Differential Diagnosis and Treatment of Condylar Hyperplasia
Facial asymmetry has been categorized as congenital, originating prenatally; developmental, occurring during growth with uncertain etiology; or acquired, due to injury or disease.1-3 A variety of diagnostic aids, including sequential study models, radiographs, and scintigraphy, are used to identify the probable cause, which, in turn, determines the appropriate mode of therapy. The TMJ and condyles are the source of most postnatal facial asymmetries, with unilateral condylar hyperplasia a common pathology.4 Condylar hyperplasia can been classified as hemimandibular elongation, in which the mandible displaces horizontally toward the unaffected side; hemimandibular hyperplasia, in which there is three-dimensional enlargement of the mandible through the midline; or a combination of the two.5 A recent classification by Wolford and colleagues described four types of condylar hyperplasia based on age of onset, clinical characteristics, imaging, and histology.6
True condylar hyperplasia develops between puberty and the cessation of growth at age 18-25.7,8 Treatment usually involves condylectomy of the condyle that has continued to grow and a reduction of maxillary bone to correct the occlusal cant. Bilateral sagittal split osteotomies are often performed to close the lateral open bite on the affected side and correct the midline.9
This article shows how a radiographically evident condylar hyperplasia can be successfully managed as a case of condylar hypoplasia.
Similar articles from the archive:
Case Report
A 22-year-old male patient presented with the chief complaint of progressively increasing deviation of the chin to the right side (Fig. 1).
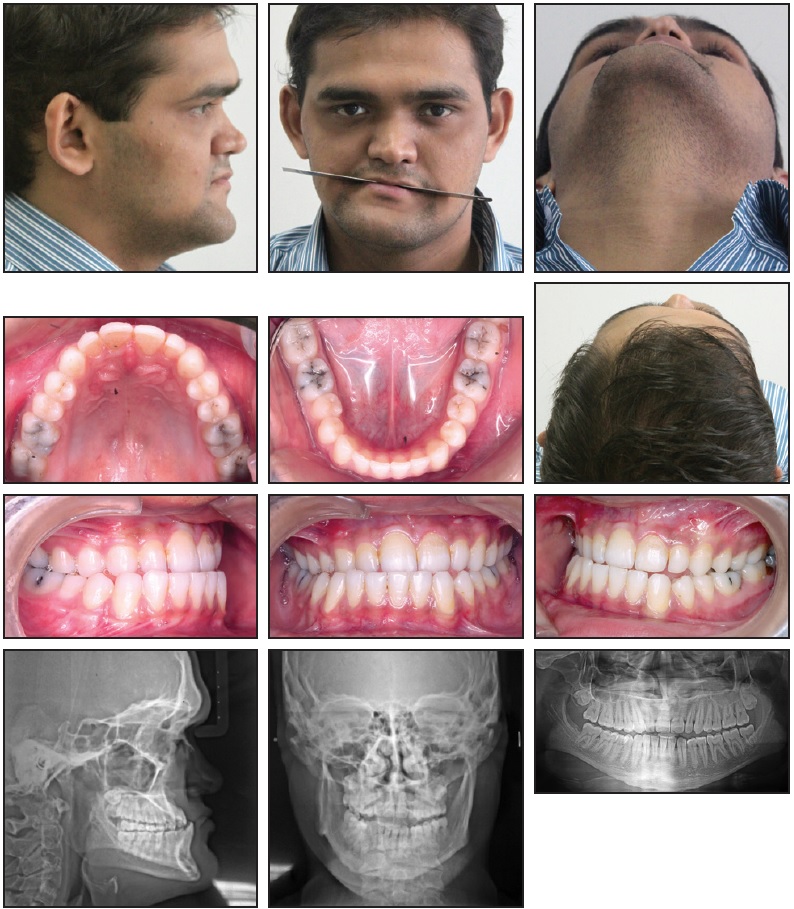
Fig. 1 22-year-old male patient with facial asymmetry, chin and midline deviation to right, canted occlusal plane, and Class III skeletal pattern before treatment.
The patient had experienced a fall from stairs when he was 7 years old, but reported no visible injury or treatment at that time. Clinical examination revealed marked asymmetry in the middle and lower thirds of the face, with a canted oral rim, chin deviation to the right, concave profile, depressed nasal bridge, and malar deficiency. The right side of the face appeared shorter than the left; the chin was deviated to the right, and there was a midface deficiency. Both arches were well aligned, but in complete crossbite. The lower midline was shifted 4mm to the right, and the occlusal plane was canted downward on the left. The upper and lower first molars were carious.
