CASE REPORT
Management of Alveolar Bone Exostosis after Orthodontic Treatment
Alveolar bone exostoses are benign localized outgrowths of buccal or lingual bone, consisting of mature cortical and trabecular bone.1-3 The etiology of alveolar bone exostosis is still unclear. Causes may include genetic and functional influences, racial or autosomal dominant factors, masticatory hyperfunction, continued jaw growth past the age of maturity, and even nutritional factors such as high levels of polyunsaturated fatty acids or vitamin D. These bony growths appear to have a genetic link, but environmental conditions can also influence their size.4-7
Depending on its location in the jaw, an alveolar bone exostosis can be classified as a torus palatinus, a sessile or nodular bony mass commonly seen in the midline of the hard palate; a torus mandibularis, a bony protuberance found on the lingual aspect of the mandibular canine-premolar region; a buccal bone exostosis, seen on the buccal aspect of the alveolar ridge; or other types. Diagnosis should be based on a clinical examination combined with radiographic findings. An exostosis should be differentiated from an osteoma, which is rare. A torus is often obvious, presenting as several rounded protuberances or calcified multiple lobules, whereas a buccal exostosis is singular and may appear as a sharp, pointed bony projection producing tenderness just under the mucosa. Histologically, the two types are indistinguishable. The exostosis presents as a hard bony mass on palpation, but the overlying mucosa will be intact and show normal color when stretched.8-10 Radiographically, these growths appear as well-defined round or oval calcified structures over the dental roots.11 The lesions do not have malignant transformation potential.
No treatment is required for an alveolar bone exostosis unless it is large enough to affect the periodontal tissue, cause pseudo-swelling of the lip, or produce pain or discomfort for the patient. Palatal or mandibular tori directly adjacent to the teeth can make hygiene more difficult, and they may have to be removed for prosthetic restorations. Buccal exostoses can become traumatized and not only interfere with oral hygiene, but also affect smile esthetics.3
Similar articles from the archive:
- CASE REPORT Orthodontic Movement of Posterior Teeth into a Corticocancellous Bone-Block Allograft Area July 2016
- Stress on Bone from Placement and Removal of Orthodontic Miniscrews at Different Angulations May 2009
- Bonding Interdental Retainers in Patients with Generalized Marginal Bone Loss June 2001
Many authors have reported the development of bony exostoses subsequent to dental procedures. Periodontal surgery causes trauma to local and adjacent tissues, which facilitates the activation of osteogenic progenitor cells leading to excessive bone growth. Moreover, patients presenting with tori or any type of bony exostoses are highly susceptible to bony overgrowth responses.12,13 Placement of a pontic denture over an edentulous ridge can lead to alveolar bone enlargement, known as subpontic osseous hyperplasia. Histological examination has shown these lesions to be composed of dense masses of mature bone with normally developed lamellae and Haversian systems.14,15 Another report described alveolar exostosis following orthodontic implant placement, but the pathogenesis was unclear.16 A possible explanation was that excessive mechanical load on the bone could induce the formation of exostoses.
The process involved in development of alveolar bone exostoses subsequent to orthodontic treatment is also uncertain, but some evidence indicates that it is related to alveolar bone thickening on the labial aspect caused by rapid upper incisor retraction.17 In that study, incisor inclination was associated with changes in overall bone thickness, especially at the apical level. The present article describes a case in which alveolar bone exostoses developed after orthodontic anterior retraction.
Diagnosis and Treatment Plan
A 28-year-old female presented with the chief complaint of “my front teeth sticking out” (Fig. 1). Clinical examination showed a symmetrical, round face with deficient lower facial height, a straight-to-convex profile, and a normal mandibular growth pattern. The patient had slightly incompetent lips at rest, with an interlabial gap of 4mm. The dental midlines were coincident with the facial midline. The canines were in a Class II relationship, but the molar relationship was Class I. Both arches exhibited mild crowding of the anterior teeth. The mandibular left first molar had undergone root-canal treatment with a poor restoration.
