Treatment with the Mandibular Arnold Expander
Nonsurgical Treatment of a Surgically Prepared Skeletal Class III Patient Using Skeletal Anchorage
A skeletal Class III is one of the most complex malocclusions to treat.1,2 According to Ellis and McNamara, it is most commonly characterized by a retrusive maxilla, protrusive maxillary incisors, retrusive mandibular incisors, a protrusive mandible, and excessive lower facial height.3 Adult skeletal Class III patients can be treated by either orthodontic camouflage or orthognathic surgery, depending on the degree of skeletal discrepancy, the skeletal pattern, and the age of the patient.4 Orthodontic camouflage treatment generally involves retroclination of the mandibular incisors and proclination of the maxillary incisors to achieve a positive overjet and correct the canine relationship. Options include extraoral traction or the use of Class III elastics (alone or in combination with sliding jigs), with space provided by interproximal stripping or extractions.5 Recently, the introduction of skeletal anchorage has made orthodontic camouflage a more viable option in mild to moderate skeletal Class III cases.
The situation becomes more complicated if orthognathic surgery is planned, but the patient refuses surgery while presurgical orthodontic treatment is already in progress—especially if the patient has a vertical growth pattern. In such a case, as described in this report, skeletal anchorage can allow distalization of the entire mandibular dentition as an alternative to premolar extractions.6
Diagnosis and Treatment Plan
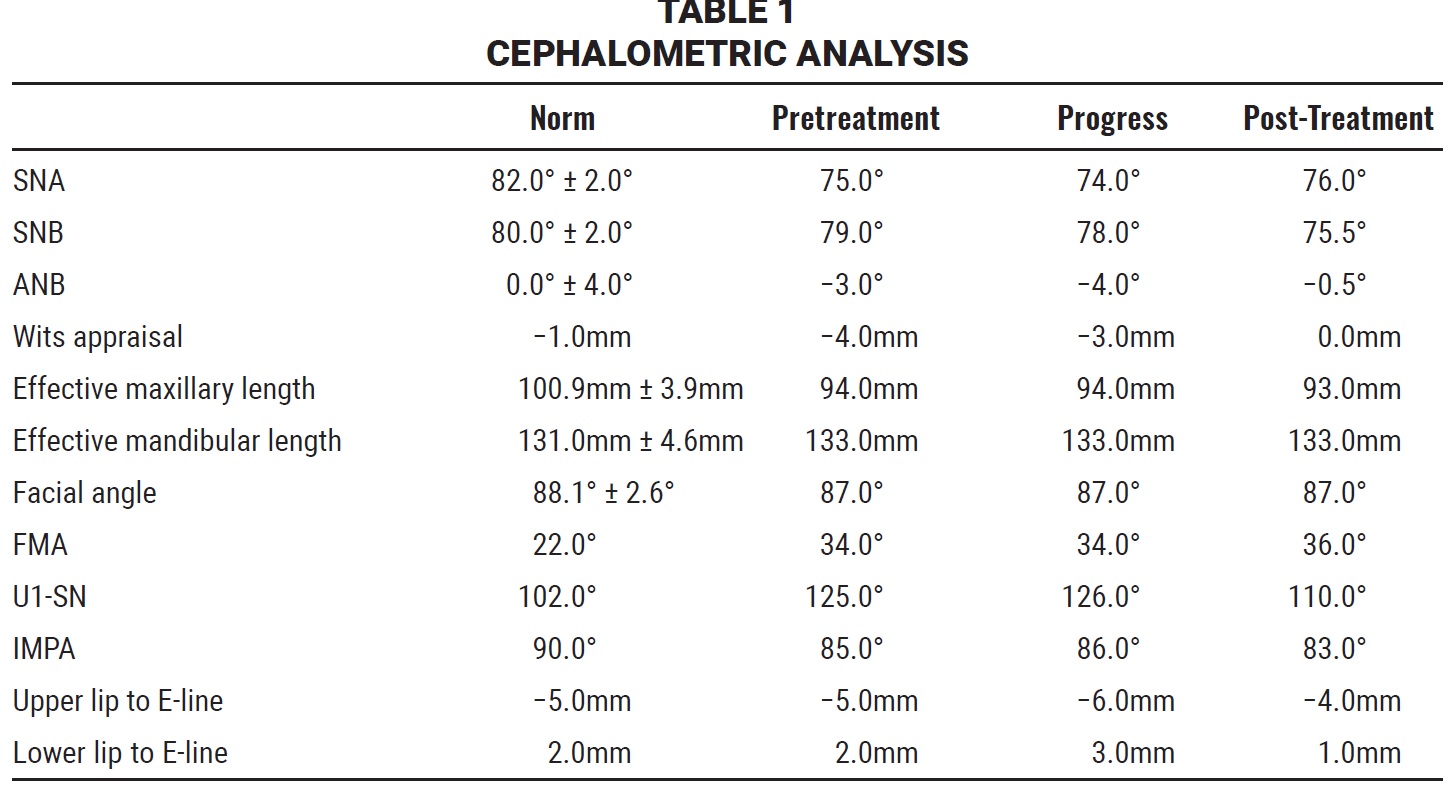