A panoramic radiograph showed an elongated left condyle with a deep masseteric notch. The left ramus was longer and narrower than the right, and the right antegonial notch was deeper than the left, with longer body length on the left.
The lateral cephalogram indicated a Class III skeletal pattern with a retrognathic maxilla and prognathic mandible (SNA = 79°, SNB = 89°, ANB = −10°), as well as a horizontal growth pattern (FMA = 9°). The maxilla was small in terms of both effective and absolute length (CoA = 76mm, ANS-PNS = 43mm). The effective mandibular length from the left condylion to left gnathion was within normal limits (117mm), but the right half of the mandible was notably shorter. The maxillary incisors were proclined (U1-NA = 50°, 10mm), and the mandibular incisors were retroclined (L1-NB = 18°, 2mm).
The posteroanterior cephalogram revealed marked asymmetry in the lower two-thirds of the face. The chin point was deviated to the right (Me-MSR = 6mm) because of the shorter lower border of the mandible on the right (Ag-Me = 43mm) than on the left (50mm). The vertical dimension of the maxilla was also shorter on the right (Cg-J = 94mm) than on the left (103mm), and the right ramus (Co-Ag = 53mm) was shorter than the left (63mm). In summary, the patient had a facial asymmetry with the left side of the face appearing longer, even though its measurements were within the norms.
To assess the cause of asymmetry, a technetium (Tc) 99m scan was used to reconstruct single-photon emission computerized tomography (SPECT) images (Fig. 2).
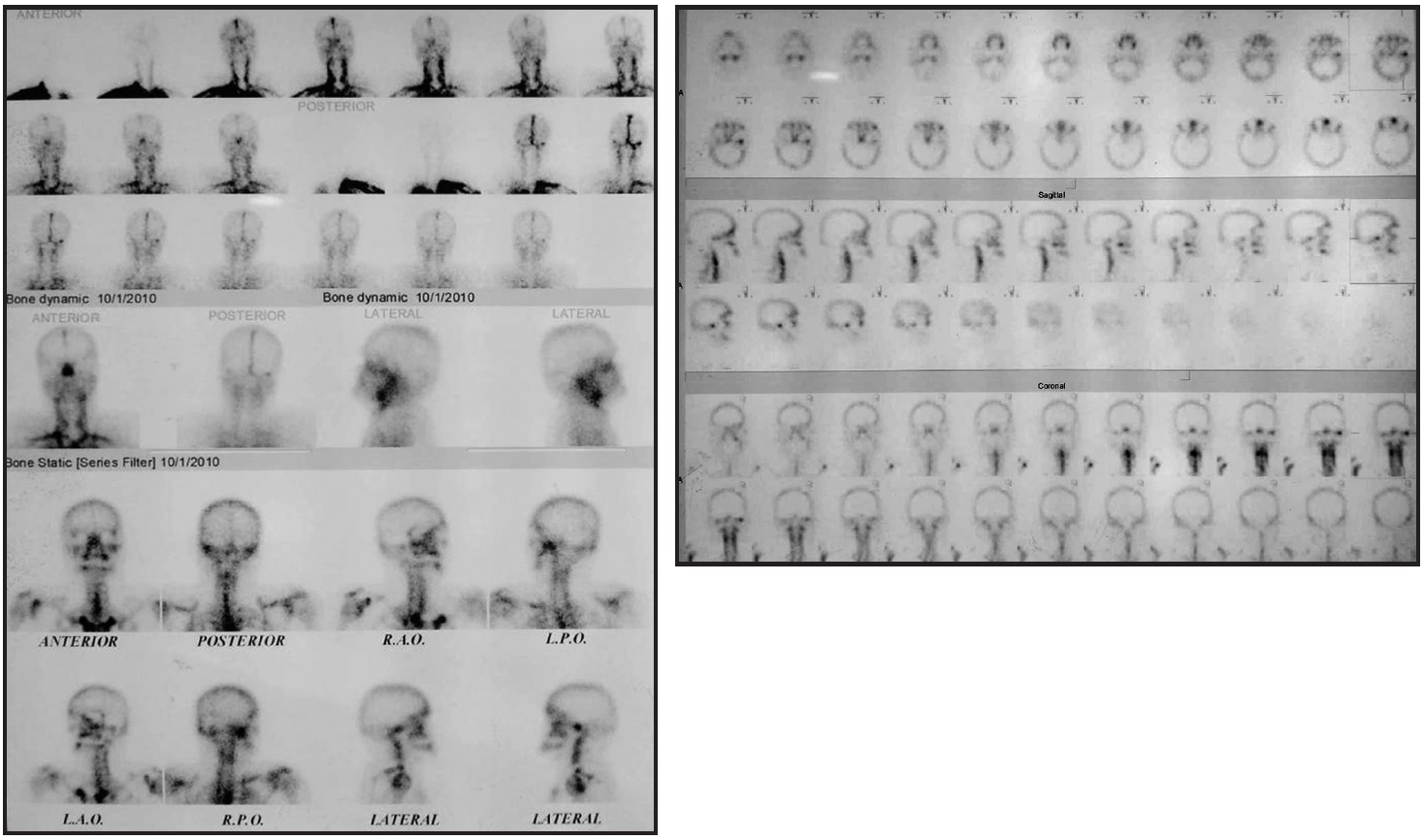
Fig. 2 Single-photon emission computerized tomography shows increased uptake in left condyle, indicating left condylar hyperplasia.
