontic camouflage treatment can be attempted, although it may create detrimental effects on facial appearance. For example, a camouflage approach involving upper premolar extractions can increase the nasolabial angle and extrude the maxillary incisors.5-7
A recently developed solution is to use temporary anchorage devices (TADs) for direct intrusion of the anterior teeth.8 Power arms can be added for the anterior teeth to further reduce side effects such as uncontrolled tipping and facilitate bodily movement during en masse retraction.9
This case report details the successful management of a gummy smile using four premolar extractions and a combination of skeletal anchorage and lingual orthodontics assisted by power arms.
Diagnosis and Treatment Plan
An 18-year-old male requested treatment with an esthetic appliance (Fig. 1). His profile was convex, with a balanced nose, normal nasolabial angle and mentolabial sulcus, and retrusive lower jaw. From the front, the face was well proportioned and symmetrical, with centered midlines, though a slight lip incompetence was noted.
Similar articles from the archive:
- CASE REPORT Treatment of an Accentuated Gummy Smile with Skeletally Anchored Orthodontic Intrusion October 2023
- An Interdisciplinary Approach to Treating Impacted Canines Associated with Gummy Smiles November 2020
- Correction of Severe Overbite and Gummy Smile in Patients with Bimaxillary Protrusion April 2010

Fig. 1 18-year-old male patient with gummy smile before treatment (continued in next image).
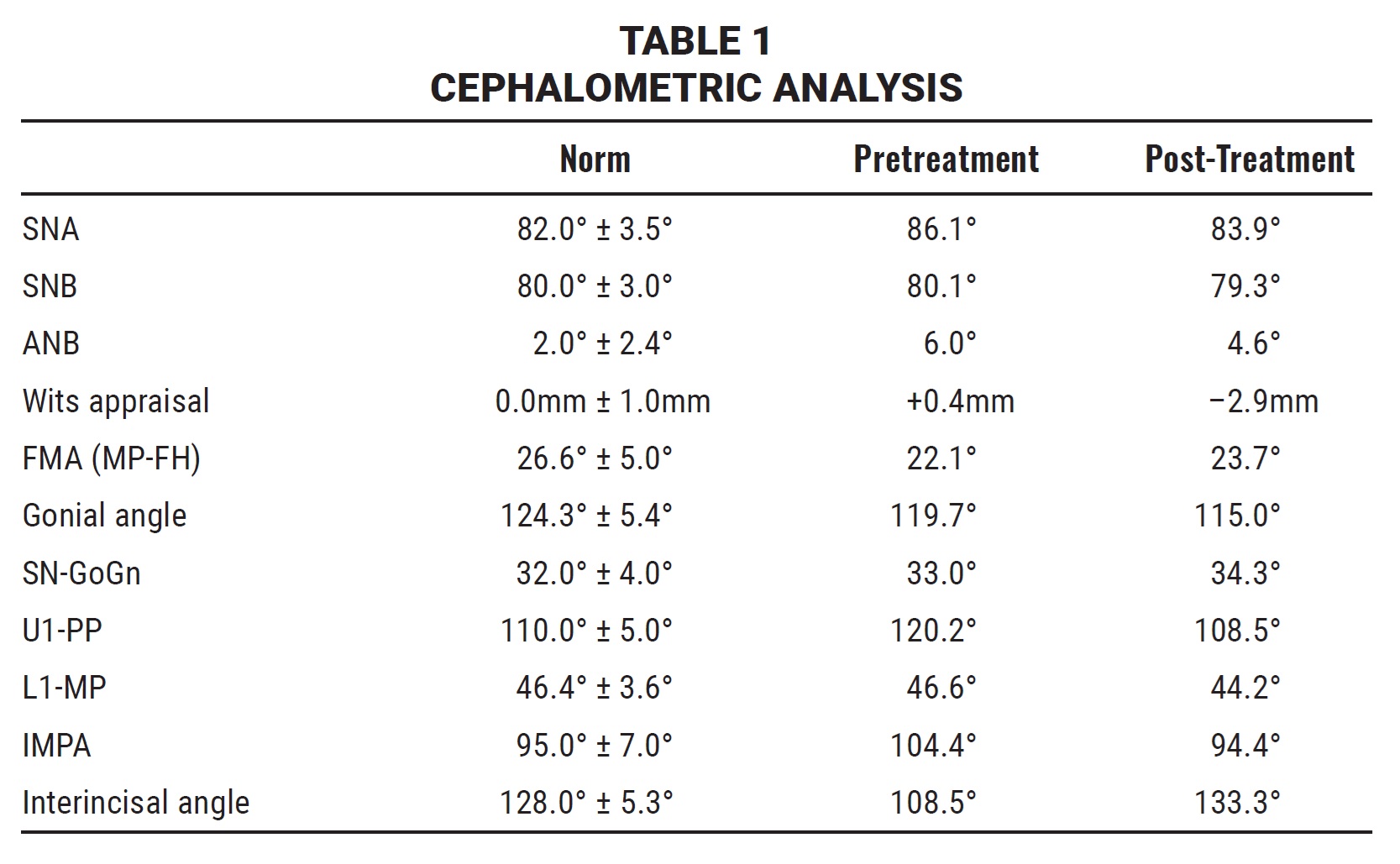
In smiling, the patient exhibited excessive gingival display, along with short clinical crowns, an interincisal diastema, and generalized spacing. Bilateral Class I canine and molar relationships were present, with mild crowding in the lower arch and exaggerated upper and lower curves of Spee. All teeth were present, including the third molars (Fig. 1B and 1C).