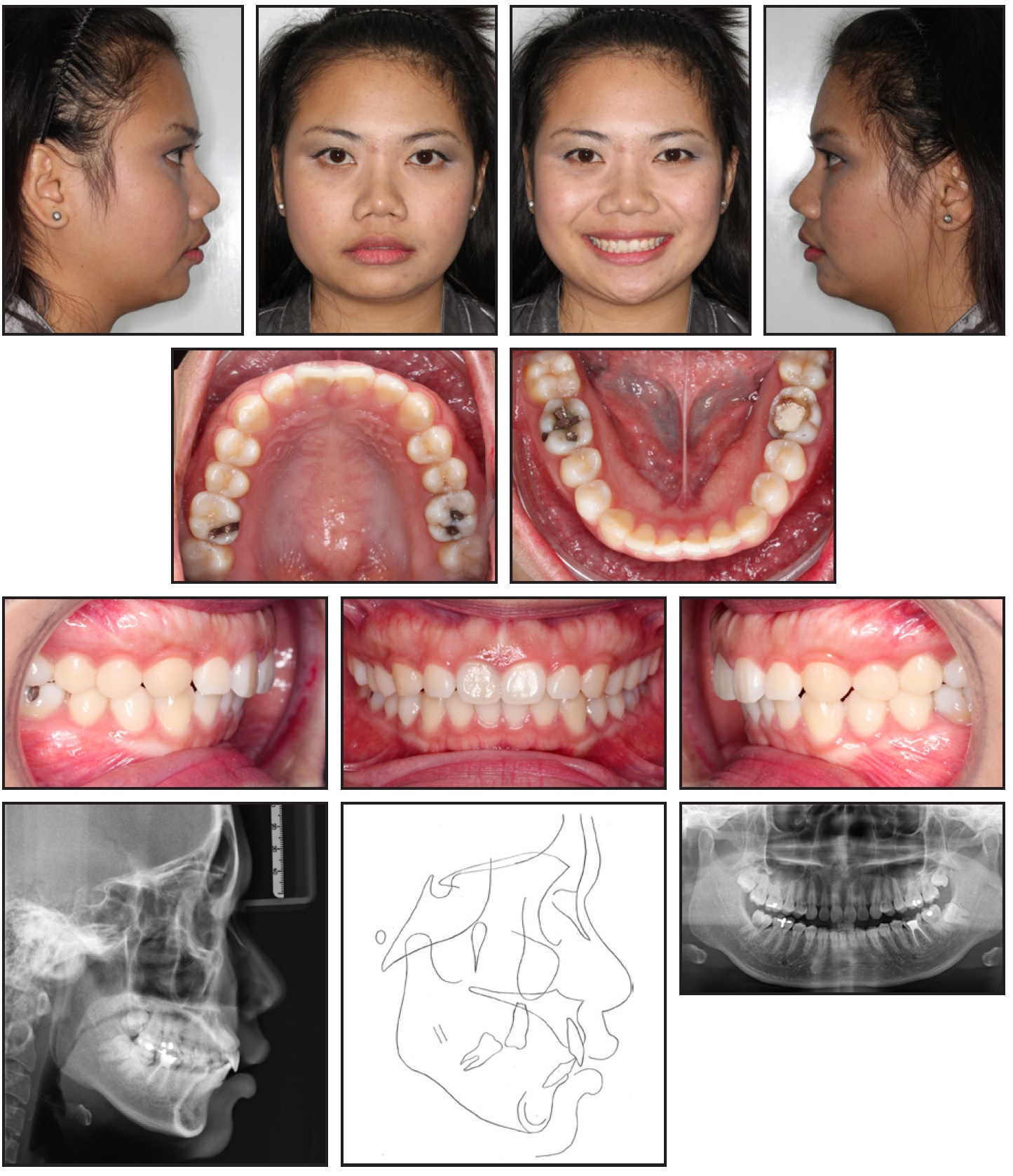
Fig. 1 28-year-old female patient with mild skeletal Class II relationship, Class I malocclusion, and normodivergent facial pattern with protrusive upper lip before treatment.
TMJ function was normal, with a normal range of motion and no jaw deviation on opening and closing. There were no signs of active periodontal disease.
The panoramic radiograph showed normal overall alveolar bone support and no pathological lesions. Cephalometric analysis indicated a mild skeletal Class II relationship (ANB = 6°) with a normal vertical facial configuration and normal maxillary incisor inclination and position (Table 1). The upper lip was protrusive, but the lower lip was normal relative to the E-line.
Orthodontic treatment objectives were to retract the upper and lower anterior teeth, establish a functional occlusion, achieve proper overjet and overbite, improve the lip relationship and the nasolabial angle, and ensure long-term stability.