A 21-year-old male presented with the chief complaints of an unesthetic facial appearance, irregular teeth, and speech difficulties. He reported a history of trauma to his upper front teeth. The patient had a dolichocephalic skull, a leptoprosopic face, acceptable facial symmetry, and a concave profile with lip incompetence (Fig. 1). There was a 4mm anterior open bite, and the upper midline was shifted 2mm to the right. The maxillary arch displayed 6mm of crowding, with a palatally positioned upper right lateral incisor and an amalgam restoration on the upper right first molar. The mandibular arch had 4mm of crowding, with amalgam restorations in the posterior regions. The lower right first molar restoration was fractured, and the lower premolars were supraerupted.
Similar articles from the archive:
- CASE REPORT A Zygomatic Miniplate as Skeletal Anchorage for Correction of Severe Skeletal Anterior Open Bite April 2020
- CASE REPORT Two-Stage Treatment of Skeletal Class III Malocclusion with Arch-Width Discrepancy and Lower Incisor Agenesis May 2019
- CASE REPORT Skeletal Open-Bite Correction with Mini-Implant Anchorage and Minimally Invasive Surgery September 2018
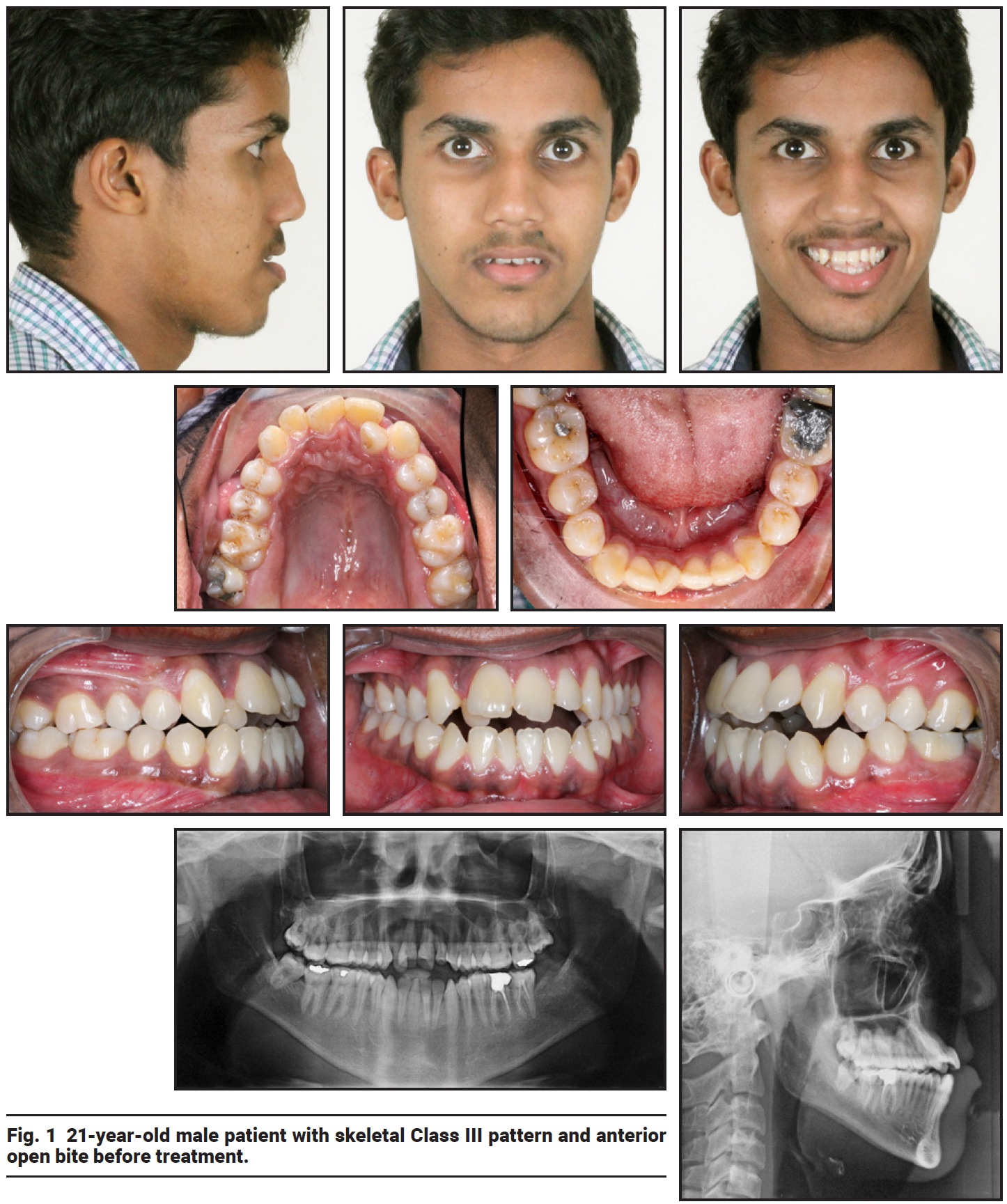
Fig. 1 21-year-old male patient with skeletal Class III pattern and anterior open bite before treatment.
Radiographic evaluation revealed root-canal treatment of the lower right first molar, which was asymptomatic. All third molars had erupted except for a missing lower left third molar. Lateral cephalometric analysis (Table 1) indicated a skeletal Class III pattern (ANB = −3°, Wits appraisal = −4mm) with a hyperdivergent growth pattern (SNMP = 35°). The maxillary base was backwardly postioned (SNA = 75°). The maxillary incisors were proclined (U1-SN = 125°), and the mandibular incisors were retroclined (IMPA = 85°). Cephalometrics for orthognathic surgery (COGS) analysis (Ptm-N = 59mm) and quadrilateral cephalometric analysis confirmed that the maxilla was backwardly placed and deficient in length.
Treatment objectives were to correct the skeletal base, anterior open bite, crowding, and midline deviation; establish a Class I canine relationship; achieve a normal overjet and overbite and a stable occlusal relationship; and obtain an acceptable profile with a pleasant smile.
The first treatment option was to extract the upper first premolars and use the space to relieve crowding and decompensate the proclined upper incisors, thus producing a negative overjet prior to surgical advancement of the maxilla. The second option involved camouflage orthodontic treatment following the extraction of all four first premolars. Because the patient wanted a pleasant profile, well-aligned dentition, and improved speech, he agreed to the surgical treatment plan.
Treatment Progress
Professional oral prophylaxis was prescribed, and an opinion regarding the status of the lower left first molar and upper left anterior teeth was requested from the Department of Conservative and Endodontic Dentistry. Tongue exercises were also prescribed.
After extraction of the upper first premolars, preadjusted .022" × .028" MBT* brackets were bonded in both arches. Leveling and alignment were carried out over six months using an archwire sequence of .014" nickel titanium, .016" × .022" nickel titanium, and .019" × .025" nickel titanium. A U-loop made of .016" × .022" beta titanium wire was inserted for anterior retraction, but not activated. Canine retraction was continued on the left side using elastomeric chain from the second molar.