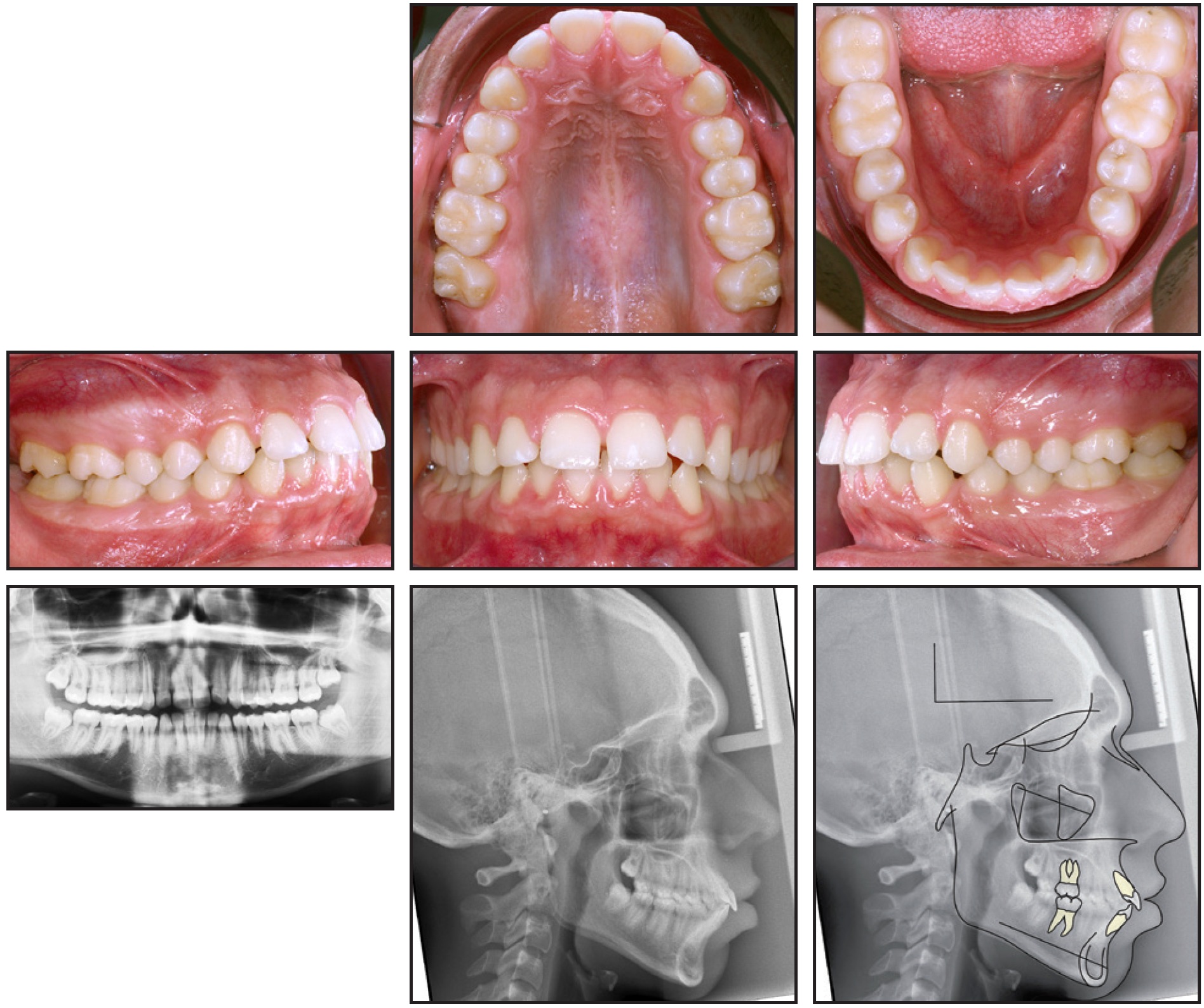
Fig. 1 (cont.) 18-year-old male patient with gummy smile before treatment (continued in next image).
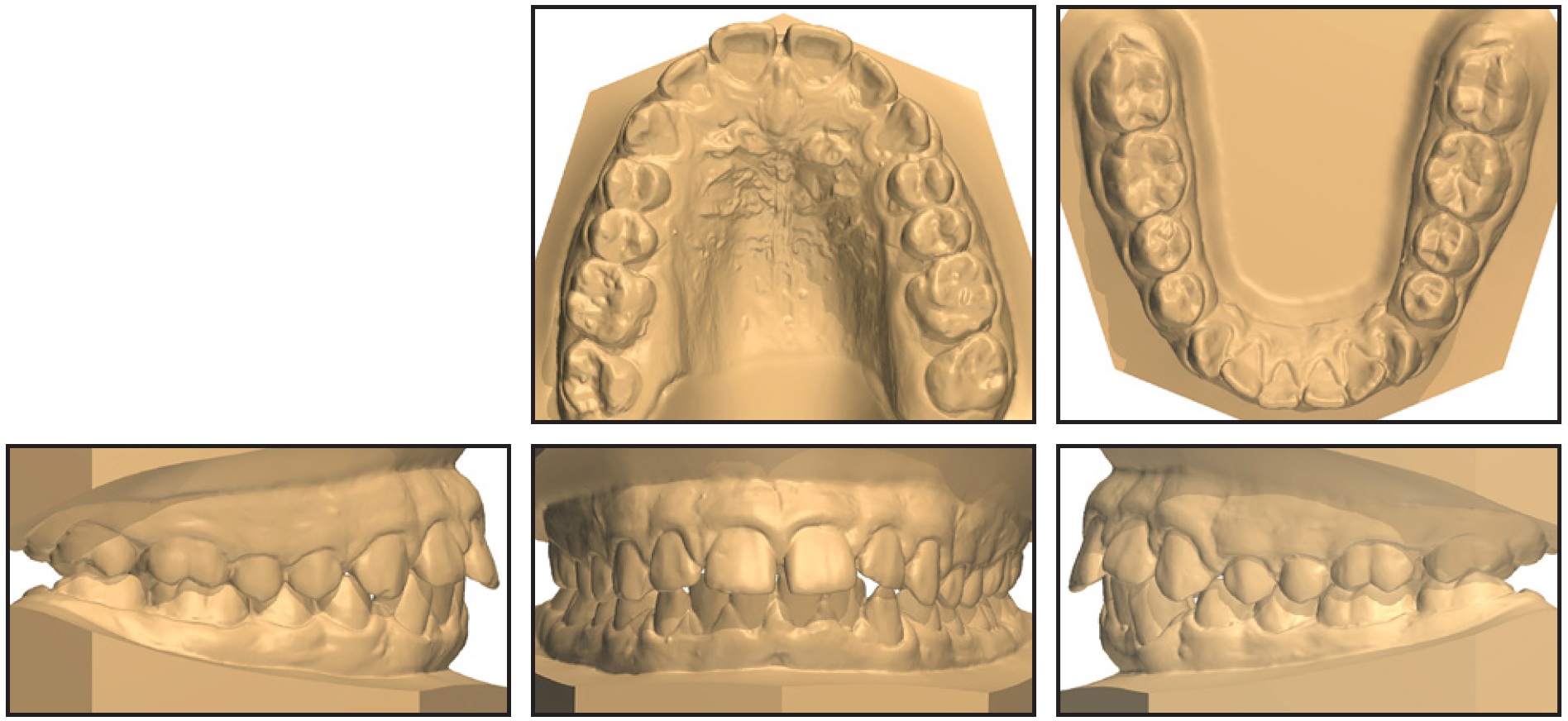
Fig. 1 (cont.) 18-year-old male patient with gummy smile before treatment.