Since the patient’s chief complaint was protrusion of the anterior teeth, we planned to use conventional orthodontic mechanics to retract the anterior teeth bodily, thus maintaining the normal incisor inclinations. Three extraction options were considered. The first called for extraction of the upper first premolar, lower right first premolar, and lower left first molar (the endodontically treated tooth). The second involved extraction of all four first premolars, combined with endodontic retreatment and proper restoration of the lower left molar. The third option was to remove the four first premolars and lower left first molar, followed by an implant to replace the lower left first molar. The first option was chosen by the patient.
The patient was referred for extraction of the upper third molars before orthodontic treatment, but the left lower third molar was preserved to occlude with the opposing tooth.
Treatment Progress
Treatment was initiated with an .022" × .028" Roth-prescription appliance in both arches and bonded tubes on the upper and lower molars. Leveling and alignment were carried out on .016", .016" × .022", and .019" × .025" nickel titanium archwires (Fig. 2). Because of the asymmetrical extractions, moderate posterior anchorage was used in the upper arch and the lower right quadrant, but minimal anchorage in the lower left quadrant.
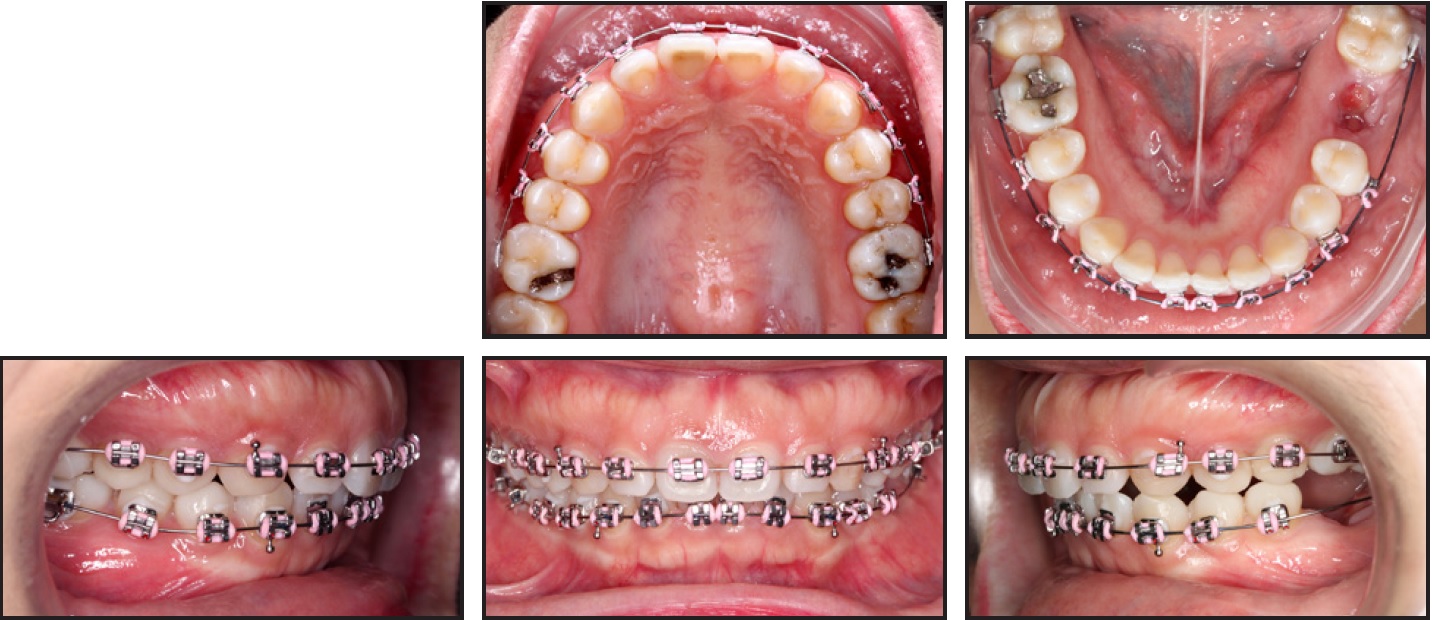
Fig. 2 After three months of leveling and alignment.
After three months of treatment, the canines were distalized for seven months on a rigid .019" × .025" stainless steel archwire. Retraction of the upper and lower incisors was completed in another five months (Fig. 3).

