Delayed Extraction of the Mesial First-Molar Root as a Means of Accelerating Space Closure
Because the first molar is one of the first permanent teeth to erupt, it can be lost to decay at an early age.1 In such a case, protracting the second and third molars to close the first-molar extraction space can avoid the need for a future prosthesis.2 Protracting the lower molars is not a simple procedure, however, because a considerable amount of root movement is needed, potentially leading to such problems as soft-tissue folding (gingival clefting), periodontal problems, or root resorption.3-5
Biomechanical considerations are among the many factors involved in protraction. The orthodontic force must pass through the center of resistance of the protracted tooth or teeth to avoid tipping movement. In addition, because soft-tissue folding during space closure may cause alveolar bone resorption, a guided bone regeneration procedure or other measures should be considered to prevent bone loss.6 A third concern is traumatic occlusion of the protracted molars, which can produce severe mobility and periodontal bone destruction. The molar should be protracted with slight intrusion to prevent trauma, and protraction can be enhanced by taking the molar out of occlusion. The final and most important consideration is the atrophy of edentulous alveolar bone.7 Alveolar bone constricts about 34% in an edentulous area during the five years following tooth extraction,8 with the most bone resorption occurring during the first six months. Tooth movement, therefore, slows over time. It may be advantageous to extract only the distal root of the first molar, maintaining the mesial root until the protracted second molar moves closer.
Similar articles from the archive:
This report compares the treatment time, mode of tooth movement, and periodontal conditions in two patients of similar age who needed first-molar extraction spaces closed and the second and third molars protracted. In one patient, extraction of the mesial root of the lower first molar was delayed, and in the other, both first-molar roots were extracted before the second molar was protracted.
Case 1
A 15-year-old female presented with a hopeless lower left first molar with periapical pathosis (Fig. 1).

Fig. 1 Case 1. 15-year-old female patient with hopeless lower left first molar before treatment.
She was referred for extraction of the first molar and protraction of the second and third molars to close the space. To minimize the risk of alveolar bone atrophy, the first molar was hemisected, and only the distal root was extracted before orthodontic mechanics were initiated.
Two small-headed, 6mm micro-implants* were placed into the buccal alveolar bone between the lower left first and second premolars (Fig. 2A). The micro-implants were tied together with stainless steel ligature wire and built up with composite resin. A standard .018" upper-incisor bracket was bonded to the composite (Fig. 2B), a tube was bonded to the lower second molar, and an .017" × .025" TMA** sectional wire was inserted to connect the bracket and tube.
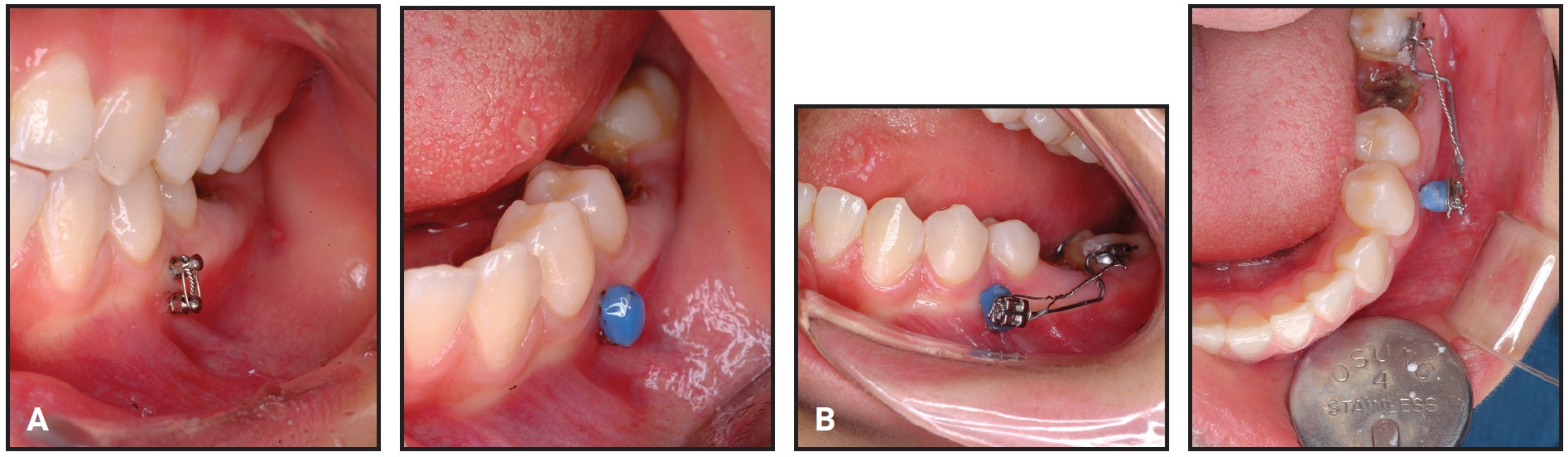
Fig. 2 Case 1. A. Two micro-implants* placed between lower left first and second premolars and built up with composite. B. Bracket bonded to composite and connected to second-molar tube with TMA** sectional wire.