The increased uptake in the left condyle indicated left condylar hyperplasia. Muscle function on both sides of the face was evaluated by electromyography, using bipolar surface electrodes. The right temporalis showed greater activity than the left, both at rest and in function. In addition, the right masseter showed slightly greater activity than the left in function (clenching).
Based on the clinical and radiographic analysis, we concluded that the maxilla was deficient on the right side, in the sagittal dimension as well as in the vertical plane. Mandibular dimensions were within normal limits in the sagittal plane, despite the Tc scan indication of a hyperactive condyle on the left side. This finding was reaffirmed by an optimal 12.5% ratio of head size to total body height.10 The ramus was shorter on the right side, resulting in occlusal canting. Therefore, to correct the facial deformity in the vertical and sagittal dimensions, we would need to increase the mandibular ramal and body length and the vertical height of the maxilla on the right side, advance the maxilla, and restore the carious teeth. Conventional treatment of condylar hyperplasia would have called for a condylectomy and mandibular reduction surgery on the left side, but the patient’s facial height contraindicated such reduction.
Leveling and alignment were carried out for four months using .022" MBT* appliances, until an .019" × .025" stainless steel archwire could be placed (Fig. 3).
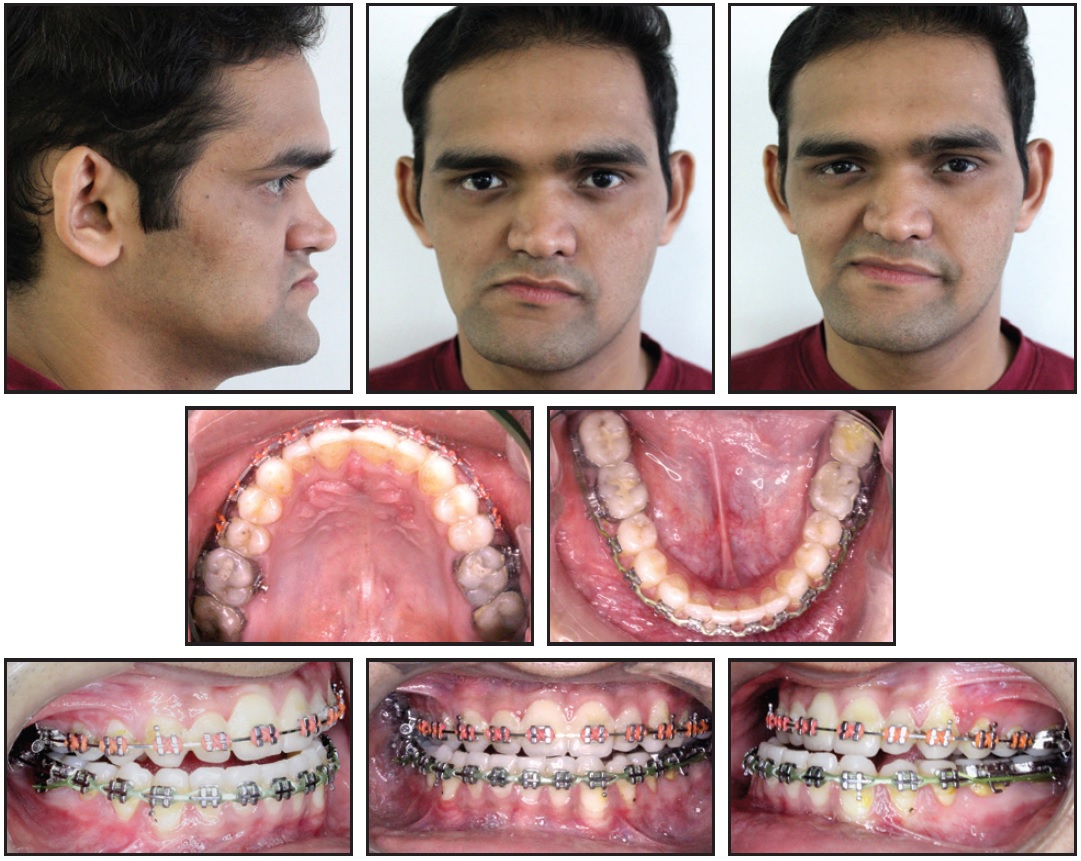
Fig. 3 After six months of treatment, prior to mandibular distraction.