Fig. 3 After 12 months of retraction.
To prevent tipping during the anterior retraction, an upper sweep curve and a lower reverse curve of Spee were bent into the archwires. Class II intermaxillary elastics were used for mesialization of the lower left second molar. Finishing required 21 months because of the patient’s pregnancy.
After the spaces were closed and proper alignment was achieved, bony hard-tissue growths were noted on the buccal surfaces of the attached gingivae of the upper and lower anterior teeth. The bony lesions were hard and oval-shaped, and the overlying gingiva was pale and thin, indicating buccal alveolar bone exostoses. The patient also complained about traumatic ulceration when brushing her upper teeth. At this point, after 36 months of orthodontic treatment, the fixed appliances were removed and 4-4 lingual retainers were bonded in both arches (Fig. 4).
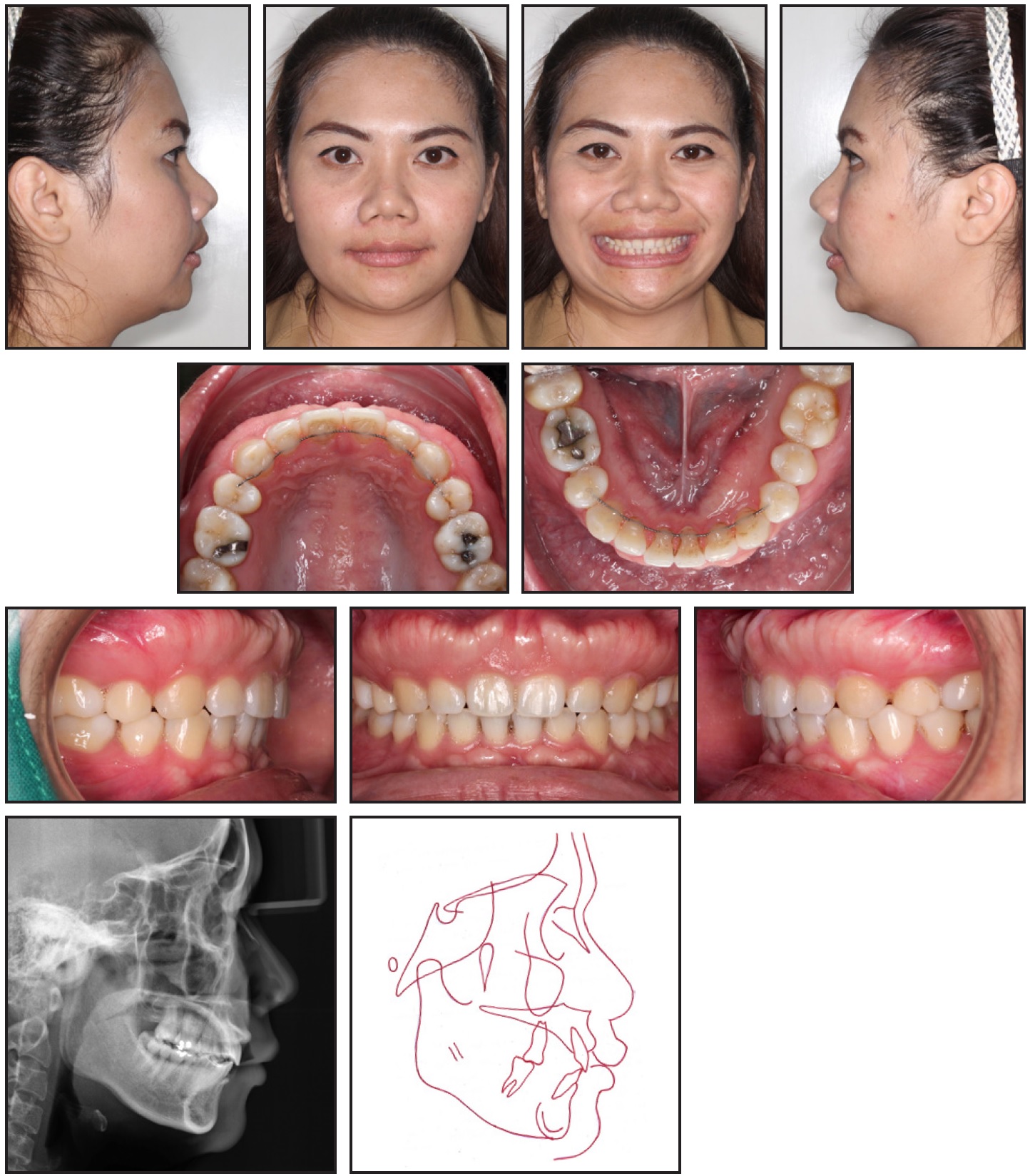
Fig. 4 After 36 months of treatment.