The ligature wire was tightened every four weeks for reactivation.
We decided to protract the second molar with slight intrusion to facilitate tooth movement. To prevent extrusion of the upper molars, brackets were bonded and a sectional wire was placed.
The lower second molar was slightly intruded by the sectional archwire, taking it out of occlusion (Fig. 3).
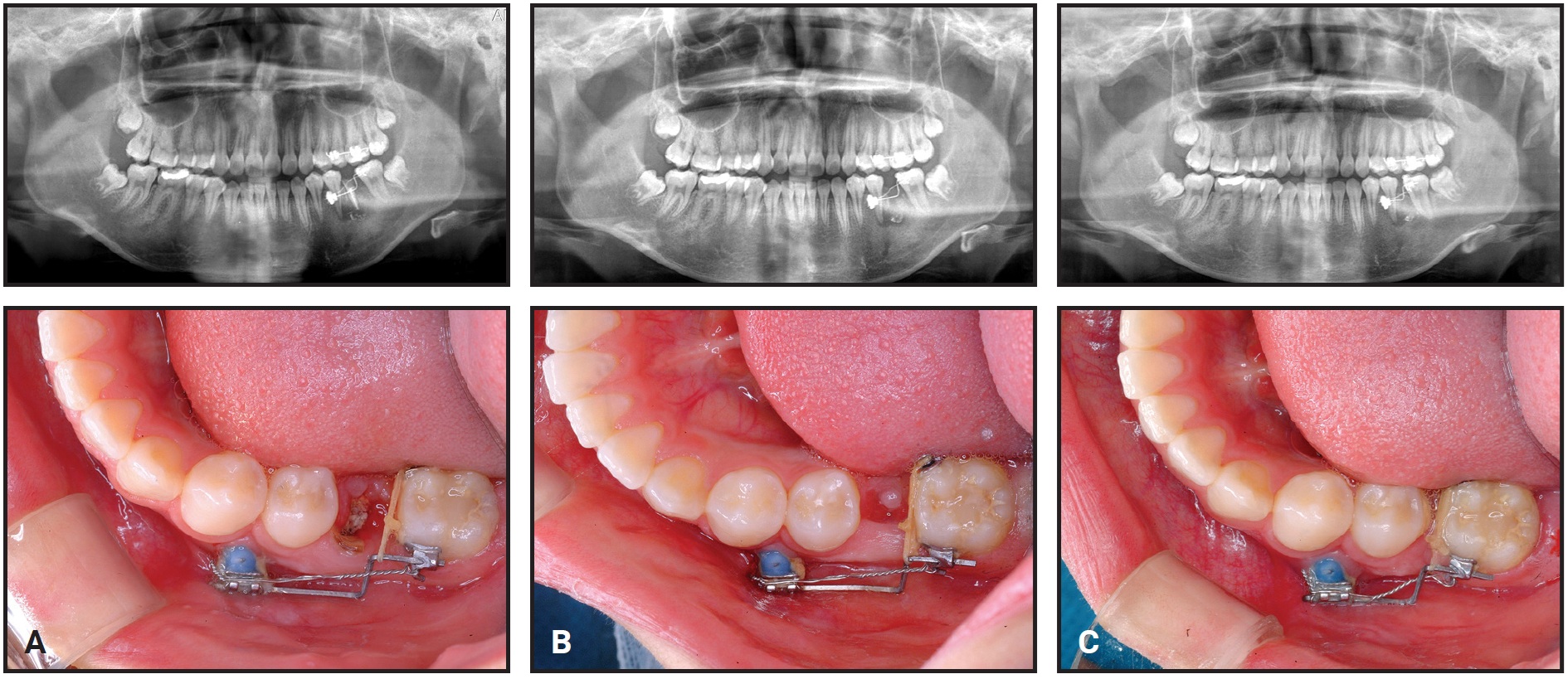
Fig. 3 Case 1. A. After two months of treatment, with first-molar mesial root remaining. B. Mesial root of first molar extracted after three months of treatment. C. After nine months of treatment, edentulous space almost closed.