At this stage, after six months of leveling and alignment, the patient refused surgery. This required a change in orthodontic treatment from a presurgical to a camouflage approach, using skeletal anchorage. The new objectives would be to obtain a positive overjet and close the upper extraction spaces, thus establishing a Class I canine relationship. Achievement of an ideal profile was questionable.
To facilitate en-masse distalization of the mandibular dentition, the lower right third molar was extracted. At the same time, under local anesthesia, miniplates were affixed to the anterior border of the mandibular rami using surgical screws (Fig. 2). An orthodontic force of 400g per side was generated using elastomeric chain from the miniplate to a crimpable hook between the lower lateral incisor and canine (Fig. 3).
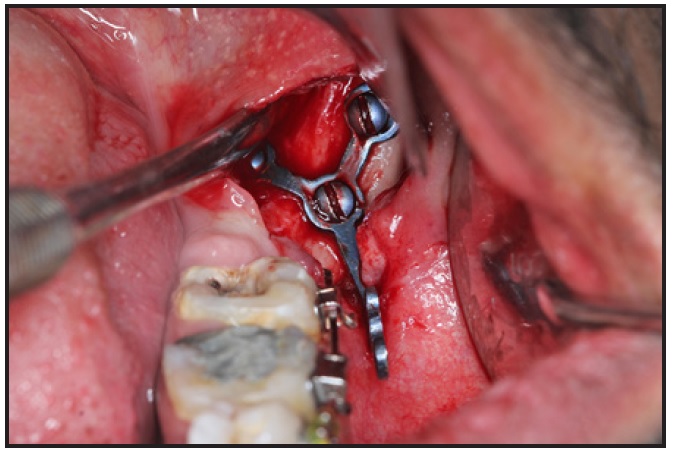
Fig. 2 Fixation of miniplate to anterior border of mandibular ramus after six months of leveling and alignment.
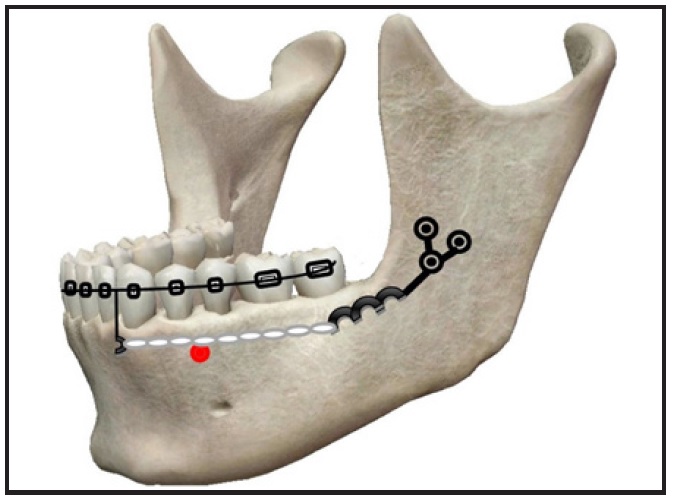
Fig. 3 Orthodontic force applied from miniplate to crimpable hook between lower lateral incisor and canines for en-masse distalization.
After six months of en-masse distalization, when 3mm of positive overjet had been created, retraction of the maxillary dentition was initiated using loop mechanics (Fig. 4). An open U-loop made of .016" × .022" beta titanium wire was applied on the left side for anterior space closure, while power chains were added to expedite canine retraction. The right extraction space had already been closed by distal canine movement during the leveling and alignment phase, since the lateral incisor was palatally positioned.
When the patient moved overseas, four months after placement of the elastomeric chain, we could not complete the treatment as planned. Two years later, the patient reported to the clinic requesting that the appliances be debonded; they were removed without occlusal settling or the establishment of proper interdigitation.
The patient was advised to continue his tongue exercises. A fixed lower 3-3 retainer was bonded.
Treatment Results
Nearly all of the initial treatment objectives were achieved (Fig. 5A). The upper and lower crowding and anterior open bite were resolved in the presurgical orthodontic phase. After the subsequent compromise treatment, the smile esthetics improved considerably, and the lip incompetence and negative lip step were corrected. The patient was satisfied with his profile. The dental midlines were coincident with the facial midline; acceptable overbite and overjet were achieved, along with Class I canine and Class II molar relationships. The patient did not report any TMJ pain or discomfort during or after orthodontic treatment. A panoramic radiograph showed no signs of significant root or bone resorption, with acceptable root parallelism.