The decision was made not to remove the lower anterior exostosis, since it was less developed than the upper one and didn’t affect the patient’s esthetics and function. The patient was referred for alveoloplasty to remove the upper exostosis. Under local anesthesia, a full-thickness mucoperiosteal flap was reflected to provide clear access (Fig. 5). The bony protuberance was removed with a bone-cutting carbide bur under continuous saline irrigation, and the bone was then smoothed with a bone file. After the area was cleaned with normal saline solution, the flap was closed with 5.0 silk sutures. Antibiotics, analgesics, and .12% chlorhexidine gluconate mouthrinse were prescribed.

Fig. 5 Resective osseous surgery. A. Flap reflection revealing exostosis. B. After removal of bony mass with cutting carbide bur. C. After replacement of flap and suturing.
No postoperative complications occurred. A follow-up appointment was scheduled seven days after surgery to check the wound healing and remove the sutures (Fig. 6). There was no sign of infection at the surgical site, and periodontal health was acceptably maintained.

Fig. 6 Patient seven days after alveoloplasty.
Treatment Results
Post-treatment evaluation 15 months after surgery showed normal healing (Fig. 7). The patient exhibited a harmonious facial balance with improvement in the lateral profile and lip competence. She had good dental alignment, proper overjet, adequate overbite, a slightly Class II canine relationship, a Class I molar relationship on the right side, and a full-cusp Class II molar relationship on the left due to the asymmetrical extractions. The upper dental midline was coincident with the facial midline, but the lower dental midline was deviated to the right because of the Bolton discrepancy. The patient was satisfied with the outcome.
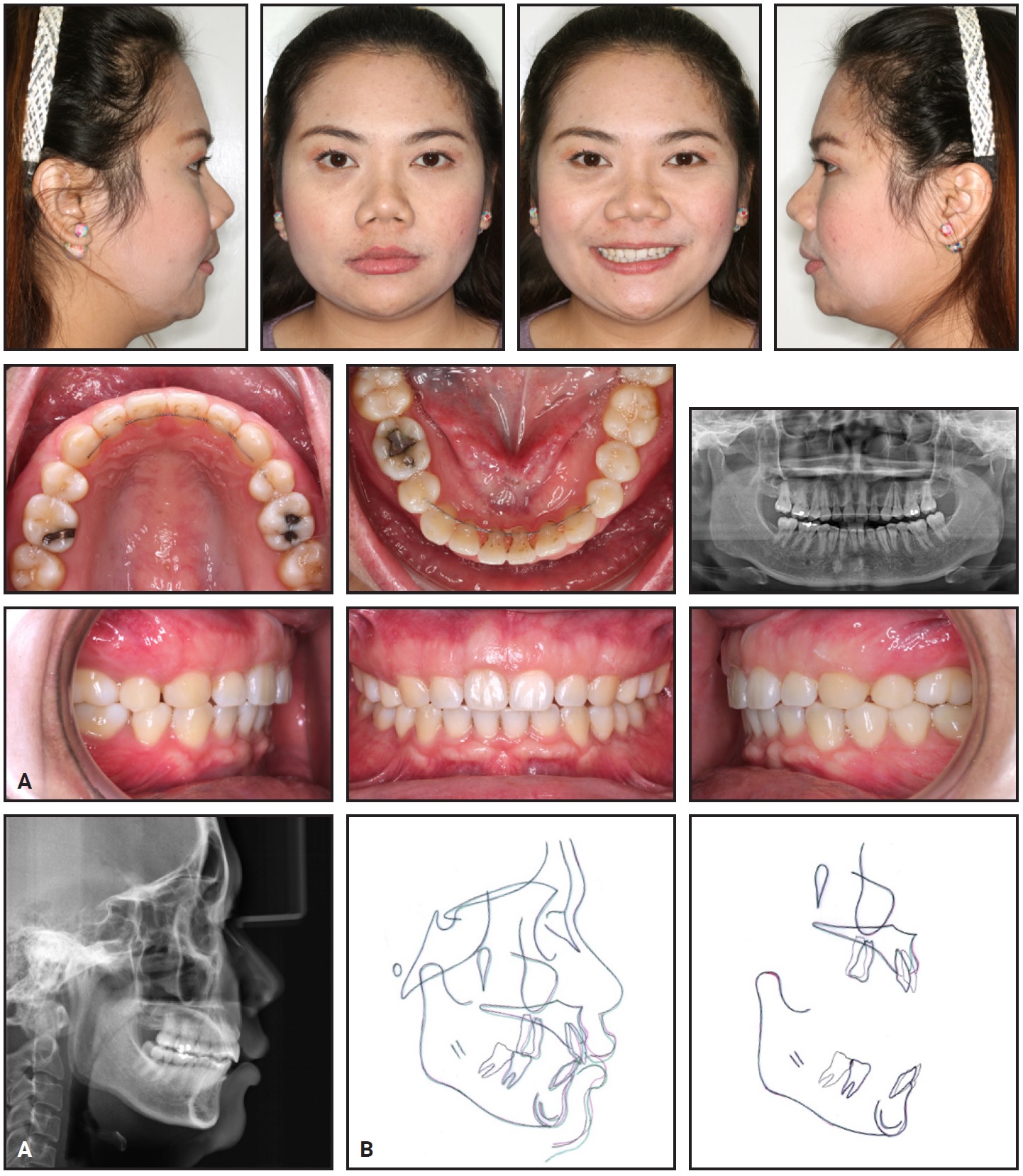
Fig. 7 A. Patient 15 months after alveoloplasty. B. Superimposition of cephalometric tracings (black = pretreatment, red = post-treatment, green = 15 months after alveoloplasty).
The panoramic radiograph indicated good periodontal health, with no significant bone loss or root resorption. Cephalometric analysis confirmed that the maxillary incisor inclination was maintained, and the lip position improved relative to the E-line (Table 1). Superimpositions showed posterior movement of the maxillary and mandibular incisors and intrusion of the mandibular incisors. The upper first molar and lower second molar moved forward into a normal occlusion. A cephalometric measurement—the distance from the most prominent point of the upper alveolar bone to a line through N point perpendicular