Back-to-Work Coronavirus Infection Control
The COVID-19 pandemic shut down orthodontic practices nationwide for at least six weeks. Orthodontists saw patients only for emergency and urgent care, following strict infectious-disease precautions. As isolation, social distancing, and stay-at-home orders “flattened the curve” for the highly infectious SARS-CoV-2 virus, orthodontic offices began gradually reopening for much-needed patient care.
Safe orthodontic practice during this transitional phase—which will likely last until sufficient vaccines, therapeutics, and immunity have been developed—requires the implementation of special airborne-disease transmission precautions, in addition to the Centers for Disease Control and Prevention (CDC) Standard Precautions. On April 27, the ADA published a comprehensive “Return to Work Interim Guidance Toolkit” for dental practices. The toolkit provides COVID-19 infection-prevention protocols under the following headings:
- Welcome Back Reassurance
- Pre-Appointment Screening Process
- In-Office Patient Registration Procedures
- Reception Area Preparation
- Chairside Checklist
- Staff Protection
- Shopping List
- Appendix
Similar articles from the archive:
The novel coronavirus is transmitted mainly through aerosol droplets. Protecting patients and staff from potentially contaminated aerosols by using proper infection-control protocols will reduce the risk of airborne-disease transmission and help ensure the safety of both patients and staff. In general, however, dental procedures generate a greater volume of aerosols than orthodontic procedures do. Let’s review how the ADA “Return to Work Interim Guidance Toolkit” applies to orthodontic practices.
Welcome Back Reassurance
You need to announce to patients that the practice is reopening and let them know what to expect at their appointments during this phase. Many resources are available to help you reassure patients and enthusiastically say, “Welcome back—we missed you!” (Fig. 1). Use multiple methods of communication—letters, e-mails, texts, social media posts, website posts, and personal phone calls. Patients and parents may be anxious about their safety; this is the time to provide reassurance. Let them know you have been busy during the closure implementing infection-control protocols as recommended by the CDC. Include information on appointment scheduling and check-in procedures, such as: “Only the patient will enter the office. Parents and siblings, please wait in the car.” Tell them how to communicate with the office by text or phone when they arrive for the appointment, and that a “greeter” will meet the patient at the car or the door.
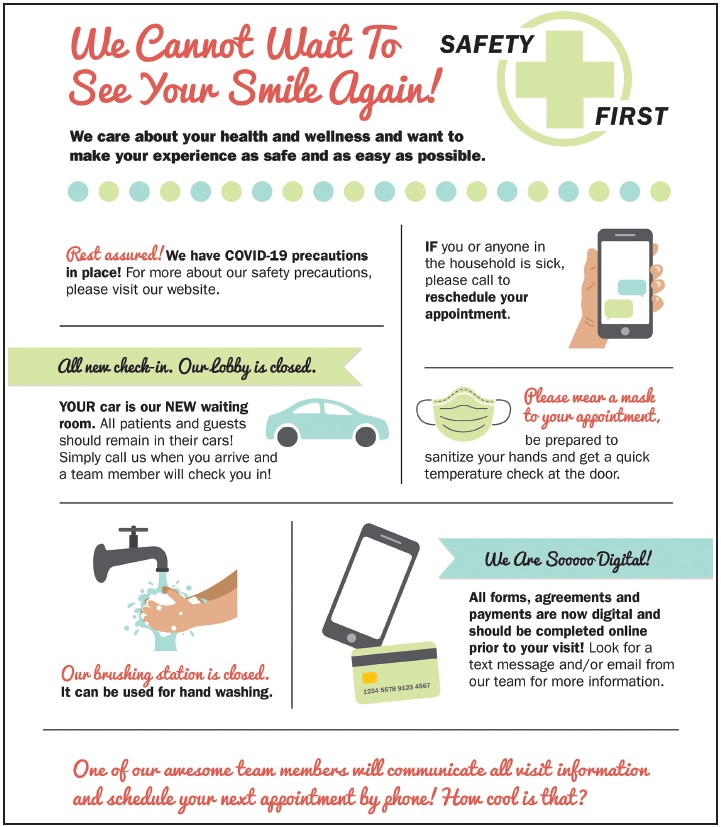
Fig. 1 “Welcome Back” message to patients (image courtesy of Virginia Creative Group and Allison Parks Hale, Smart Practice Consulting, Yorktown, VA).