Cephalometric analysis (Table 1) indicated a skeletal Class II malocclusion (ANB = 6°) with a tendency toward hypodivergence (FMA = 22.1°), as well as excessively proclined upper and lower incisors (U1-PP = 120.2°, IMPA = 104.4°).
The patient was diagnosed with altered passive eruption (APE), a genetically linked developmental disorder characterized by apical migration of the soft tissue, which partially covers the clinical crowns of the teeth, resulting in excessive gingival display.10,11 According to the system of Coslet and colleagues,11 the patient was APE type 1, as distinguished by a gingival margin incisal or occlusal to the cementoenamel junction and a mucogingival junction apical to the alveolar crest, with an excessively wide band of keratinized gingiva and short clinical crowns. Based on radiographic examination and bone sounding, the patient’s condition could be further classified as subgroup B, in which the alveolar crest is located close to the cementoenamel junction.10,12
The treatment objectives were to improve the facial profile and eliminate the gummy smile. A combination of orthognathic surgery and premolar extractions was proposed, but this option was rejected by the patient. Instead, the patient agreed to a camouflage approach involving premolar extractions; significant anterior retraction with a lingual appliance, using skeletal anchorage and power arms to prevent adverse effects on the incisors; and periodontal surgery to improve the contours of the gingiva (Fig. 2). Normalizing the inclinations and lengths of the incisors would improve facial esthetics, leaving open the possibility of future surgical maxillary impaction.

Fig. 2 Simulation of ideal gingival contours.
Due to the sagittal discrepancy, the upper first and lower second premolars were chosen for removal; the extraction approach was further supported by the presence of the third molars. Because space closure in a patient with proclined incisors risks worsening a gummy smile, the incisors would also be intruded to create an ideal smile arc.
Treatment Progress
To reduce proclination of the upper incisors during space closure, the standard torque overcorrections were omitted from the setup for preadjusted Ormco ALIAS* brackets (Fig. 3).
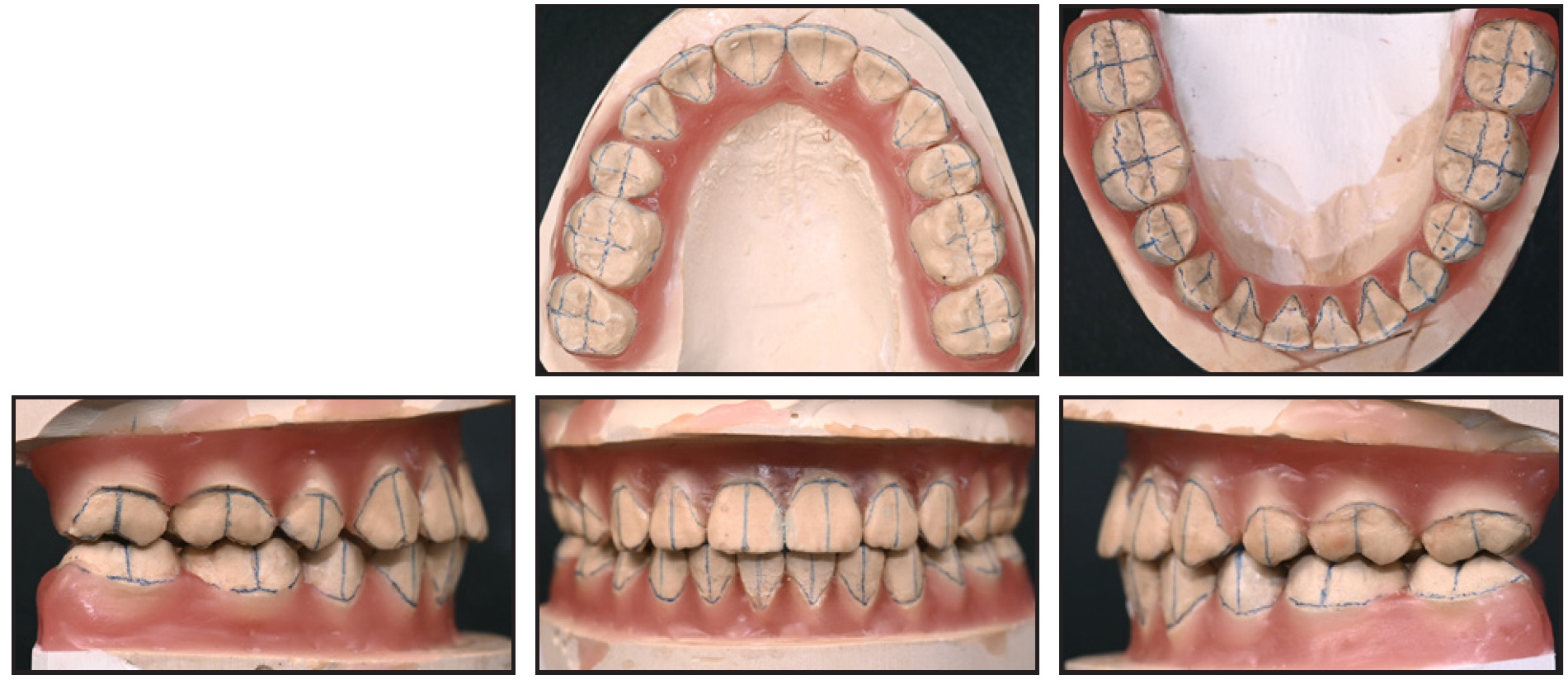
Fig. 3 Setup of lingual appliance.
Indirect bonding was performed using single jigs, following the Komori KommonBase technique,13 and .013" copper nickel titanium archwires (medium in the upper arch and small in the lower) were inserted for initial alignment, excluding the upper first and lower second premolars (Fig. 4). Closed springs were placed in those segments to reinforce the wires over the wide interbracket spans. Interproximal reduction was performed on the premolars to prevent unwanted movement of the anterior teeth, enabling the extractions to be delayed so that space closure could begin with full-thickness stainless steel archwires. Occlusal build-ups were added to the upper molars to promote molar intrusion.