Fig. 4 After six months of distalization in lower arch, U-loop mechanics applied for upper anterior retraction.
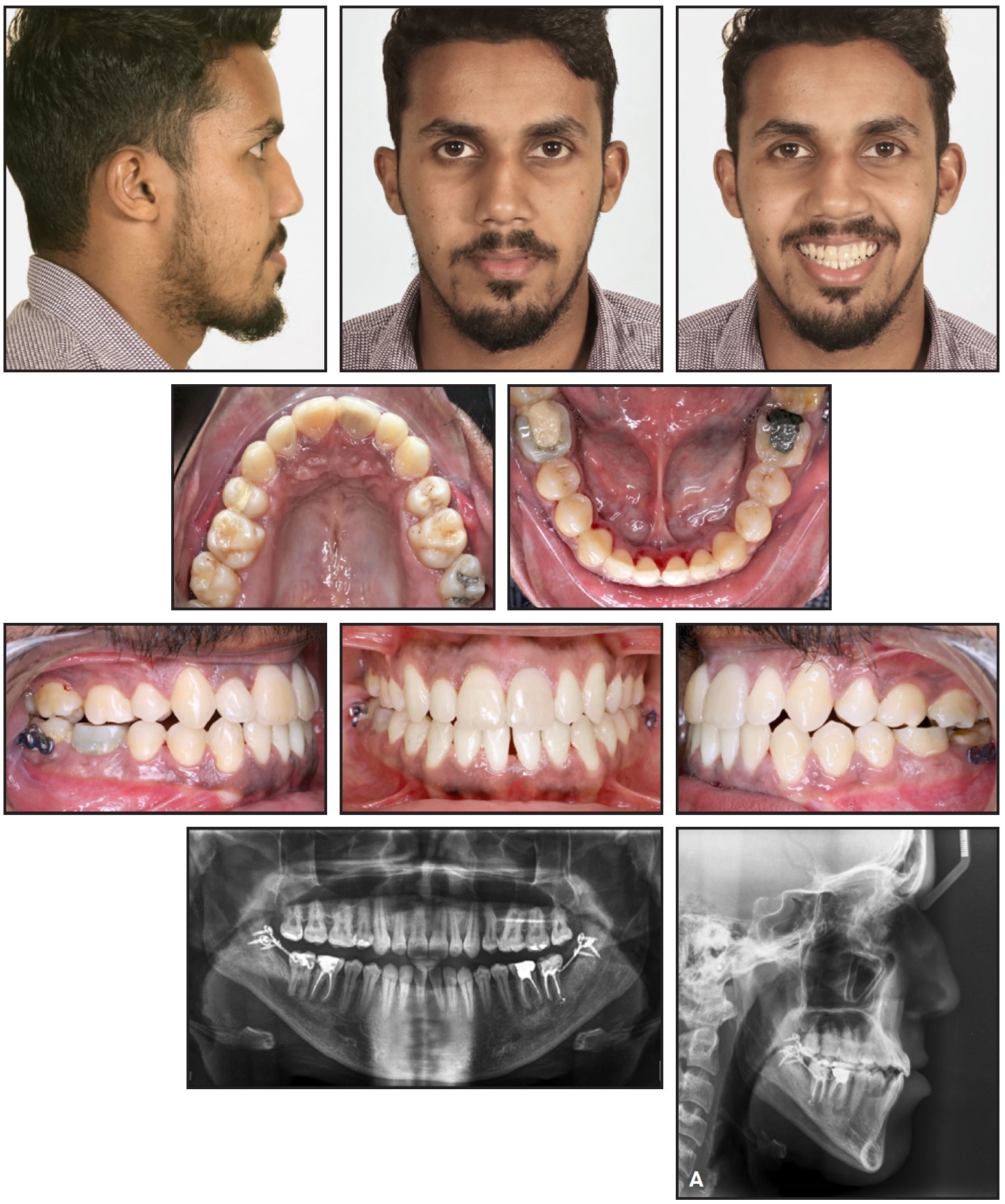
Fig. 5 A. Patient after 34 months of treatment (continued in next image).