Pre-Appointment Screening Process
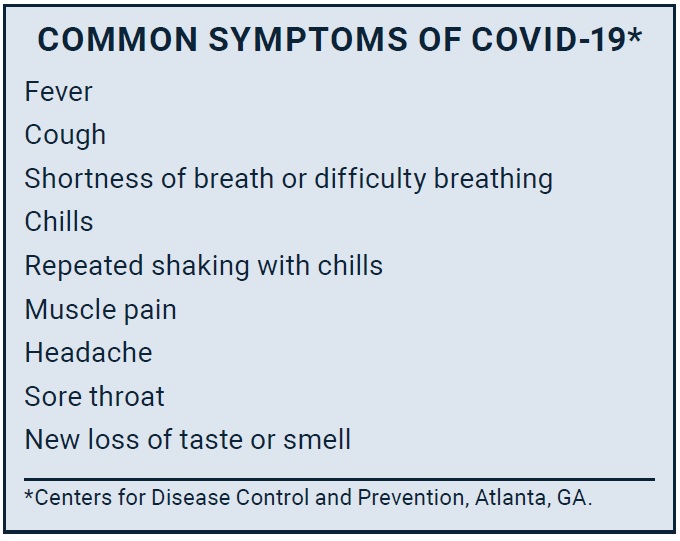
Before patients arrive for their orthodontic appointments, they need to answer wellness screening questions to help determine if they are at a high risk of being infectious for SARS-CoV-2. Do they have any of the COVID-19 symptoms? Do they have a fever? Have they been around an infected person? Have they traveled to an area of high infectivity? Are they at higher risk because of being immune-compromised? Let patients know that these new precautions are out of concern for their health and well-being. If a patient answers “yes” to any of the screening questions, the office staff should review the situation with the doctor before scheduling an appointment.
The pre-appointment screening notice should remind patients of the following points:
- Their temperature will be taken.
- They should bring their own mask (to preserve PPE for the clinical staff).
- They should brush and floss at home, since the toothbrushing sinks will be closed.
- Only the patient will enter the office, unless there are special circumstances.
- If parents come in, they will need to undergo wellness screening and a temperature check.
As part of the screening process, ask about broken or loose appliances. If a bracket is off, it may require scheduling an “aerosol procedure appointment,” which involves more time and different personal protective equipment (PPE) compared with a “non-aerosol procedure appointment.” The AAO COVID-19 Task Force has provided members with aerosol and non-aerosol procedure lists that include PPE recommendations.
As you reopen your practice, plan for a reduced appointment schedule to allow time for the wellness screening, social distancing for patient flow and seating, additional PPE donning and doffing time, and the initial anxiety of patients and the orthodontic team. You may want to spread out your appointment hours over longer daily periods and more days of the week. Start slow, and as the team and patients master the new changes, you can gradually increase patient flow.
In-Office Patient Registration Procedures
The designated greeter meets the patient at the car or the office door with a “welcome back” greeting. For a child patient, do the initial screening at the car. Ask an older patient to sit in a screening chair in the entry or by the front door. Take the patient’s temperature. If it is higher than 100.4°F, reschedule the appointment; if lower, ask the patient to put on a mask, review the wellness screening, and offer the patient hand sanitizer. A tablet can be used to record the wellness screening as an aseptic alternative to a paper form. Walk the patient to the orthodontic clinic, stopping at the closed toothbrushing sink for an optional mouthrinse (this can also be done at the chair), with the patient expectorating into the cup that contained the mouthrinse.
When the patient arrives at the chair, the orthodontist and assistant should be waiting in the appropriate PPE for the procedure. After the appointment is complete, the greeter returns to escort the patient back to the reception room (or to the car, in the case of a young child or special-needs patient); the return walk should go through a hall other than the entry, if possible. The greeter can then communicate information about the appointment to the parent, with all further documentation and communication handled electronically.