After six months of treatment, an extraoral device was placed to correct the mandibular asymmetry by distraction of the right side (Fig. 4).
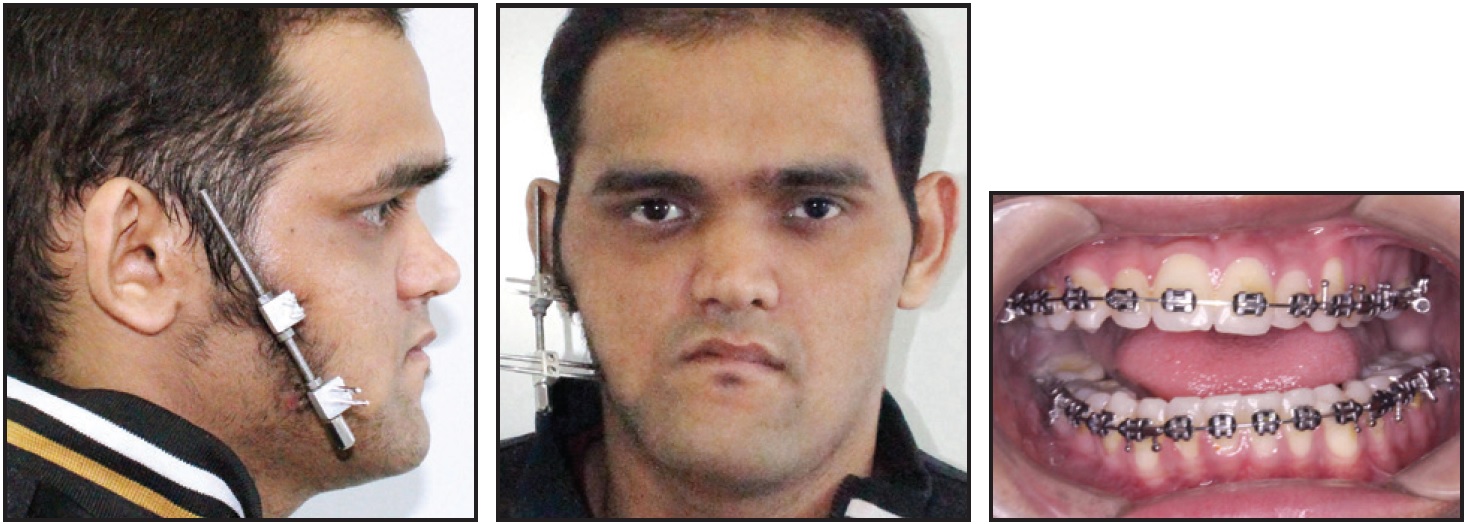
Fig. 4 After seven months of treatment, with mandibular distraction in progress.
An angular cut was made, and the distractor was placed obliquely to elongate the ramus and the mandibular body simultaneously. Distraction was carried out at the rate of one turn per day for eight days, until the chin point was centered. The distractor was kept in place for another two months to retain the correction.
Although this procedure corrected the canting of the mandibular occlusal plane, it created an 11mm open bite. To bring the posterior teeth into occlusion on the left side, we prescribed ³⁄16", 3.5oz intermaxillary elastics for two months (Fig. 5).