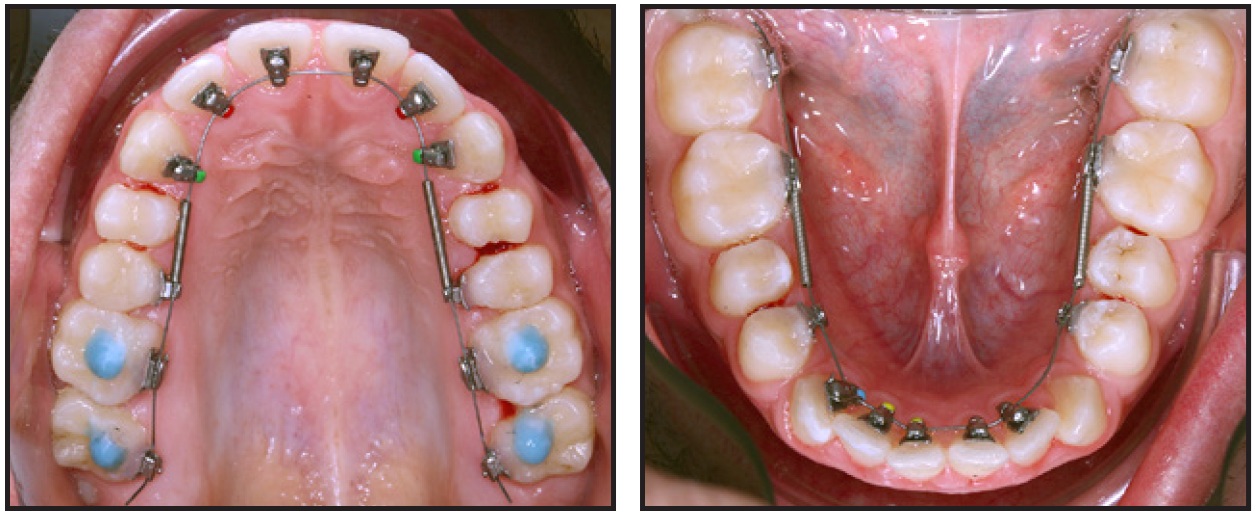
Fig. 4 Lingual appliance placed with .013" copper nickel titanium archwires.
Four months later, .018" × .018" copper nickel titanium archwires (medium upper and small lower) were placed for continued leveling and torque management. Buccal molar tubes were added to control the posterior teeth and, later, to assist in alignment of the third molars.
Six months after the beginning of treatment, when the full-thickness copper nickel titanium archwires were fully expressed, the digital planning for TAD insertion was performed using Blue Sky Plan** software. Cone-beam computed tomographic imaging was obtained, and the DICOM files were matched with the STL models to identify positions with adequate bone to support the skeletal appliance (Fig. 5).
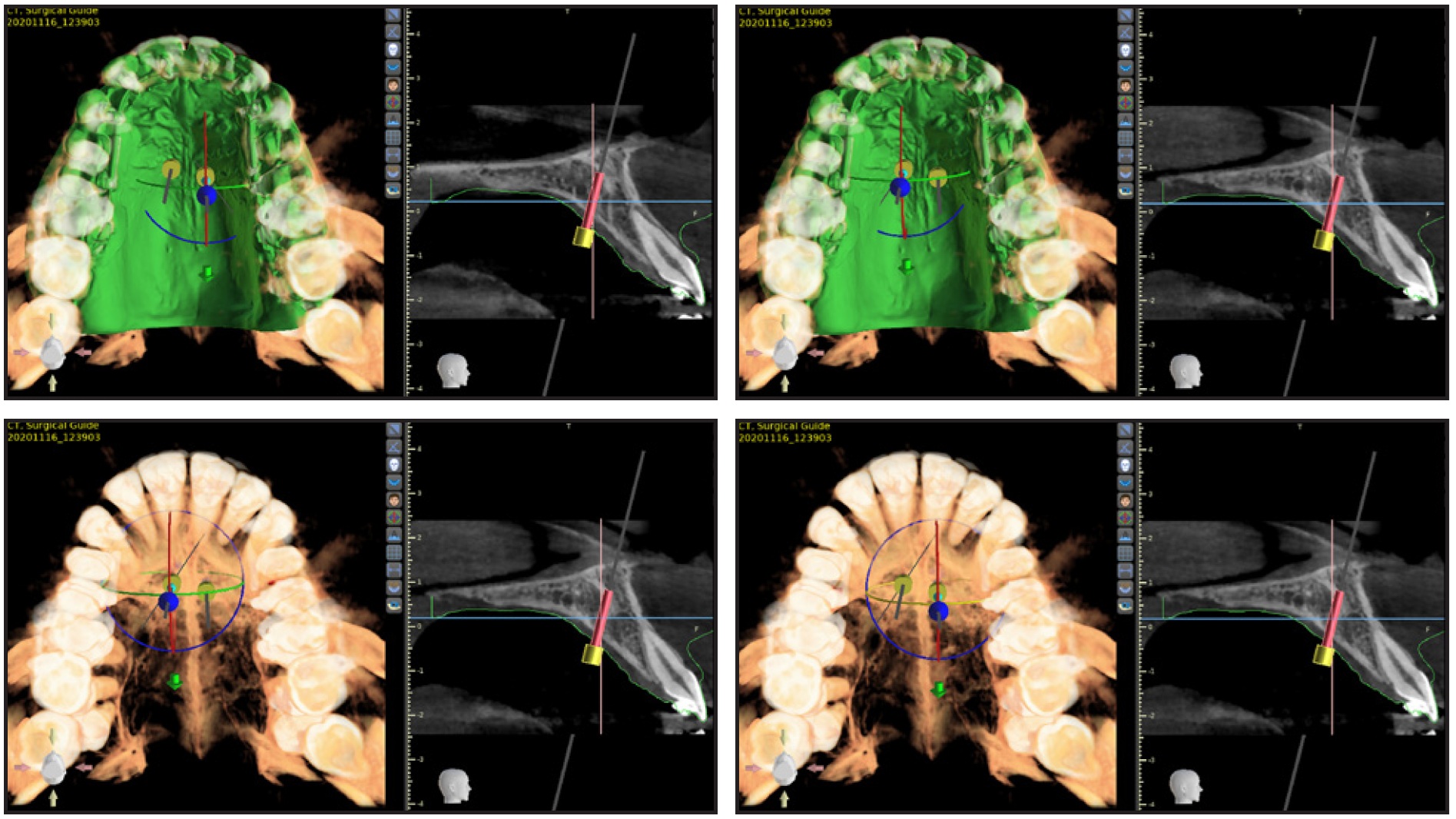
Fig. 5 Digital planning of miniscrew insertion.