Reception Area Preparation
The patient screening chair can be positioned in the entryway, in a hall outside the office, or by the front door. Set a table beside the chair with the necessary wellness screening equipment: thermometer, masks, hand sanitizer, disinfectant wipes, tissue, exam gloves, trash can, and paper forms or digital recording device.
In the reception area, separate patient seating by at least six feet; if you cannot remove chairs, place barriers over enough chairs to maintain proper spacing. Remove all magazines, toys and games, tablets, and refreshment amenities to prevent cross-contamination. Set up a barrier—a “sneeze shield” type—on the front-desk counter, and indicate the six-foot distance with floor markings such as colorful tape or decals. The greeter and receptionist should wear ASTM Level 1 masks and gloves as needed. Limit paperwork as much as possible. Maintain a schedule for cleaning and disinfection of all surfaces in the reception area and bathrooms. We love our orthodontic patients, but no handshaking or hugging at this time.
Chairside Checklist
Prior to reopening, all the equipment in the sterilization room must be cleaned, restarted, and tested. Clean the sterilizer according to the manufacturer’s instructions, and run a spore test. Instrument washers and ultrasonic cleaners must also be cleaned and tested. Chairside closed-water systems (water bottles) should be shock-treated and tested, with results of less than 500 CFU/ml for heterotrophic bacteria.
For adequate distancing, schedule non-aerosol appointments at every other chair in an open bay. Aerosol treatment chairs should be isolated. For a non-aerosol procedure, PPE includes a gown, Level 3 (or possibly 2) surgical mask, face shield, and exam gloves (Fig. 2). An aerosol procedure requires an N95 respirator mask instead of a surgical mask. During the current PPE shortage, the CDC and Occupational Safety and Health Administration (OSHA) have published reuse protocols for both kinds of masks. An N95 respirator mask can be reused if removed aseptically, stored in a paper bag, and labeled with the wearer’s name. A surgical mask can be worn for more than one patient, as long as it is not removed between patients. Adding a face shield protects either kind of mask from spatter and splash on its exterior surface. Another option for protecting the N95 mask exterior is to wear a cloth or surgical mask over the N95 mask, with safety glasses or goggles for eye protection.

Fig. 2 Robin Horne, orthodontic assistant at Parks Orthodontics, Yorktown, VA, wears disposable isolation gown (with tie back and knit cuffs) over scrubs, nitrile gloves, ASTM Level 2 surgical mask with face shield, and surgical bonnet while working with a patient (image courtesy of Allison Parks Hale, Smart Practice Consulting, Yorktown, VA).
After the greeter escorts the patient to the chair, the orthodontist and assistant review the scheduled treatment with the patient, sanitize their hands, put on gloves, and perform the procedure. Any additional instruments, supplies, or lab items needed during the appointment are delivered by a floating assistant.
After the patient exits the chair for a non-aerosol procedure, the orthodontist and assistant remove their gloves, sanitize their hands, and move on to the next patient chair. After an aerosol procedure, they should discard their disposable gowns or place reusable gowns in a contaminated laundry container marked with a biohazard symbol for reprocessing.
Designating a floating assistant and a sterilization technician will preserve PPE supplies and save time. The sterilization technician is responsible for handling contaminated instruments and disinfecting treatment chairs between patients. All contaminated instruments must be processed according to CDC-recommended protocols: clean, rinse, dry, inspect, package, sterilize, and store the sterile packaged instruments inside a cabinet or drawer.
After each appointment, the sterilization technician removes barriers and disinfects the treatment chair, delivery unit, and equipment, using an Environmental Protection Agency (EPA)-approved health-care disinfectant (Fig. 3). Be sure to verify that the disinfectant is effective against the SARS-CoV-2 virus by consulting EPA List N: Disinfectants for Use Against SARS-CoV-2. Pay careful attention to the contact time—the amount of time the surface should be visibly wet, as listed in the EPA table.