to the Frankfort horizontal plane—was devised to evaluate changes in upper alveolar bone thickness (Fig. 8). This measurement increased from 10mm before orthodontic treatment to 11.5mm after treatment; 15 months after the alveoloplasty, it was significantly reduced to 7.5mm. Combined with an increase in the nasolabial angle (from 89° to 106°), this resulted in an improved facial profile and upper lip.
Discussion
Harmonious texture, shape, color, and architecture of the gingival tissue are crucial to smile esthetics, especially in females, and can thus enhance self-esteem.18 In the present case, an unsightly smile due to buccal alveolar bone exostoses developed after orthodontic treatment. While it was not a major problem for this patient, owing to her low smile line and lack of gingival display, the bony protuberance strained and thickened her upper lip muscle.

Fig. 8 Distance from most prominent point of upper alveolar bone to line through N point perpendicular to Frankfort horizontal plane, used to evaluate changes in upper alveolar bone thickness.
Although an exostosis usually requires no treatment, it can be removed with minor osseous surgery to restore the patient’s gingival architecture, reduce lip strain, avoid food retention above the bone, and reduce traumatic ulceration during oral hygiene.19 In addition, because the protuberant bony masses tend to interfere with the U-loops of removable retainers, we bonded fixed retainers in this case.
Caucasian women tend to prefer fuller lips than Asian women, who prefer more retrusive lips.20 Since our patient’s chief complaint was her protrusive front teeth, extractions were required to retract the anterior teeth and improve her lip position. Considering her normal incisor display and anatomical crown width-length ratios, the resective bone surgery alone was sufficient to improve the appearance of her smile. If the buccal bone exostosis had been accompanied by excessive gingival display or a gummy smile, a crown-lengthening procedure could have been performed to remove alveolar bone and excessive gingiva.21
The prevalence of buccal exostoses varies among studies, most likely because of racial and ethnic differences, with higher rates seen in Mongoloids than in Caucasoids.22 In addition, maxillary tori have been found more frequently in women, and mandibular tori more often in men.23,24 Alveolar exostoses in both the maxilla and the mandible are most commonly seen in young adults and in middle-age patients.25 Because they tend to develop during the teenage years and may expand over time, there are few reports of alveolar exostoses in children or pre-teens.