After three months of protraction, the space created by extraction of the distal root was closed, and the mesial first-molar root was extracted. To prevent mesial tipping of the second molar, a tipback bend was made in the TMA wire. After nine months of treatment, the space was almost closed.
The third molar spontaneously moved mesially, following the protracted second molar. A gingivectomy was performed on the third molar, and a bracket was bonded for uprighting. After 16 months of treatment, the second and third molars were aligned into occlusion (Fig. 4).
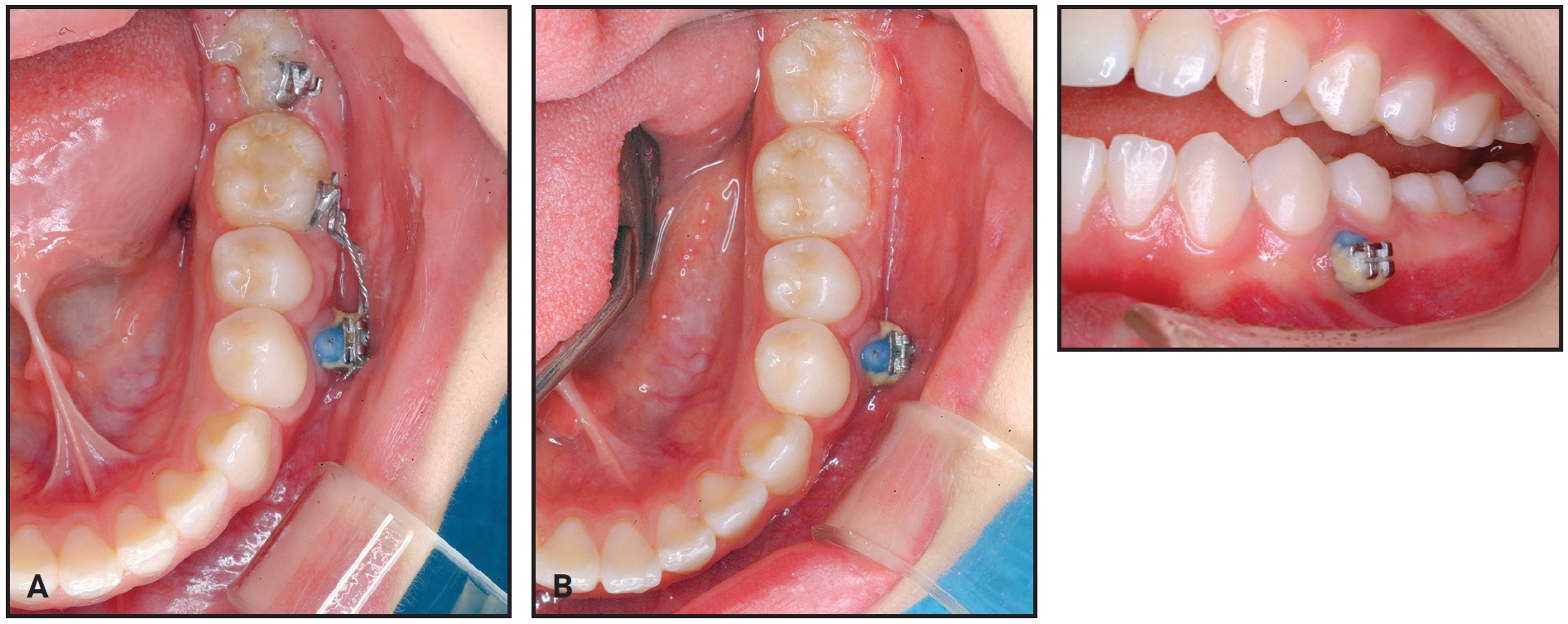
Fig. 4 Case 1. A. Spontaneous mesial movement of third molar after 13 months of treatment. B. Three months later, molars aligned into occlusion.
After six months of retention, the micro-implants were removed (Fig. 5).