The upper first and lower second premolars were extracted (Fig. 6). Two 2mm × 15mm Spider Screws*** were placed in the palate, and a skeletal appliance was installed for simultaneous intrusion and retraction of the upper anterior teeth. Small lower and medium upper .018" × .018" stainless steel archwires were inserted, along with power arms for the anterior teeth to prevent uncontrolled tipping, control incisor torque, and facilitate bodily movement, following the method of Komaki and colleagues.14

Fig. 6 Upper first and lower second premolars extracted, palatal Spider Screws*** placed to support skeletal appliance, and .018" × .018" stainless steel archwires inserted.
Five months later, space closure with a closed elastomeric chain was initiated in the lower arch (Fig. 7). Vertical retraction of the upper anterior teeth continued to level the incisal edges.

Fig. 7 Space closure with closed elastomeric chain.
The finishing stage began two years after the start of treatment. The archwires were changed to medium upper and small lower .0175" × .0175" TMA,* with finishing and detailing bends added to refine the alignment and occlusion. After a total treatment time of two years and ten months, upper and lower Essix† retainers were delivered for nighttime wear (Fig. 8).15

Fig. 8 Patient after 34 months of treatment.
One month after debonding, gingivectomy and osseous resective surgery were performed.10,11 Chu’s Aesthetic Gauges‡ were used to determine the ideal gingival heights of the anterior teeth, based on mean distributions of tooth sizes, widths, and esthetic proportion ratios (Fig. 9).12 In this case, the gauges showed abnormal width-to-length ratios of the upper left canine and first premolar, which were addressed with the gingivectomy.12
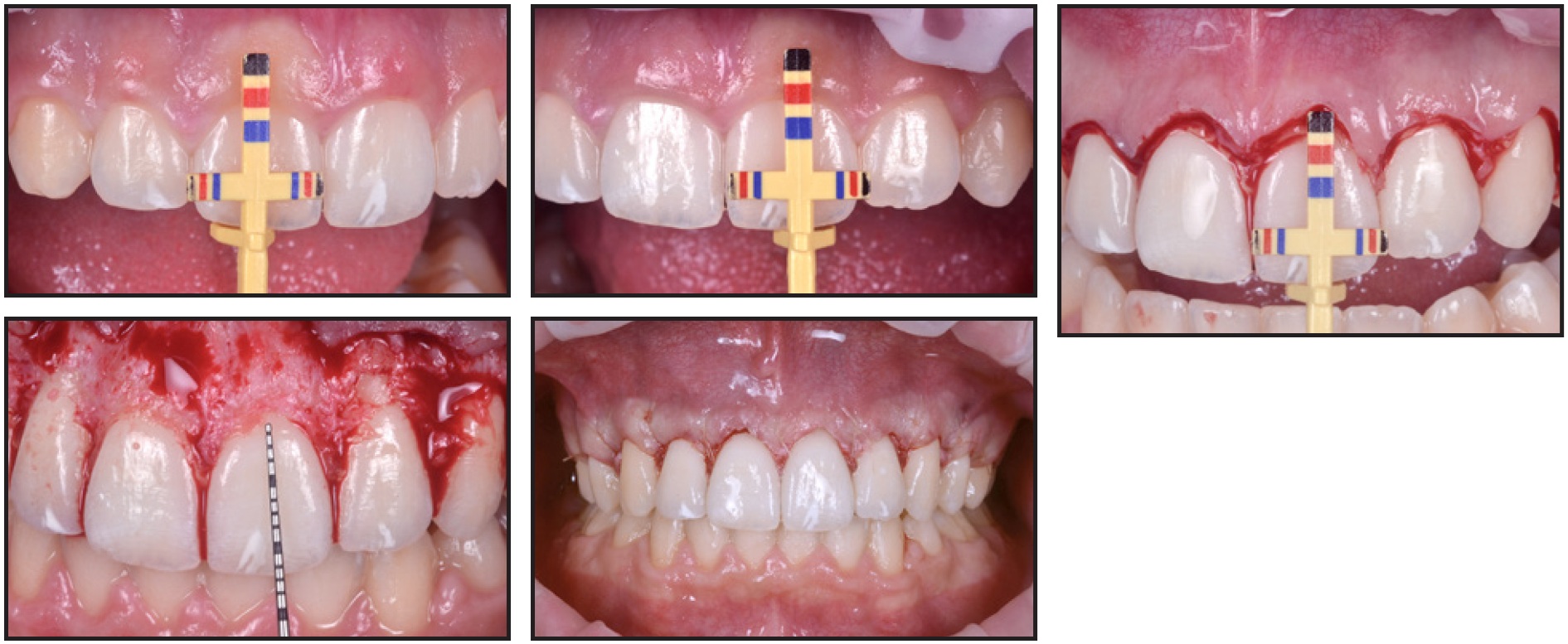
Fig. 9 Periodontal surgery performed, with Chu’s Aesthetic Gauges‡ used to determine ideal gingival height.
Four months later, when healing was complete, upper 2-2 and lower 3-3 retainers were bonded (Fig. 10A). Some improvement in posterior occlusal contact was observed at this point (Fig. 10B).