Cephalometric evaluation indicated a reduction in upper incisor proclination, a slight backward movement of the mandible (SNB = 75.5°), a reduction in the ANB angle (ANB = −.5°), and an improved Wits appraisal (Table 1). There was no change in chin prominence (facial angle = 87°), but the superimposition showed a slight downward and backward movement of pogonion, possibly due to the distalization of the molars and clockwise rotation of the mandible. A slight opening of the mandibular plane angle (FMA = 36°) was noted because of the downward and backward rotation of the mandible. Superimposition of the pretreatment and progress tracings showed extrusion of the upper and lower anterior segments, mild extrusion of the upper molars, and an edge-to-edge anterior bite. Superimposition of the progress and post-treatment tracings also indicated slight extrusion of the upper and lower molars and posterior displacement of the lower molars, resulting in a Class III molar relationship. Soft-tissue examination confirmed posterior displacement of point B and labrale inferius and the establishment of a good lip seal (Fig. 5B).
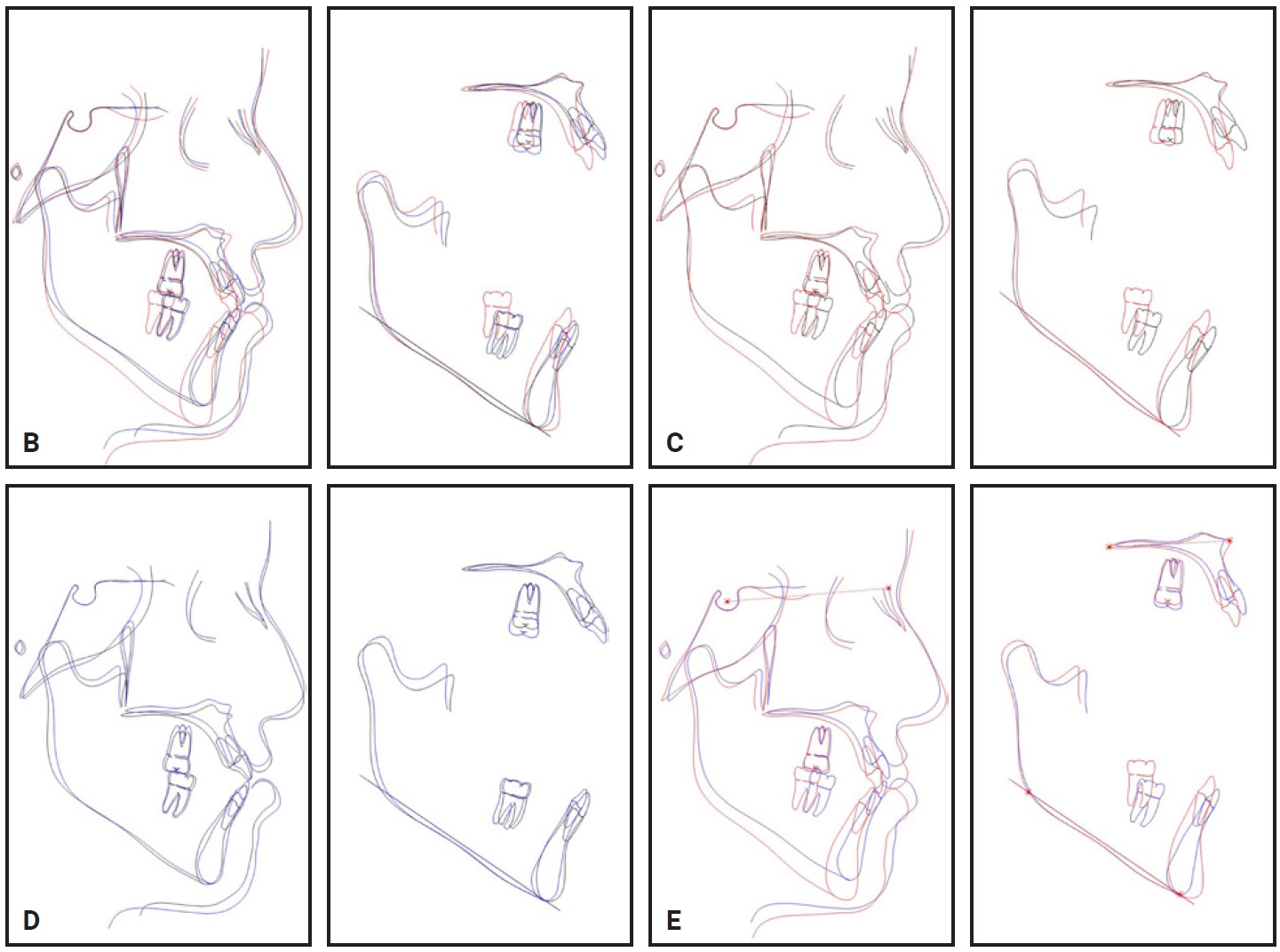
Fig. 5 (cont.) B. Superimposition of cephalometric tracings before treatment (black), after six months of treatment (blue), and after treatment (red). C. Superimposition of cephalometric tracings before treatment (black) and after treatment (red). D. Superimposition of cephalometric tracings before treatment (black) and after six months of treatment. E. Superimposition of cephalometric tracings after six months of treatment (blue) and after treatment (red).
Discussion
When a skeletal Class III discrepancy is beyond the limits of dental compensation, orthognathic surgery is usually the only option to create a stable occlusion and acceptable profile.7 In the case shown here, the patient was being prepared for maxillary advancement surgery. When he refused surgery after completion of the leveling and alignment phase, the treatment plan had to be changed to en-masse distalization of the lower arch, using skeletal anchorage to create a positive overjet. The patient’s vertical growth pattern would make it difficult to obtain an esthetic profile.