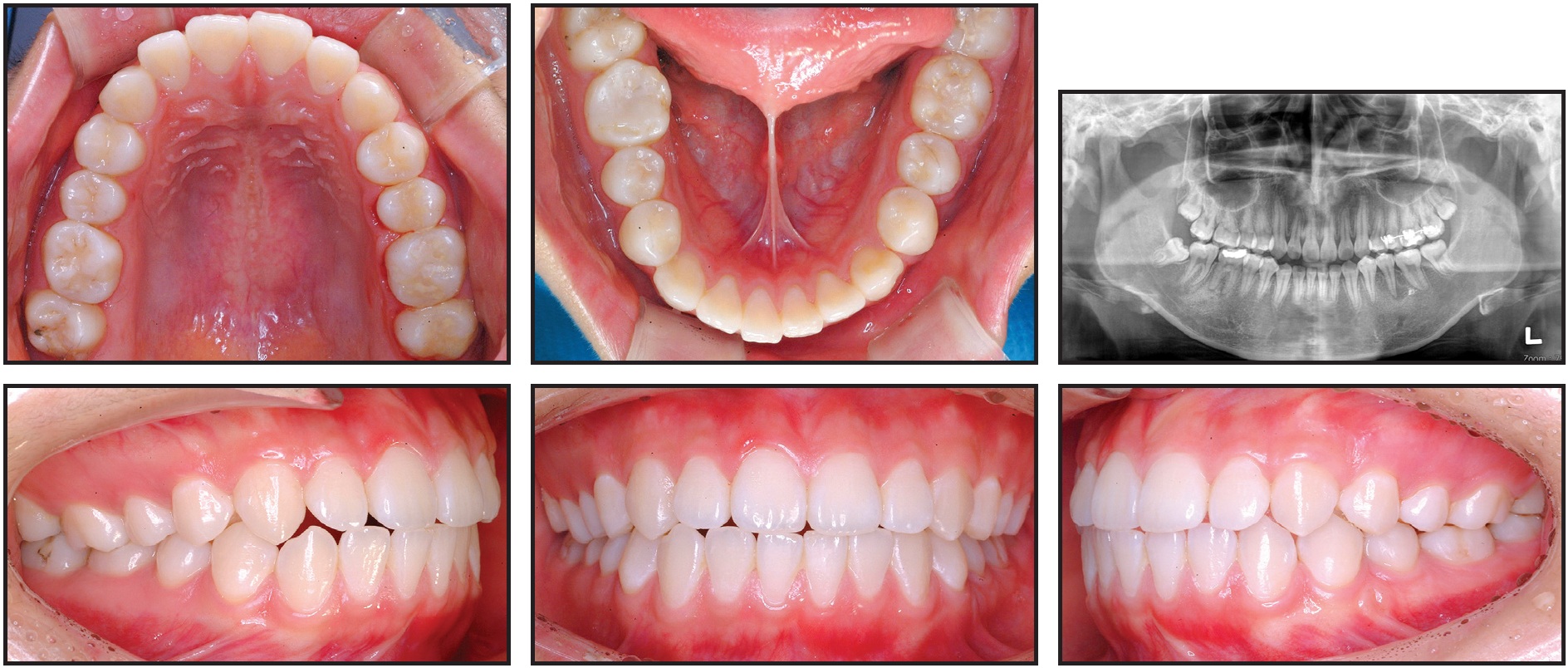
Fig. 5 Case 1. After six months of retention, favorable occlusion observed and micro-implants removed.
Records showed a well-maintained occlusion without root resorption or alveolar bone loss. The teeth displayed almost bodily movement without tipping, and no side effects, including alveolar bone atrophy, inflammation, soft-tissue clefting, or root resorption, were observed.
Case 2
A 16-year-old female scheduled for prosthodontic treatment was referred for intrusion of an overerupted upper right first molar after decay of the lower first molar (Fig. 6).

Fig. 6 Case 2. 16-year-old female patient with extracted lower right first molar and extruded upper right first molar before treatment.
The patient presented with the lower right molar already extracted, so intrusion of the upper right first molar and protraction of the lower right second and third molars were planned.
Two small-headed micro-implants were placed in the buccal (7mm) and palatal (10mm) sides of the upper right posterior area, and an intrusion force was applied to the upper right first molar (Fig. 7).