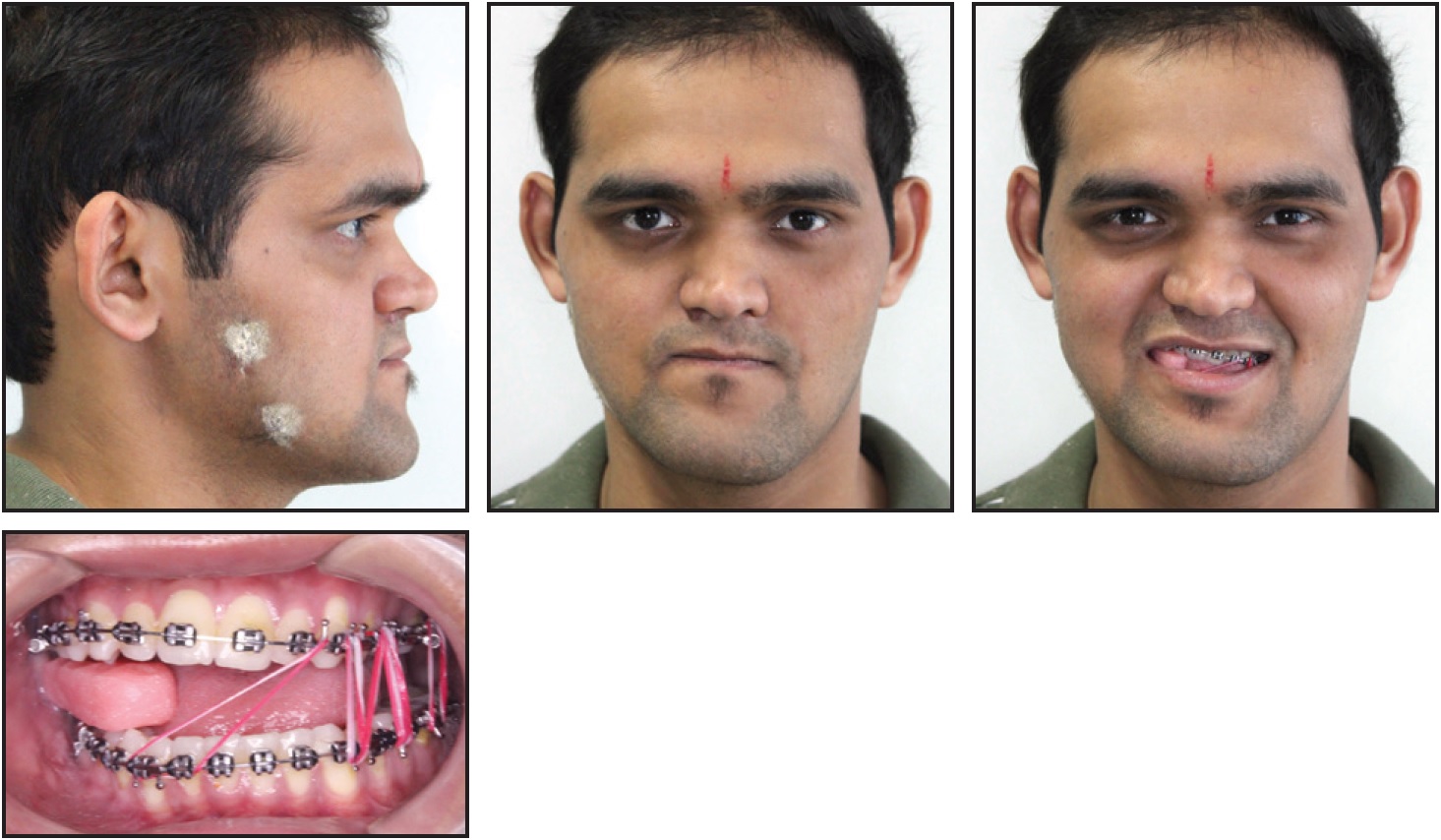
Fig. 5 After eight and a half months of treatment, with mandibular distraction complete, intermaxillary elastics used to close 11mm open bite; bite block worn on right side to maintain interocclusal gap and allow for eventual vertical correction of maxilla.
An intermaxillary elastic was worn across the midline from the upper left canine to the lower right canine to maintain a retentive force toward the distracted side.
At that point, panoramic and PA cephalograms clearly showed the leveled lower occlusal plane with marked deviation of the maxillary occlusal plane, which was canted upward on the right (Fig. 6).