In the initial diagnosis, the skeletal Class III base was attributed to a short and backwardly placed maxilla: SNA was 75° and the effective maxillary length was 94mm, which is 4mm deficient for that age, according to McNamara.8 Upper premolar extractions were prescribed to help relieve crowding and resolve the incisor proclination. Minor lower incisor crowding was addressed by proclination of the lower anterior teeth. Positive overjet was achieved by en-masse distalization of the lower arch using miniplate anchorage, and the upper extraction spaces were closed using loop mechanics, thereby reducing proclination of the upper anterior segments.
The Wits appraisal is considered the most discriminative factor in determining whether a developing Class III malocclusion should be treated by camouflage treatment or surgery. The average Wits value for patients to be treated nonsurgically, as defined by Stellzig-Eisenhauer and colleagues, is 4.6mm ± 1.7mm.9 Since our patient’s Wits appraisal fell within this range, we could reasonably plan camouflage treatment using the ramal plate to anchor retraction of the entire mandibular dentition.
Sugawara and colleagues found that while many types of mechanics could be used to distalize the mandibular molars to some extent, the amount of distal translation that could be achieved was quite limited.10 They concluded that the use of skeletal anchorage could provide three-dimensional control of tooth movement, even if the amount of required movement was greater than the mesiodistal width of the premolars. When distalization of more than 3-4mm is performed with anchorage from interradicular miniscrews, however, the force required may cause frequent screw failures.11,12 Miniplates can withstand more force and are more stable because they are anchored to the bone with multiple screws.12-15 A systematic review by Schätzle and colleagues reported a 7.3% failure rate for miniplates, compared with 16.4% for miniscrews.14 Since 7mm of molar distalization was required in our case, we chose to use miniplates instead of miniscrews.
A minor 2° opening of the mandibular plane angle was an expected compromise due to our change in treatment plan, but neither the profile nor the TMJ function of the patient was affected. Retraction mechanics using skeletal anchorage helped to correct the deviated occlusal plane in the lower arch. The upper arch showed slight proclination and the lower showed retroclination, as is common in camouflage treatment of skeletal Class III patients. In the end, we were able to manage this surgically prepared skeletal Class III patient through a nonsurgical approach with skeletal anchorage. Treatment resulted in a pleasing profile, proper occlusion, and normal overjet and overbite, although the occlusion was less than ideal because of unforeseen circumstances.