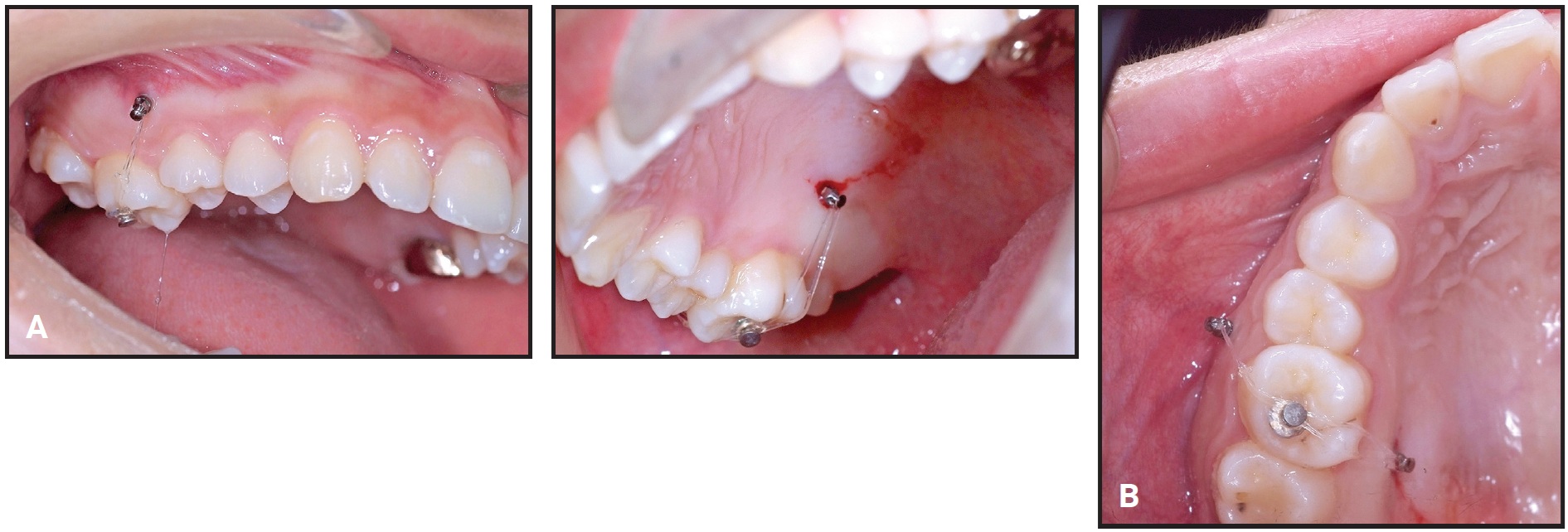
Fig. 7 Case 2. A. 7mm micro-implant placed in upper right posterior bone on buccal side and 10mm micro-implant on palatal side. B. Intrusion force applied to upper right first molar.
After a modest amount of intrusion had been achieved, protraction of the lower second and third molars was started to close the extraction space with micro-implant anchorage.
After six weeks of treatment, two small-headed 6mm micro-implants were placed into the buccal alveolar bone between the lower right first and second premolars, tied with a stainless steel ligature wire, and built up with composite resin, as in Case 1 (Fig. 8). A standard .018" upper-incisor bracket was bonded to the composite, a tube was bonded to the lower second molar, and an .017" × .025" TMA sectional wire was inserted. Reactivation was performed by tightening the ligature wire every four weeks (Fig. 9).

Fig. 8 Case 2. A. Bracket bonded over two micro-implants between lower right first and second premolars, as in Case 1. B. Mesial force applied with TMA sectional wire.
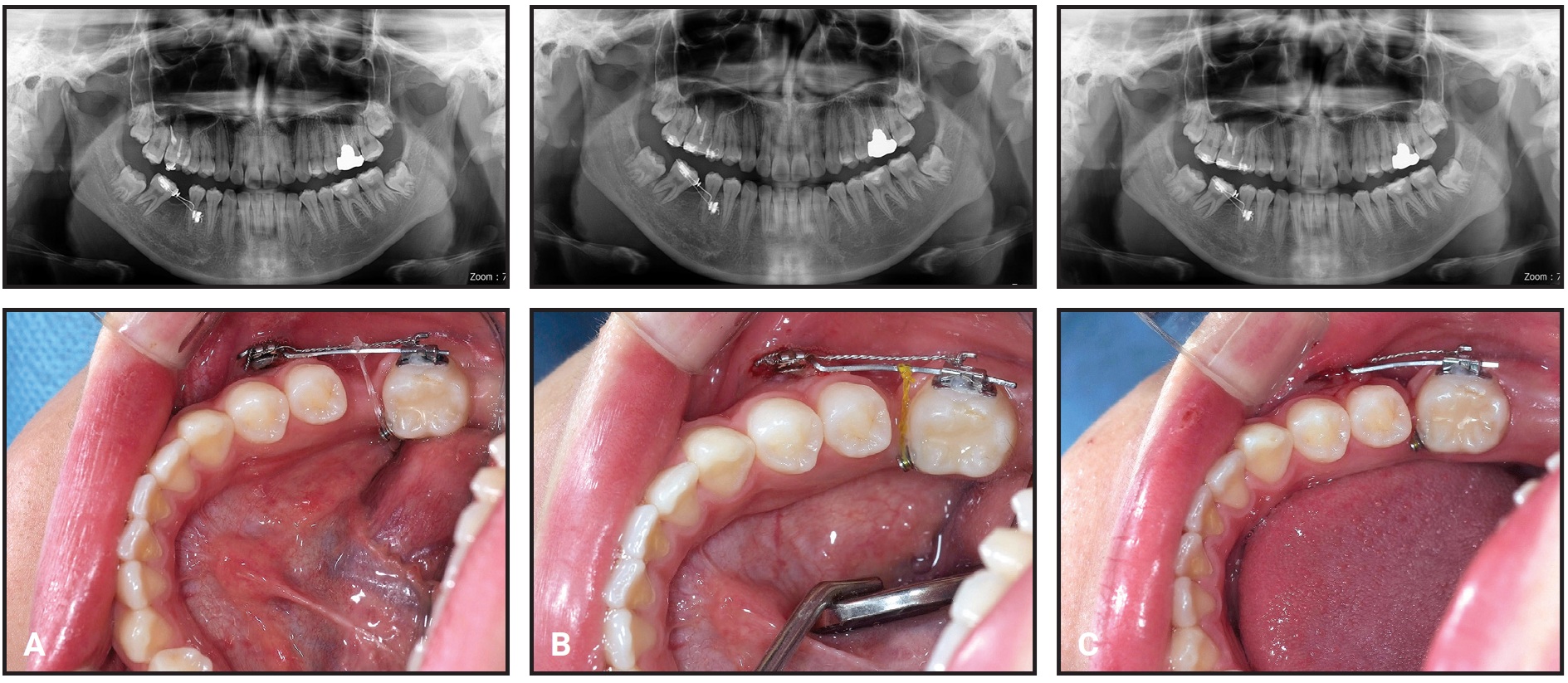
Fig. 9 Case 2. Mesial tipping of lower right second molar and development of bone atrophy near first-molar extraction space during protraction. A. After six months of treatment. B. After 10 months of treatment. C. After 14 months of treatment.
The intrusion force was applied continuously to the upper right first molar, and the lower second molar was intruded slightly by the sectional archwire to avoid occlusal contact during protraction. Panoramic radiographs indicated forward tipping of the lower second molar rather than bodily movement.
After 20 months of treatment, most of the lower right first-molar space had been closed by the mesial movement of the second molar. A gingival cleft had developed as a result of soft-tissue folding, and bone loss on the mesial side of the lower right second molar was evident on a panoramic radiograph at 24 months (Fig. 10).