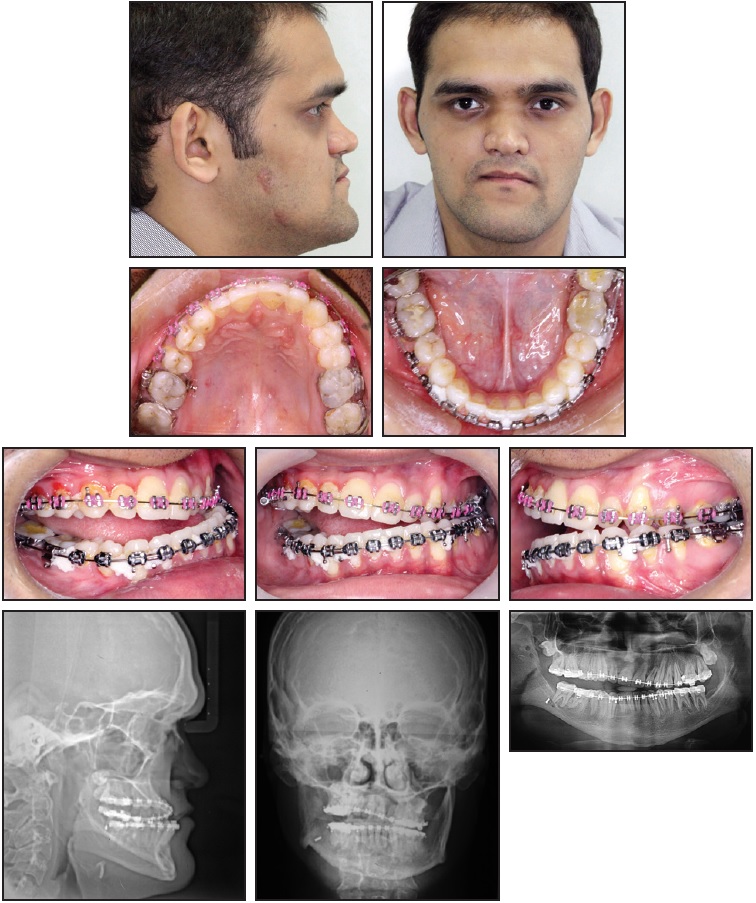
Fig. 6 After 12 months of treatment, lower occlusal plane leveled and maxillary occlusal plane canted upward on right side.
To allow for eventual vertical correction of the maxilla, the interocclusal gap on the right side had been maintained with an acrylic occlusal bite block. A facebow transfer was taken to record the maxillary occlusal plane with respect to the cranium, since the maxilla required correction in both the sagittal and vertical directions. After the models were articulated, a mock surgery was performed to visualize the required amount of correction. A Le Fort I osteotomy was then performed to advance the maxilla by 7mm, along with a genioplasty to correct the chin asymmetry. An intraoral distractor was placed by means of a midpalatal split to elongate the maxilla on the right side, thus correcting the maxillary cant and closing the interocclusal gap (Fig. 7). The upper archwire was cut at the midline to allow vertical descent of the maxilla on the right side (Fig. 8).

Fig. 7 After 14 months of treatment, with vertical maxillary distraction in progress.

Fig. 8 After 15 months of treatment, with vertical maxillary distraction complete.
The distraction achieved 7mm of vertical movement of the right maxilla, and the posterior occlusion was settled within one month. The sectional wire was then removed, and an upper .017" × .025" nickel titanium archwire was placed. Class III elastics were worn for nine months to maintain the positive overjet.
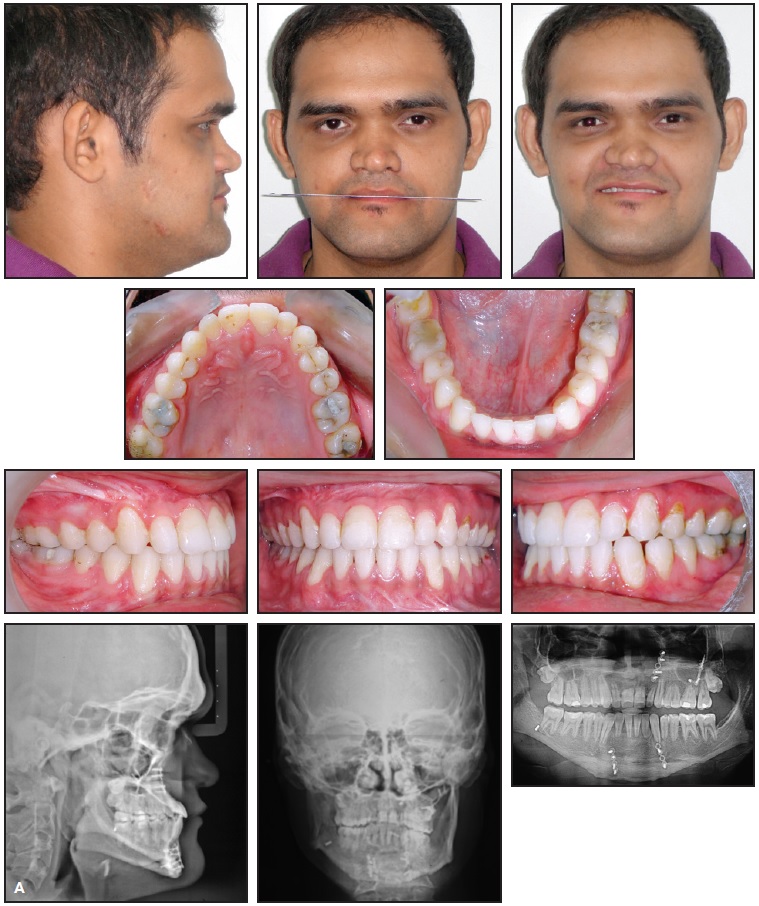
Fig. 9 A. Patient after 24 months of treatment (continued in next image).