Stability of treatment is a major concern of every orthodontist. Angle attributed relapse of orthodontic treatment to unfavorable environmental factors. Proffit, in his “equilibrium theory revisited,” maintained that intrinsic forces from the tongue can affect the equilibrium of tooth positions.16 Particularly in an open-bite Class III case, the posture, size, and position of the tongue are critical during retention; a neuromuscular adaptation to an altered tongue position can be expected. Our patient was advised to continue his tongue exercises, and a fixed lower retainer was bonded for long-term stability.
FOOTNOTES
- *Trademark of 3M, Monrovia, CA; www.3M.com.
REFERENCES
- 1. Kama, J.D.; Ozer, T.; and Baran, S.: Orthodontic and orthopedic changes associated with treatment in subjects with Class III malocclusions, Eur. J. Orthod. 28:496-502, 2006.
- 2. Jacobson, A.; Evans, W.G.; Preston, C.B.; and Sadowsky, P.L.: Mandibular prognathism, Am. J. Orthod. 66:140-171, 1974.
- 3. Ellis, E. and McNamara, J.A. Jr.: Components of adult Class III malocclusion, J. Oral Maxillofac. Surg. 42:295-305, 1984.
- 4. Baik, H.S.: Limitations in orthopedic and camouflage treatment for Class III malocclusion, Semin. Orthod. 13:158-174, 2007.
- 5. Niwa, K.; Kushimoto, K.; and Yamamaoto, T.: Mandibular first premolar teeth extraction in skeletal Class III malocclusion, Gifu Shika Gakkai Zasshi 17:330-338, 1990.
- 6. Lin, J. and Gu, Y.: Preliminary investigation of the nonsurgical treatment of severe skeletal Class III malocclusion in the permanent dentition, Angle Orthod. 73:401-410, 2003.
- 7. Mahfouz, M.: The current concepts of orthodontic discrepancy stability, Open J. Stomatol. 4:184-196, 2014.
- 8. McNamara, J.A. Jr.: A method of cephalometric evaluation, Am. J. Orthod. 86:449-469, 1984.
- 9. Stellzig-Eisenhauer, A.; Lux, C.J.; and Schuster, G.: Treatment decision in adult patients with Class III malocclusion: Orthodontic therapy or orthognathic surgery? Am. J. Orthod. 122:27-37, 2002.
- 10. Sugawara, J.; Daimaruya, T.; Umemori, M.; Nagasaka, H.; Takahashi, I.; Kawamura, H.; and Mitani, H.: Distal movement of mandibular molars in adult patients with the Skeletal Anchorage System, Am. J. Orthod. 125:130-138, 2004.
- 11. Park, J. and Cho, H.J.: Three-dimensional evaluation of interradicular spaces and cortical bone thickness for the placement and initial stability of microimplants in adults, Am. J. Orthod. 136:314-e1, 2009.
- 12. Ludwig, B.; Glasl, B.; Kinzinger, G.S.; Lietz, T.; and Lisson, J.A.: Anatomical guidelines for miniscrew insertion: Vestibular interradicular sites, J. Clin. Orthod. 45:165-173, 2011.
- 13. Chen, Y.J.; Chang, H.H.; Huang, C.Y.; Hung, H.C.; Lai, E.H.; and Yao, C.C.: A retrospective analysis of the failure rate of three different orthodontic skeletal anchorage systems, Clin. Oral Impl. Res. 18:768-775, 2007.
- 14. Schätzle, M.; Männchen, R.; Zwahlen, M.; and Lang, N.P.: Survival and failure rates of orthodontic temporary anchorage devices: A systematic review, Clin. Oral Impl. Res. 20:1351-1359, 2009.
- 15. Yao, C.C.; Chang, H.H.; Chang, J.Z.; Lai, H.H.; Lu, S.C.; and Chen, Y.J.: Revisiting the stability of mini-implants used for orthodontic anchorage, J. Formosan Med. Assoc. 114:1122-1128, 2015.
- 16. Proffit, W.R.: Equilibrium theory revisited: Factors influencing the position of the teeth, Angle Orthod. 48:175-186, 1978.







COMMENTS
.