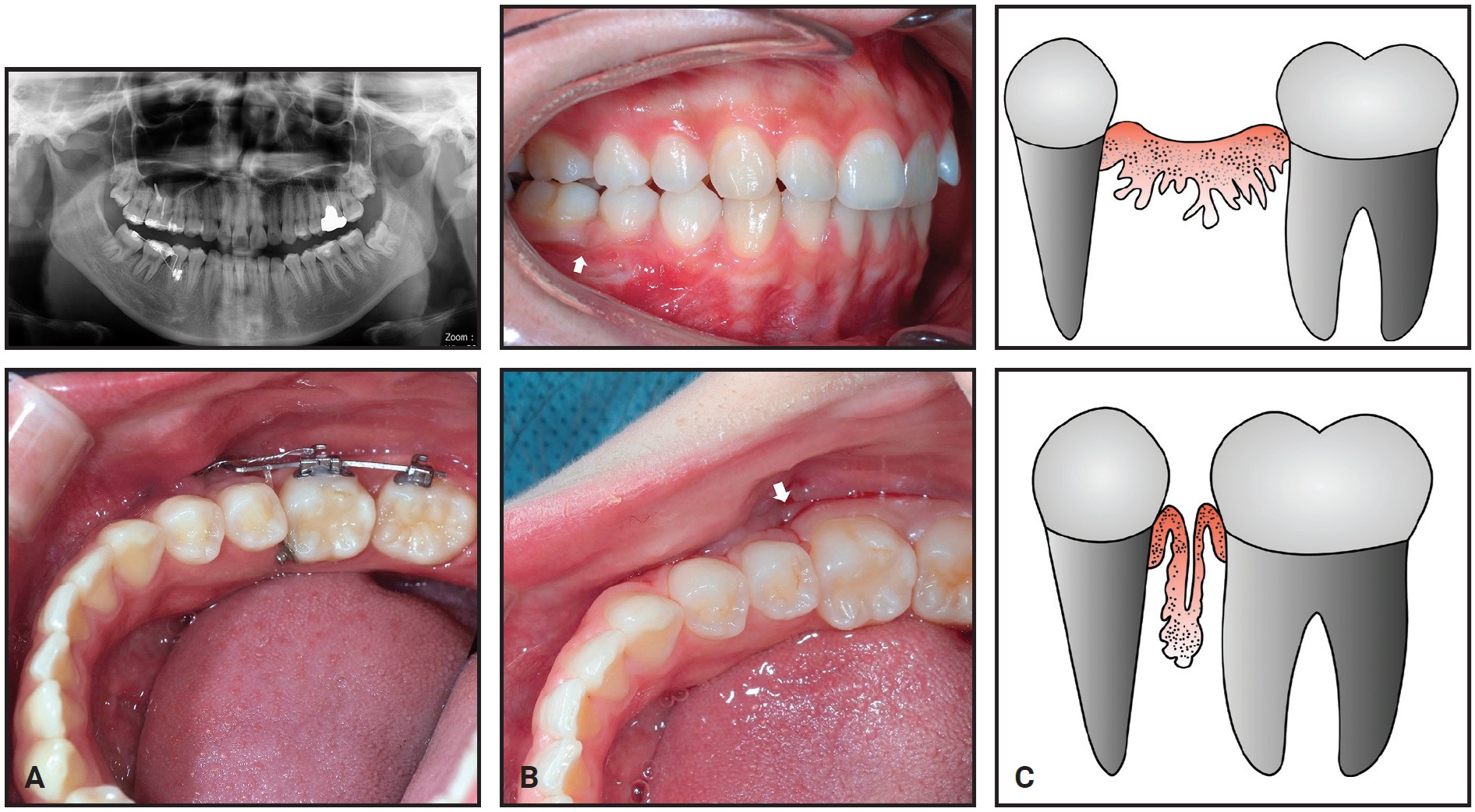
Fig. 10 Case 2. A. Gingival cleft caused by soft-tissue folding after 24 months of treatment, with bone loss apparent on mesial side of lower right second molar. B. Gingival cleft evident in interproximal area of second premolar and protracted second molar. C. Illustration of gingival cleft caused by closure of edentulous space.
Total treatment time was 27 months (Fig. 11). The post-treatment records showed the gingival cleft between the second premolar and the protracted second molar, bone resorption in the mesial part of the second molar, and apical root resorption of the protracted second molar. In addition, bone atrophy in the buccolingual dimension was observed in the bone between the second premolar and the second molar.

Fig. 11 Case 2. Patient after 27 months of treatment.
Discussion
When a patient presents with a missing first molar, closing the edentulous space by protraction of the second molar may be an effective treatment option for proper bone support and oral hygiene.2 The timing of the lower first-molar extraction can greatly affect the duration and outcome of orthodontic treatment. The first-molar roots can be hemisected to postpone extraction of the mesial half.
In both cases shown here, the edentulous space created by extraction of a lower first molar was closed by mesial movement of the lower second and third molars. Treatment was finished about 10 months sooner in Case 1, the patient in whom extraction of the mesial molar root was delayed. This patient also showed bodily tooth movement during the protraction of the second molar, whereas the second patient exhibited tipping movement from the beginning of protraction.