Fig. 9 (cont.) B. Superimposition of pre- and post-treatment cephalometric tracings.
Post-treatment photographs showed marked improvement in the canting of the oral rim, with a centered chin. An esthetic profile and excellent occlusion were achieved. Post-treatment radiographs showed that the difference in mandibular body length on the right and left sides was reduced from 9mm to 3mm. Menton shifted 6mm to the left and was centered on the MSR.
Two-year follow-up found a stable occlusion and facial symmetry. A repeat Tc 99m scan showed negligible focal spots at the left condyle, indicating cessation of growth at this previously active site (Fig. 10).
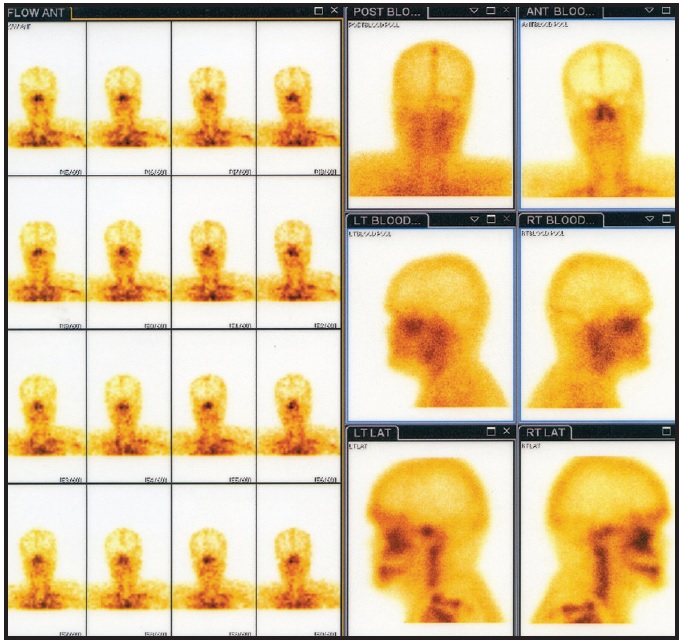
Fig. 10 Technetium 99m scan two years after treatment.
Discussion
Although facial asymmetry often presents subclinically,11,12 significant facial disproportions can lead to both esthetic and functional issues.13,14 An appropriate treatment plan requires careful investigation of the etiology of asymmetry. The exact pathogenesis of condylar hyperplasia is still unclear, but possible causes include trauma followed by excessive proliferation in the repair process, genetic factors, increased functional loading of the TMJ, hormonal influences, arthrosis, infection, and hypervascularity.15 The patient shown here had a history of a fall during childhood.16
Successful management of condylar hyperplasia depends largely on a correct diagnosis.17 Nuclear imaging is an important diagnostic adjunct, providing physiological details by means of radionuclide-labeled tracers. In the present case, SPECT images reconstructed from a Tc 99m scan showed increased uptake in the left condyle, indicating condylar hyperplasia. Our clinical findings of a vertical enlargement of the mandible and horizontal displacement of the chin to the right could be categorized as Obwegeser and Makek type 35 or Wolford type 1B condylar hyperplasia.6
Condylar hyperplasia is commonly treated by reduction of the apparently enlarged side, but our patient had normal mandibular dimensions and a nearly ideal 12.5% ratio of head size to total body height,15 presenting a true diagnostic and treatment-planning challenge. Since a reduction of mandibular length was not indicated, the right facial dimensions had to be increased to correct the facial asymmetry. Saridin and colleagues have pointed out that condylar hyperplasia can also be caused by reduced growth of the contralateral condyle compared with the affected condyle, as indicated by oxygen-15-labeled water and fluoride-18-labeled positron emission tomography imaging.18 In our patient, the fluoride uptake was significantly higher in the affected condyle, indicating a cessation of growth in the contralateral condyle and weighing against condylectomy in this case. Because the active condyle in a case of condylar hyperplasia ceases to grow between ages 18 and 25,7 the growth status of the functioning condyle must be kept under observation. A repeat Tc scan was performed to assess the need for condylectomy when the patient approached age 25.
Management of condylar hyperplasia depends on the patient’s growth status and deformity.19 In this case, based on clinical evaluation and cephalometric findings, we decided to correct the skeletal deficiency first by means of distraction and orthognathic surgery, avoiding the need for later condylectomy. The results were satisfactory and stable.
FOOTNOTES
- *Trademark of 3M, Monrovia, CA; www.3M.com.