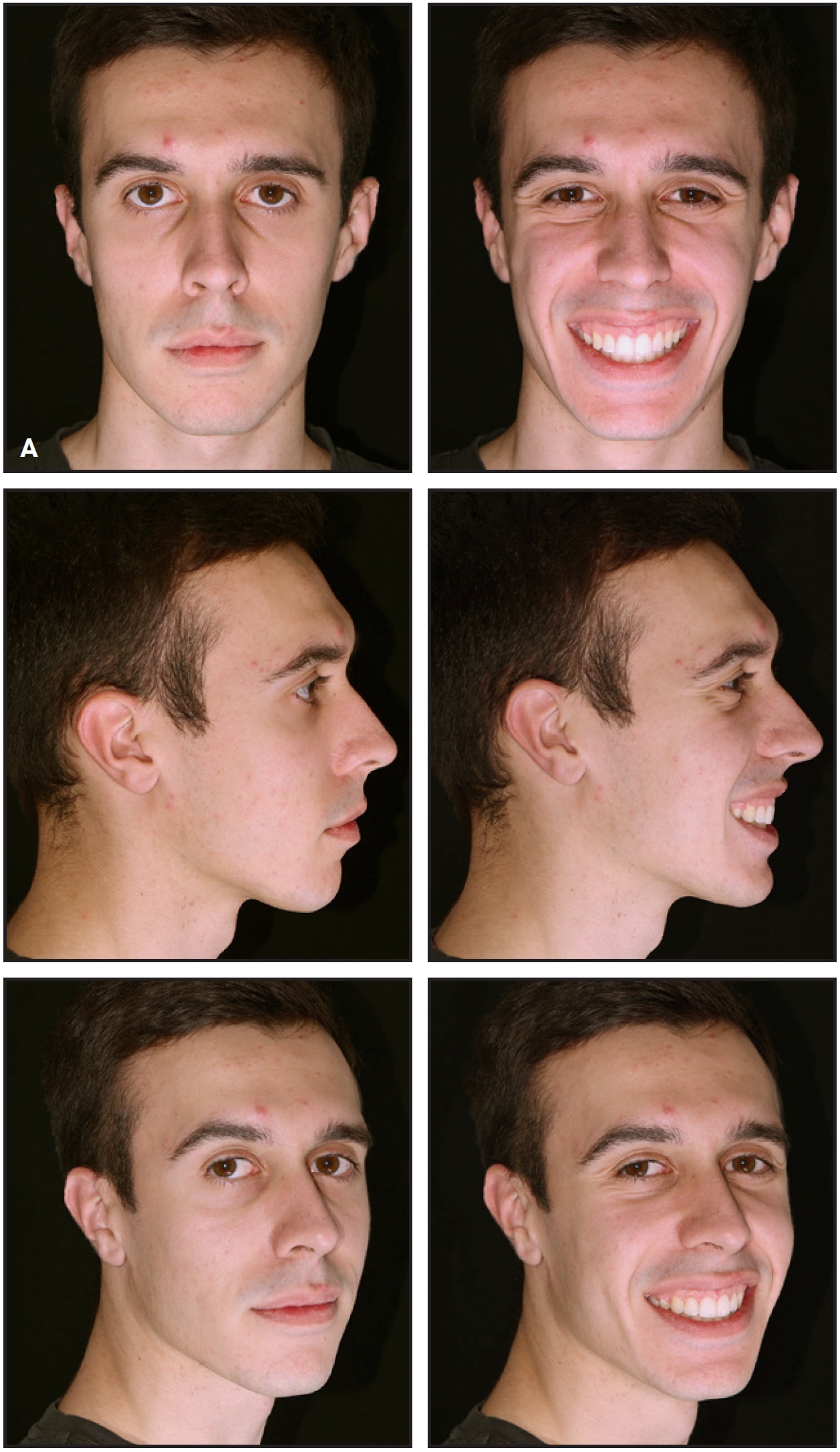
Fig. 10 A. After four months of postsurgical healing, upper 2-2 and lower 3-3 retainers bonded (continued in next page).
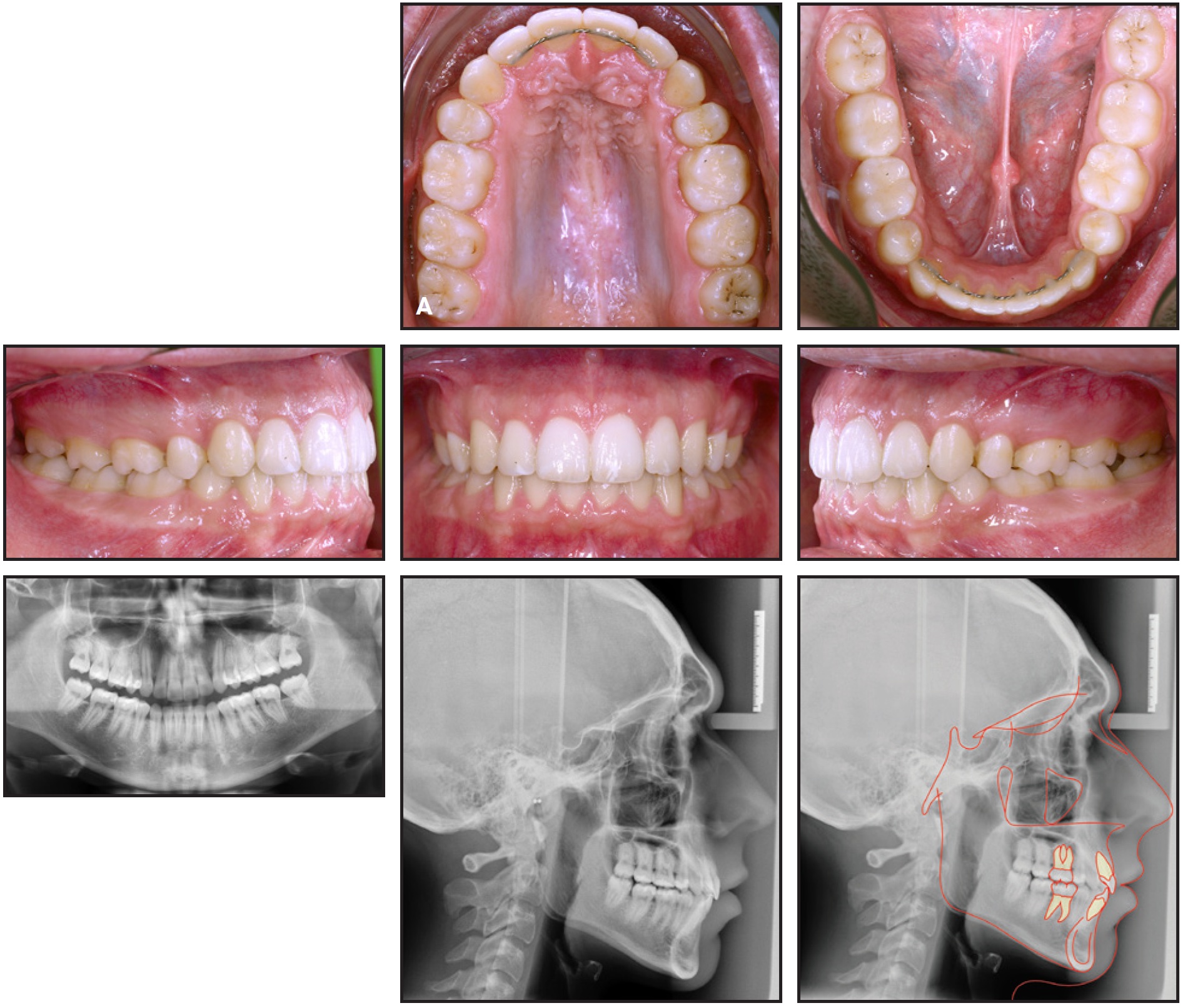
Fig. 10 (cont.) A. After four months of postsurgical healing, upper 2-2 and lower 3-3 retainers bonded (continued in next image).