Both the buccolingual and the apicocoronal dimensions of the alveolar ridge are reduced at the edentulous site following tooth extraction.9,10 One study found the buccolingual width of the alveolar bone can be constricted by as much as 23% during the first six months after an extraction and 34% five years after the extraction.8 If the buccolingual width of the edentulous alveolar bone decreases, the rate of tooth movement also decreases. Delayed extraction of the first molar’s mesial root will maintain bone volume in the mesial half of the extraction site, without affecting the rate of protraction.
The regional acceleratory phenomenon (RAP) in the alveolar bone typically occurs during the healing of the alveolar sockets after tooth extraction.11 The RAP is a hard- or soft-tissue reaction to a noxious stimulus that increases the healing capacities of the affected tissues.11 Therefore, the rate of tooth movement will be accelerated upon extraction of the distal first-molar root, and another RAP may occur when the mesial root is extracted. In addition, one study found that the extraction sockets of dogs were filled with woven bone one month after extraction, and the woven bone was being replaced with lamellar bone and bone marrow six months after extraction.12 This suggests that if the time period from the extraction of the first molar to the protraction of the second molar is longer than six months, bone formation in the extraction socket will have progressed further, and that the tooth movement will eventually slow down. Delayed extraction of the mesial root of the lower first molar will therefore reduce maturation of the bone in the mesial half of the extraction site. Movement of the tooth into immature bone may be two to three times faster than movement into mature bone.13 The continuous RAP, the delayed maturation of bone at the extraction site, and the preservation of alveolar bone width might all explain the faster and more bodily movement seen in Case 1. A shorter treatment also carries less risk of root resorption.