Although bone exostoses are non-malignant lesions of unknown, multifactorial etiology, they may represent a response to occlusal trauma. Glickman and Smulow, observing new bone formation on the external surfaces of the alveolar ridge on both sides of traumatized teeth, suggested that a buttressing bone formation occurs to reinforce trabecular bone as a means of functional adaptation.26 Our case report illustrates the development of alveolar bone exostoses that enlarged after the retraction of upper anterior teeth. Many factors may contribute to changes in alveolar bone thickness during incisor retraction, including the rate of tooth movement, the degree of buccolingual inclination, the extent of upper incisor intrusion, and the use of orthodontic implants.16,17 In our case, the rapid rate of incisor retraction and bodily tooth movement might have been responsible. The buttressing bone formation could have been a response to trauma from orthodontic forces, which resulted in the release of bone morphogenic proteins, expressed as exostoses ossifying at the points of stress.25
Cortical bone remodeling from tooth movement is different in the anteroposterior, vertical, and transverse directions.27 Vertically, orthodontic extrusion can increase tooth displacement faster than bone apposition, leading to an increase in clinical crown height. On the other hand, intrusion can maintain a 1:1 ratio between bone remodeling and tooth movement, resulting in bone reduction after intrusive movements. In the transverse direction, rapid expansion may cause dehiscence and fenestration of the buccal cortical plate. In the sagittal dimension, considerable evidence indicates that the ratio of bone remodeling to anterior tooth movement is not constant.28 In our case, the exostoses occurred after the anterior teeth had been retracted into the extraction spaces, indicating that the remodeling of cortical bone—particularly the resorption on the tension side—could not catch up with the tooth movement.
While traditional cephalometric radiographs are routinely obtained prior to treatment, the best way to evaluate hard-tissue changes in the alveolar bone is through three-dimensional cone-beam computed tomography.29,30 Since this was unavailable in the present case, we devised a cephalometric measurement to assess changes in upper alveolar bone thickness.
ACKNOWLEDGMENT: The authors would like to express their appreciation for the enthusiastic encouragement of staff at the Faculty of Dentistry, Khon Kaen University and for their valuable support in the present study.
REFERENCES
- 1. Neville, B.W.; Damm, D.D.; Allen, C.M.; and Bouquot, J.E.: Oral and Maxillofacial Pathology, W.B. Saunders Co., Philadelphia, 1995.
- 2. Regezi, J.A. and Sciubba, J.J.: Oral Pathology: Clinico-Pathologic Correlations, W.B. Saunders Co., Philadelphia, 1989.
- 3. Medsinge, S.V.; Ramesh, K.; Harmeeta, B.; and Atamjeet, S.: Buccal exostosis: A rare entity, J. Int. Oral Health 5:62-64, 2015.
- 4. Haugen, L.K.: Palatine and mandibular tori: A morphologic study in the current Norwegian population, Acta Odontol. Scand. 50:65-77, 1992.
- 5. Gorsky, M.; Raviv, M.; Kfir, E.; and Moskona, D.: Prevalence of torus palatinus in a population of young and adult Israelis, Arch. Oral Biol. 41:623-635, 1996.
- 6. Seah, Y.H.: Torus palatinus and torus mandibularis: A review of the literature, Austral. Dent. J. 40:318-321, 1995.
- 7. Eggen, S. and Natvig, B.: Relationship between torus mandibularis and number of present teeth, Scand. J. Dent. Res. 94:233-240, 1986.
- 8. Smitha, K. and Smitha, G.P.: Alveolar exostosis revisited: A narrative review of the literature, Saudi J. Dent. Res. 2014.
- 9. Eversole, L.R.: Clinical Outline of Oral Pathology: Diagnosis and Treatment, Lea & Febiger, Philadelphia, 1978.
- 10. Antoniades, D.Z.; Belize, M.; and Papanayiotou, P.: Concurrence of torus palatinus with palatal and buccal exostoses: Case report and review of the literature, Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 85:552-557, 1998.
- 11. Bouquot, J.E.: Bond’s Book of Oral Diseases, 4th ed., Churchill-Livingstone, Philadelphia, 1988.