Treatment Results
All treatment goals were accomplished, with close adherence to the digital plan, confirming the accuracy of the preadjusted lingual system.16 The profile was improved, and a good lip seal was established. Correction of the incisor inclinations and the excessive gingival display had produced an appealing smile. Solid Class I canine and molar relationships were obtained on both sides, while the curves of Spee were leveled. The anterior teeth were in ideal light contact, and the marginal ridges were aligned. The panoramic radiograph confirmed root parallelism, and cephalometric analysis17-19 demonstrated an improvement in the inclinations of the upper and lower incisors (U1-PP = 108.5°, IMPA = 94.4°) and favorable changes in the soft-tissue profile (Table 1 and Fig. 10C).
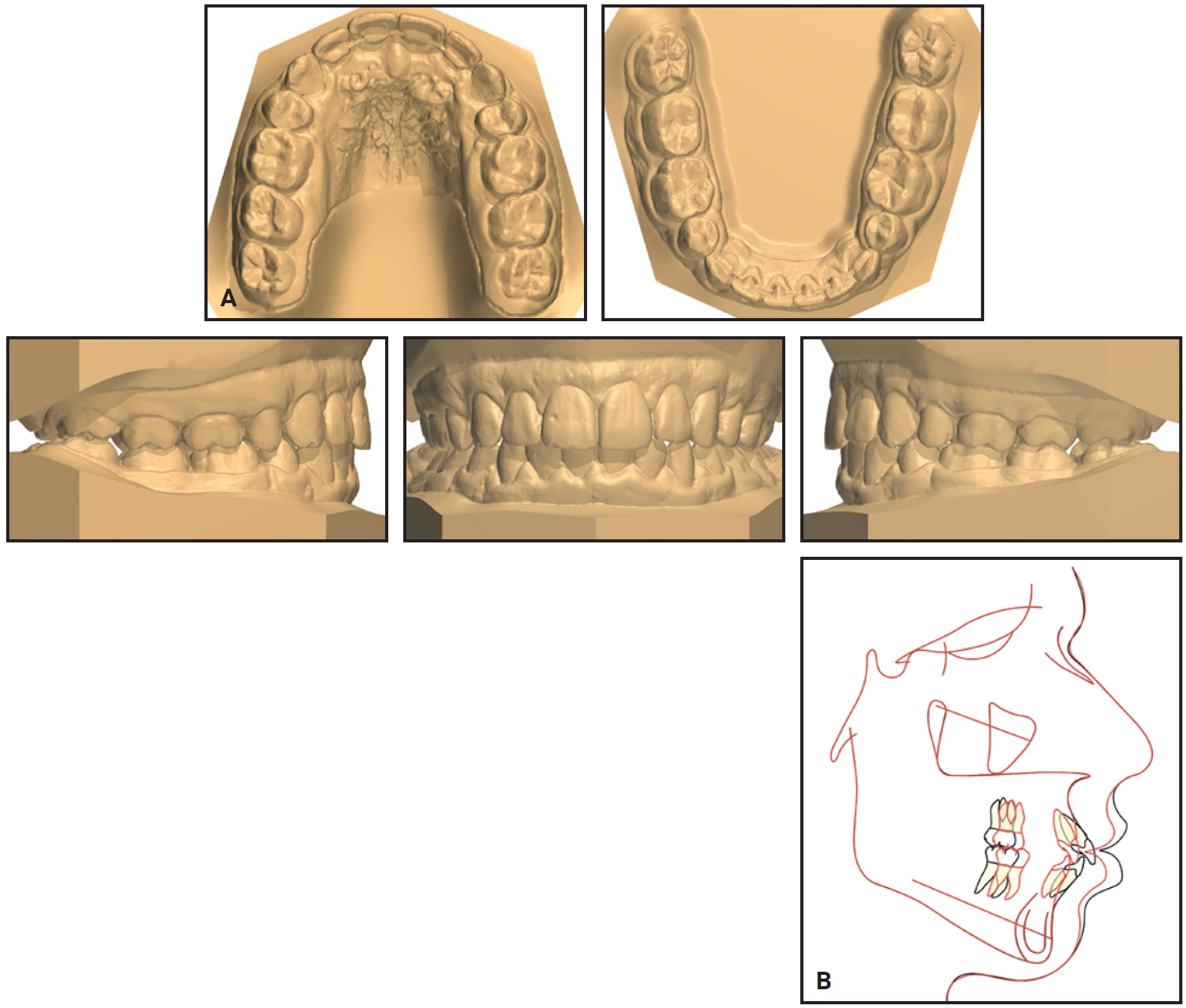
Fig. 10 (cont.) A. After four months of postsurgical healing, upper 2-2 and lower 3-3 retainers bonded. B. Superimposition of pretreatment (black) and post-treatment (red) cephalometric tracings.
Discussion
Potential causes of excessive gingival display include extruded incisors, vertical maxillary excess, short maxillary anterior crowns, a hyperactive upper lip, and APE.20 Because of the tendency of conventional intrusion mechanics to induce labial tipping of the incisors, especially in extraction cases, gummy smiles are often addressed surgically.3,4,21-24 Surgical correction carries its own risks, however, including alveolar bone necrosis, infection, and loss of tooth vitality.25 In selected cases, the direct application of intrusive forces from miniscrews offers a viable alternative.25-27
Although miniscrews for incisor intrusion are typically placed between the roots of the anterior teeth,5,7 other positions have been used with success. Kaku and colleagues treated a gummy smile with anterior retraction facilitated by miniscrews in the buccal alveolar bone between the second premolars and first molars in both arches, followed by anterior intrusion with two additional miniscrews in the maxillary bone between the upper canines and lateral incisors.25 In the present case, palatal anchorage was used to achieve simultaneous anterior intrusion and extraction-space closure while preventing undesirable side effects.
The skeletally anchored palatal appliance and power arms successfully intruded and retracted the upper incisors with good vertical control, resolving the patient’s gummy smile. As these results demonstrate, a camouflage treatment involving extraction of the upper first and lower second premolars may be an effective approach that preserves the option of future orthognathic surgery in borderline cases.
FOOTNOTES
- *Registered trademark of Ormco, Brea, CA; www.ormco.com.
- **Blue Sky Bio, Grayslake, IL; www.blueskybio.com.
- ***Registered trademark of HDC, Thiene, Italy; www.hdc-italy.com.
- †Registered trademark of Dentsply Sirona, Charlotte, NC; www.dentsplysirona.com.