In Case 1, no alveolar bone resorption or buccolingual alveolar bone atrophy was seen. On the other hand, in Case 2, where the entire first molar was extracted before treatment, we observed buccolingual alveolar bone atrophy and resorption of anterior alveolar bone, as well as more periapical resorption of the protracted second molar.
The overlying soft tissue on the edentulous ridge eventually matures after molar extraction. Because soft tissue remodels more slowly than the bone does, this mature soft tissue may fold down and produce a soft-tissue cleft during space closure (Fig. 10C). In Case 1, the presence of the mesial root prevented soft-tissue maturation and may thus have reduced the risk of developing a soft-tissue cleft. In Case 2, the soft-tissue folding caused bone resorption, which can be accelerated when a patient has poor oral hygiene.14 If a large edentulous space is involved, guided bone regeneration should be considered to prevent such bone resorption.6 A preventive gingival graft or apically repositioned flap can be considered ahead of space closure, or the folded soft tissue can be removed.
FOOTNOTES
- *Dentos, Daegu, Korea; www.dentos.co.kr. Distributed by Great Lakes Orthodontics, Tonawanda, NY; www.greatlakesortho.com.
- **Trademark of Ormco Corporation, Orange, CA; www.ormco.com.
REFERENCES
- 1. Roberts, W.E.: Edentulous spaces in the mandibular posterior segments, in Decision Making in Dental Treatment Planning, 2nd ed., ed. W.B. Hall, A.H. Gluskin, W.E. Roberts, and E.E. LaBarre, Mosby, St. Louis, 1998, pp. 177-179.
- 2. Stepovich, M.L.: A clinical study on closing edentulous spaces in the mandible, Angle Orthod. 49:227-233, 1979.
- 3. Apajalahti, S. and Peltola, J.S.: Apical root resorption after orthodontic treatment: A retrospective study, Eur. J. Orthod. 29:408-412, 2007.
- 4. Robertson, P.B.; Schultz, L.D.; and Levy, B.M.: Occurrence and distribution of interdental gingival clefts following orthodontic movement into bicuspid extraction sites, J. Periodontol. 48:232-235, 1977.
- 5. Atherton, J.D.: The gingival response to orthodontic tooth movement, Am. J. Orthod. 58:179-186, 1970.
- 6. Pinheiro, M.L.; Moreira, T.C.; and Feres-Filho, E.J.: Guided bone regeneration of a pronounced gingiva-alveolar cleft due to orthodontic space closure, J. Periodontol. 77:1091-1095, 2006.
- 7. Atwood, D.A.: A cephalometric study of the clinical rest position of the mandible, Part II: The variability in the rate of bone loss following the removal of occlusal contacts, J. Prosth. Dent. 7:544-552, 1957.
- 8. Carlsson, G.E.; Bergman, B.; and Hedegård, B.: Changes in contour of the maxillary alveolar process under immediate dentures: A longitudinal clinical and x-ray cephalometric study covering 5 years, Acta Odontol. Scand. 25:45-75, 1967.
- 9. Lekovic, V.; Camargo, P.M.; Klokkevold, P.R.; Weinlaender, M.; Kenney, E.B.; Dimitrijevic, B.; and Nedic, M.: Preservation of alveolar bone in extraction sockets using bioabsorbable membranes, J. Periodontol. 69:1044-1049, 1998.
- 10. Schropp, L.; Wenzel, A.; Kostopoulos, L.; and Karring, T.: Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study, Int. J. Period. Restor. Dent. 23:313-323, 2003.
- 11. Verna, C.: Regional acceleratory phenomenon, Front. Oral Biol. 18:28-35, 2016.
- 12. Cardaropoli, G.; Araújo, M.; and Lindhe, J.: Dynamics of bone tissue formation in tooth extraction sites: An experimental study in dogs, J. Clin. Periodontol. 30:809-818, 2003.
- 13. Sanjideh, P.A.; Rossouw, P.E.; Campbell, P.M.; Opperman, L.A.; and Buschang, P.H.: Tooth movements in foxhounds after one or two alveolar corticotomies, Eur. J. Orthod. 32:106-113, 2010.
- 14. Wehrbein, H.; Bauer, W.; and Diedrich, P.R.: Gingival invagination area after space closure: A histologic study, Am. J. Orthod. 108:593-598, 1995.




COMMENTS
.