REFERENCES
- 1. Hegtvedt, A.K.: Diagnosis and management of facial asymmetry, in Principles of Oral and Maxillofacial Surgery, vol. 3, ed. L.J. Peterson, A.T. Indressano, R.D. Marciani, and S.M. Roser, Lippincott Williams & Wilkins, Philadelphia, 1992, pp. 1400-1414.
- 2. Cohen, M.M. Jr.: Perspectives of craniofacial asymmetry, Part III: Common and/or well known causes of asymmetry, Int. J. Oral Maxillofac. Surg. 24:127-133, 1995.
- 3. Reyneke, J.P.; Tsakiris, P.; and Kienle, F.: A simple classification for surgical planning of maxillomandibular asymmetry, Br. J. Oral Maxillofac. Surg. 35:349-351, 1997.
- 4. Olate, S.; Netto, H.D.; Rodriguez-Chessa, J.; Alister, J.P.; de Albergaria-Barbosa, J.; and Moraes, M.: Mandible condylar hyperplasia: A review of diagnosis and treatment protocol, Int. J. Clin. Exp. Med. 6:727-737, 2013.
- 5. Obwegeser, H.L. and Makek, M.S.: Hemimandibular hyperplasia—Hemimandibular elongation, J. Maxillofac. Surg. 14:183-208, 1986.
- 6. Wolford, L.M.; Movahed, R; and Perez, D.E.: A classification system for conditions causing condylar hyperplasia, J. Oral Maxillofac. Surg. 72:567-595, 2014.
- 7. Blasberg, B. and Greenberg, M.S.: Temporomandibular disorders, in Burket’s Oral Medicine, 11th ed., ed. M.S. Greenberg, M. Glick, and J.A. Ship, B.C. Decker Inc., Hamilton, Ontario, 2008.
- 8. Singh, V.; Verma, A.; Attresh, G.; and Batra, J.: Ortho-surgical management of condylar hyperplasia: Rare case reports, Natl. J. Maxillofac. Surg. 5:54-59, 2014.
- 9. Jones, R.H. and Tier, G.A.: Correction of facial asymmetry as a result of unilateral condylar hyperplasia, J. Oral Maxillofac. Surg. 70:1413-1425, 2012.
- 10. Boyd, E.: Outline of Physical Growth and Development, Burgess Publishing Co., Minneapolis, 1941.
- 11. McCoy, J.D.: Applied Orthodontia, 3rd ed., Lea & Febiger, Philadelphia, 1931, p. 49.
- 12. Proffit, W.R. and Turvey, T.A.: Dentofacial asymmetry, in Contemporary Treatment of Dentofacial Deformity, ed. W.R. Proffit, R.P. White, and D.M. Sarver, Mosby, St. Louis, 2003, pp. 574-644.
- 13. Severt, T.R. and Proffit, W.R: The prevalence of facial asymmetry in the dentofacial deformities population at the University of North Carolina, Int. J. Adult Orthod. Orthog. Surg. 12:171-176, 1997.
- 14. Bishara, S.E.; Burkey, P.S.; and Kharouf, J.G.: Dental and facial asymmetries: A review, Angle Orthod. 64:89-98, 1994.
- 15. Ahn, S.J.; Lee, S.P.; and Nahm, D.S.: Relationship between temporomandibular joint internal derangement and facial asymmetry in women, Am. J. Orthod. 128:583-591, 2005.
- 16. Nitzan, D.W.; Katsnelson, A.; Bermanis, I.; Brin, I.; and Casap, N.: The clinical characteristics of condylar hyperplasia: Experience with 61 patients, J. Oral Maxillofac. Surg. 66:312-318, 2008.
- 17. Mehrotra, D.; Dhasmana, S.; Kamboj, M.; and Gambhir, G.: Condylar hyperplasia and facial asymmetry: Report of five cases, J. Maxillofac. Oral Surg. 10:50-56, 2011.
- 18. Saridin, C.P.; Raijmakers, P.G.; Kloet, R.W.; Tuinzing, D.B.; Becking, A.G.; and Lammertsma, A.A.: No signs of metabolic hyperactivity in patients with unilateral condylar hyperactivity: An in vivo positron emission tomography study, J. Oral Maxillofac. Surg. 67:576-581, 2009.
- 19. Xavier, S.P.; de Santana Santos, T.; Silva, E.R.; Faria, A.C.; and de Mello Filho, F.V.: Two-stage treatment of facial asymmetry caused by unilateral condylar hyperplasia, Braz. Dent. J. 25:257-260, 2014.







COMMENTS
.