- ‡HuFriedy Group, Chicago, IL; www.hufriedygroup.com.
REFERENCES
- 1. Dym, H. and Pierre, R. 2nd: Diagnosis and treatment approaches to a “gummy smile,” Dent. Clin. N. Am. 64:341-349, 2020.
- 2. Pavone, A.F.; Ghassemian, M.; and Verardi, S.: Gummy smile and short tooth syndrome—Part 1: Etiopathogenesis, classification, and diagnostic guidelines, Compend. Cont. Ed. Dent. 37:102-107, 2016.
- 3. Bastidas, J.A.: Surgical correction of the “gummy smile,” Oral Maxillofac. Surg. Clin. N. Am. 33:197-209, 2021.
- 4. Capelozza Filho, L.; Cardoso Mde, A.; Reis, S.A.; and Mazzottini, R.: Surgical-orthodontic correction of long-face syndrome, J. Clin. Orthod. 40:323-308, 2006.
- 5. Kinzinger, G.; Frye, L.; and Diedrich, P.: Class II treatment in adults: Comparing camouflage orthodontics, dentofacial orthopedics and orthognathic surgery—A cephalometric study to evaluate various therapeutic effects, J. Orofac. Orthop. 70:63-91, 2009.
- 6. Janson, G.; Mendes, L.M.; Junqueira, C.H.; and Garib, D.G.: Soft-tissue changes in Class II malocclusion patients treated with extractions: A systematic review, Eur. J. Orthod. 38:631-637, 2016.
- 7. Zhou, Y.W.; Wang, Y.Y.; He, Z.F.; Lu, M.X.; Li, G.F.; and Li, H.: Orthodontic-surgical treatment for severe skeletal class II malocclusion with vertical maxillary excess and four premolars extraction: A case report, World J. Clin. Cases 11:1106-1114, 2023.
- 8. Kim, T.W.; Kim, H.; and Lee, S.J.: Correction of deep overbite and gummy smile by using a mini-implant with a segmented wire in a growing Class II Division 2 patient, Am. J. Orthod. 130:676-685, 2006.
- 9. Hedayati, Z. and Shomali, M.: Maxillary anterior en masse retraction using different antero-posterior position of mini screw: A 3D finite element study, Prog. Orthod. 17:31, 2016.
- 10. Mele, M.; Felice, P.; Sharma, P.; Mazzotti, C.; Bellone, P.; and Zucchelli, G.: Esthetic treatment of altered passive eruption, Periodontol. 2000 77:65-83, 2018.
- 11. Coslet, J.G.; Vanarsdall, R.; and Weisgold, A.: Diagnosis and classification of delayed passive eruption of the dentogingival junction in the adult, Alpha Omegan 70:24-28, 1977.
- 12. Chu, S.J. and Hochman, M.N.: A biometric approach to aesthetic crown lengthening: Part I—midfacial considerations, Pract. Proced. Aesth. Dent. 20:17-24, 2008.
- 13. Komori, A.; Takemoto, K.; Shimoda, T.; Miyashita, W.; and Scuzzo, G.: Precise direct lingual bonding with the KommonBase, J. Clin. Orthod. 47:42-49, 2013.
- 14. Komaki, H.; Hamanaka, R.; Tominaga, J.Y.; Jinnai, S.; Nguyen, T.A.; Kuga, D.; Koga, Y.; and Yoshida, N.: Biomechanical features of tooth movement from a lingual appliance in comparison with a labial appliance during space closure in sliding mechanics, Am. J. Orthod. 162:307-317, 2022.
- 15. Albertini, P.; Albertini, E.; Siciliani, G.; and Lombardo, L.: Fluorescence-aided composite removal during lingual bracket debonding, J. Esth. Restor. Dent. 32:634-637, 2020.
- 16. Albertini, P.; Albertini, E.; Pellitteri, F.; Ghislanzoni, L.H.; and Lombardo, L.: Accuracy of planned tooth movement with lingual straight wire technique, Angle Orthod. 92:714-721, 2022.
- 17. Björk, A. and Skieller, V.: Growth of the maxilla in three dimensions as revealed radiographically by the implant method, Br. J. Orthod. 4:53-64, 1977.
- 18. Björk, A.: Prediction of mandibular growth rotation, Am. J. Orthod. 55:585-599, 1969.
- 19. Kim, M.G.; Moon, J.H.; Hwang, H.W.; Cho, S.J.; Donatelli, R.E.; and Lee, S.J.: Evaluation of an automated superimposition method based on multiple landmarks for growing patients, Angle Orthod. 92:226-232, 2022.
- 20. Silberberg, N.; Goldstein, M.; and Smidt, A.: Excessive gingival display—etiology, diagnosis, and treatment modalities, Quintess. Int. 40:809-818, 2009.
- 21. Ataoglu, H.; Uçkan, S.; Karaman, A.I.; and Uyar, Y.: Bimaxillary orthognathic surgery in a patient with long face: A case report, Int. J. Adult Orthod. Orthog. Surg. 14:304-309, 1999.
- 22. Barton, K.A.: Overbite changes in the Begg and edgewise techniques, Am. J. Orthod. 62:48-55, 1972.
- 23. Otto, R.L.; Anholm, J.M.; and Engel, G.A.: A comparative analysis of intrusion of incisor teeth achieved in adults and children according to facial type, Am. J. Orthod. 77:437-446, 1980.
- 24. Engel, G.; Cornforth, G.; Damerell, J.M.; Gordon, J.; Levy, P.; and McAlpine, J.: Treatment of deep-bite cases, Am. J. Orthod. 77:1-13, 1980.
- 25. Kaku, M.; Kojima, S.; Sumi, H.; Koseki, H.; Abedini, S.; Motokawa, M.; Fujita, T.; Ohtani, J.; Kawata, T.; and Tanne, K.: Gummy smile and facial profile correction using miniscrew anchorage, Angle Orthod. 82:170-177, 2012.
- 26. Polat-Ozsoy, O.; Arman-Ozcirpici, A.; and Veziroglu, F.: Miniscrews for upper incisor intrusion, Eur. J. Orthod. 31:412-416, 2009.
- 27. Wang, X.D.; Zhang, J.N.; Liu, D.W.; Lei, F.F.; Liu, W.T.; Song, Y.; and Zhou, Y.H.: Nonsurgical correction using miniscrew-assisted vertical control of a severe high angle with mandibular retrusion and gummy smile in an adult, Am. J. Orthod. 151:978-988, 2017.








COMMENTS
.