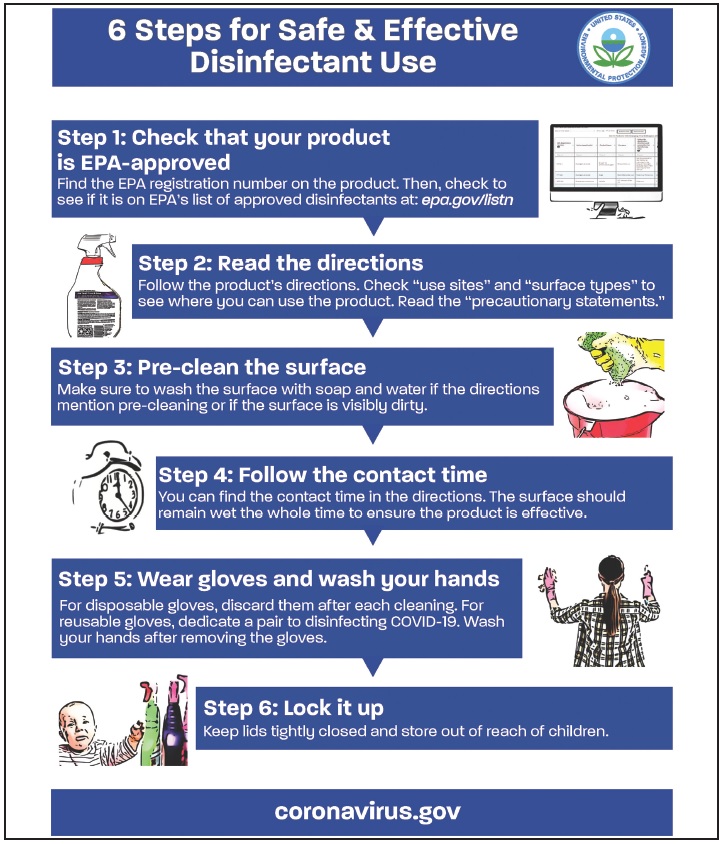
Fig. 3 Recommended use of disinfectants (image courtesy of Environmental Protection Agency, Washington, DC).
The sterilization assistant prepares the chair for the next appointment by replacing the barriers and setting packaged sterile instrument kits on the delivery unit.
Use the CDC dental checklist to review all your infection-control procedures, including PPE, hand hygiene, instrument sterilization, disinfection, and contaminated sharps management. The interactive CDC DentalCheck app can be downloaded to a smartphone or tablet. After completing the checklist, you can save the document as your orthodontic practice infection-control plan.
Staff Protection
Implement a daily employee wellness screening and temperature check. Team members who arrive at work with fevers above 100.4°F or COVID-19 symptoms should go home. They should not return to work until they are free of fever (without taking fever-reducing medicine) and have no symptoms for at least 24 hours. The ADA’s Interim Guidance recommends that team members change into scrubs when arriving at the office and change out of scrubs at the end of the day. Scrubs can be laundered in the office or taken home in a plastic bag for laundering. The scrubs are protected from aerosol contamination by an isolation gown or clinic jacket, either disposable or laundered in the office or by a commercial laundry. Leaving shoes at the office is optional.
Information on the effects of COVID-19 in pregnancy is very limited. As a precaution, pregnant staff members may be assigned to non-aerosol duties and patient care.
Shopping List
Because infection-control products are currently in short supply, it is important to plan ahead—both to ensure adequate inventory and to allow for delivery delays and back orders. Many orthodontic practices have had to delay reopening because they did not have adequate PPE supplies. A PPE Burn Rate Calculator is available on the CDC website to help calculate how many gowns, masks, shields, and gloves will be needed for scheduled patients.
Supply chains are being replenished, but it will take some time. The ADA Interim Guidance warns practices to be careful of “gray market” products that do not meet official U.S. standards and could therefore put patients and staff at risk.
Appendix
The ADA toolkit appendix includes patient letter templates, a wellness screening log sheet, and information on masks and shields.
Conclusion
Back-to-work coronavirus infection control will be a challenge at first for the orthodontic team. Orthodontists and practice administrators should allow time for training and practice in donning and doffing PPE, wellness screening, and social distancing. Careful preparation will ensure calm and confidence as you reopen your doors and welcome back patients.



COMMENTS
.