- 12. Pack, A.R.; Gaudie, W.M.; and Jennings, A.M.: Bony exostosis as a sequela to free gingival grafting: Two case reports, J. Periodontol. 62:269-271, 1991.
- 13. Chambrone, L.A. and Chambrone, L.: Bony exostoses developed subsequent to free gingival grafts: Case series, Br. Dent. J. 199:146-149, 2005.
- 14. Caiman, H.I.; Eisenberg, M.; Grodjesk, J.E.; and Szerlip, L.: Shades of white: Interpretation of radiopacities, Dent. Radiog. Photog. 44:3-10, 1971.
- 15. Takeda, Y.; Itagaki, M.; and Ishibashi, K.: Bilateral subpontic osseous hyperplasia: A case report, J. Periodontol. 59:311-314, 1988.
- 16. Agrawal, N.; Kallury, A.; Agrawal, K.; and Nair, P.P.: Alveolar bone exostoses subsequent to orthodontic implant placement, BMJ Case Rep. 25:2012007951, doi: 10.1136/bcr-2012-007951, 2013.
- 17. Yodthong, N.; Charoemratrote, C.; and Leethanakul, C.: Factors related to alveolar bone thickness during upper incisor retraction, Angle Orthod. 83:394-401, 2013.
- 18. Shaw, W.C.: The influence of children’s dentofacial appearance on their social attractiveness as judged by peers and lay adults, Am. J. Orthod. 79:399-415, 1981.
- 19. Lestari, C.; Marlie, H.; and Orienty, F.N.: Treatment of bilateral maxillary buccal exostoses on gummy smile, Bali Med. J. 7:736-740, 2018.
- 20. Gao, Y.; Niddam, J.; Noel, W.; Hersant, B.; and Meningaud, J.P.: Comparison of aesthetic facial criteria between Caucasian and East Asian female populations: An esthetic surgeon’s perspective, Asian J. Surg. 41:4-11, 2018.
- 21. Capelozza Filho, L.; Cardoso, M.A.; Reis, S.A.B.; and Mazzottini, R.: Surgical-orthodontic correction of long-face syndrome, J. Clin. Orthod. 40:323-332, 2006.
- 22. Reichart, P.A.; Neuhaus, F.; and Sookasem, M.: Prevalence of torus palatinus and torus mandibularis in Germans and Thais, Comm. Dent. Oral Epidemiol. 16:61-64, 1988.
- 23. Sonnier, K.E.; Homing, G.M.; and Cohen, M.E.: Palatal tubercles, palatal tori, and mandibular tori: Prevalence and anatomical features in a U.S. population, J. Periodontol. 70:329-336, 1999.
- 24. Shah, D.S.; Sanghavi, S.J.; Chawda, J.D.; and Shah, R.M.: Prevalence of torus palatinus and torus mandibularis in 1000 patients, Ind. J. Dent. Res. 3:107-110, 1992.
- 25. Horning, G.M.; Cohen, M.E.; and Neils, T.A.: Buccal alveolar exostoses: Prevalence, characteristics, and evidence for buttressing bone formation, J. Periodontol. 71:1032-1042, 2000.
- 26. Glickman, I. and Smulow, J.B.: Buttressing bone formation in the periodontium, J. Periodontol. 36:365-367, 1965.
- 27. Vardimon, A.D.; Oren, E.; and Ben-Bassat, Y.: Cortical bone remodeling/tooth movement ratio during maxillary incisor retraction with tip versus torque movements, Am. J. Orthod. 114:520-529, 1998.
- 28. Remmelink, H.J. and Van der Molen, A.L.: Effects of anteroposterior incisor repositioning on the root and cortical plate: A follow-up study, J. Clin. Orthod. 18:42-49, 1984.
- 29. Maki, K.; Inou, N.; Takanishi, A.; and Miller, A.J.: Computer-assisted simulations in orthodontic diagnosis and the application of a new cone beam x-ray computed tomography, Orthod. Craniofac. Res. 6:95-101, 2003.
- 30. Hassan, B.; Setelt, P.; and Sanderink, G.: Accuracy of three-dimensional measurements obtained from cone beam computed tomography surface-rendered images for cephalometric analysis: Influence of patient scanning position, Eur. J. Orthod. 23:1-6, 2008.






COMMENTS
.