Correction of Maxillary Transverse Deficiency in Growing Patients with Permanent Dentitions
Maxillary transverse deficiency (MTD) often manifests as dental crossbite with the upper teeth positioned lingual to the lower teeth in centric occlusion.1 Posterior crossbite is found in 7.7% of patients in the deciduous or mixed dentition, but its incidence increases into adulthood.2,3 Posterior crossbite is more prevalent in Caucasian than in Mexican-American, Asian, or African American populations.3,4 The etiology is multifactorial, involving congenital, developmental, traumatic, and iatrogenic factors.5 Patients with cleft-palate repair or with mouthbreathing, sucking, or tongue habits are particularly at risk.4
Patients with MTD can exhibit unilateral or bilateral posterior crossbites, often accompanied by anterior dental crowding.6 Crossbite-induced occlusal interferences may force a patient to functionally shift the mandible to one side to establish a more stable occlusion, leading to mandibular midline deviations and facial asymmetries.7,8 A unilateral crossbite is typically attributable to a bilateral constriction of the maxilla and a resultant functional shift.2,7
Similar articles from the archive:
Because a crossbite does not self-correct, treatment should be aimed at increasing the width of the maxillary arch.9 The goal is to eliminate any undesirable alteration of the TMJ complex and thus allow normal mandibular closure without deviations.10-12 If the crossbite is left untreated, resulting muscle and TMJ strain can lead to skeletal facial asymmetries requiring surgical correction in adulthood.13
Traditional rapid maxillary expanders introduce heavy intermittent forces; Isaacson reported three to 10 pounds of force from a single activation of an expansion screw.14 Immediate decay results in a loss of about two pounds of force after activation, but the decay rate rapidly declines within minutes and a constant force remains. A cumulative effect is observed with further activations, so that the total force can reach 22 pounds by the end of a typical expansion protocol. In younger patients, because of the immaturity of the midpalatal suture, lower forces are observed per activation.14
Slow maxillary expansion appliances typically deliver lower continuous forces of around two pounds.15 Most devices that utilize springs to generate the expansion forces provide continuous force application and do not require patient compliance. One drawback of this concept, however, is that the force delivered by the expander is inversely proportional to the amount of expansion.16 As expansion occurs, the springs become decompressed and lose much of their ability to apply force. Another disadvantage is that the appliance may not provide enough force to disrupt the midpalatal suture in a more mature patient.17
Several nickel titanium expanders have been introduced to provide low levels of continuous force application. The Arndt expander delivers 230-300g of continuous force upon insertion.18 Corbett’s Nitanium Palatal Expander(2)* appliance delivers 350g of force.19 The Memory Palatal Split Screw** is reported to produce as much as 1,700g of force after the first six activations and then to maintain an average force level between 1,225g and 1,425g upon further activation.20
Memoria Leaf Spring Activated Expander
Gianolio and colleagues introduced the nickel titanium Memoria Leaf Spring Activated Expander*** in 2015.21 Activation of the traditional expansion screw compresses the nickel titanium leaf springs, which then apply a constant expansion force as they regain their original shapes. This expander is available in a light (500g) or medium (800g) version—each in a 6mm size, with two leaf springs that can be activated as many as 35 times, or a 10mm size, with three leaf springs that can be activated as many as 50 times.
Unlike conventional two-screw devices, this expander uses a single screw that is only .4mm in circumference. The components of the expander are housed in an expansion screw body measuring 11mm × 12mm × 4mm. Upon delivery from the laboratory, the expander is preactivated with fully compressed leaf springs held together by a steel ligature. After cementation, the ligature is cut and no further activation is required. No patient instruction is needed, because the screw is activated eight to 10 times at each monthly appointment until adequate expansion is obtained. Recompressing the leaf springs produces a continuous expansion force as they regain their original shape. Normally, each activation provides about .1mm of expansion. Once the transverse dimension is correct, it is important to stabilize the expansion screw, since there may be residual activation in the leaf springs.21
Benchmark studies were conducted by the manufacturer on each variant of the expander to determine the forces applied by the nickel titanium leaf springs.22 In the 800g version, the fully decompressed leaf springs measure about 3.5mm in width. Upon compression, the load increases in a logarithmic fashion until a force of about 800g is reached. This load is present from 1mm compression up to full compression of the leaf coils, suggesting that a constant force of 800g is introduced by the expansion screw when it is compressed by more than 1mm. A similar pattern is found with the 500g version: following full compression of the leaf springs, the compression load forces spike as the screw contacts the body of the screw housing. When the coils are fully compressed, the screw functions as a traditional expansion screw, delivering heavy intermittent forces to the dentoskeletal structures.
Lanteri and colleagues reported using the 6mm Memoria Leaf Spring Activated Expander in two mixed dentition cases, banding the maxillary primary molars and allowing spontaneous derotation and expansion of the maxillary first molars.23 Each patient received 10 activations per month. Active expansion typically lasted six months and was followed by a three-month passive retention phase. Archform, crossbite, midline deviation, and permanent molar rotation and expansion all improved and remained stable nine months after expansion. Average increases in arch width of 6.3mm, 5.9mm, 5.9mm, and 3.8mm were observed in the canine, first primary molar, second primary molar, and first permanent molar regions, respectively.
This article describes the correction of MTD following the standardized protocol proposed by Lanteri and colleagues.23 Digital models made before and after expansion were used to evaluate the effectiveness of the expander.
Case 1
A 13-year-old female presented with the chief complaint of crowded teeth and a lower molar that was “growing in wrong.” She had a straight profile, with a prominent chin and an obtuse nasolabial angle, and she exhibited 90% incisal display on smiling and a normal lower anterior facial height. Further clinical examination showed a Class III subdivision right malocclusion, with MTD leading to constricted maxillary buccal segments (Fig. 1).

Fig. 1 Case 1. 13-year-old female patient with maxillary transverse deficiency, Class III malocclusion, and mandibular deviation before treatment.
The mandibular midline was shifted 2.5mm to the left because of a functional shift of the mandible on closure. An anterior open bite was present in the maxillary right lateral and canine regions. Both mandibular second molars were erupting at a mesial angle.
The panoramic radiograph revealed a root dilaceration of the upper right lateral incisor, normal TMJ anatomy, and no third molar buds. Cephalometric analysis indicated a Class III skeletal pattern with a prognathic mandible, a normal vertical growth pattern, and retroclined mandibular incisors. Cervical vertebral maturation was at stage 4.24 A frontal cephalometric finding of facial asymmetry supported the diagnosis of a functional shift.
Treatment objectives were to maintain the facial profile, correct the transverse discrepancy, upright the lower second molars, achieve Class I molar and canine relationships with ideal overbite and overjet, and resolve the midline deviation. Potential treatment plans included maxillary expansion with a Hyrax† expander and Class III dental correction using intermaxillary elastics. The parents were also given the option to resolve the transverse discrepancy and then delay further treatment until growth was complete. They were warned that if future growth was not favorable, surgical intervention might be required to resolve the skeletal discrepancy. The parents chose to proceed with immediate treatment, and we devised a plan utilizing the nickel titanium Memoria Leaf Spring Activated Expander to correct the transverse deficiency, followed by the DynaFlex CS2000‡ system to correct the dental Class III malocclusion. This would produce a symmetrical Class I buccal occlusion with coincident midlines and also eliminate the transverse discrepancy.
A nickel titanium Memoria Leaf Spring Activated Expander was placed and then reactivated 10 times at each monthly appointment until the correction was completed, in about two and a half months (Fig. 2).
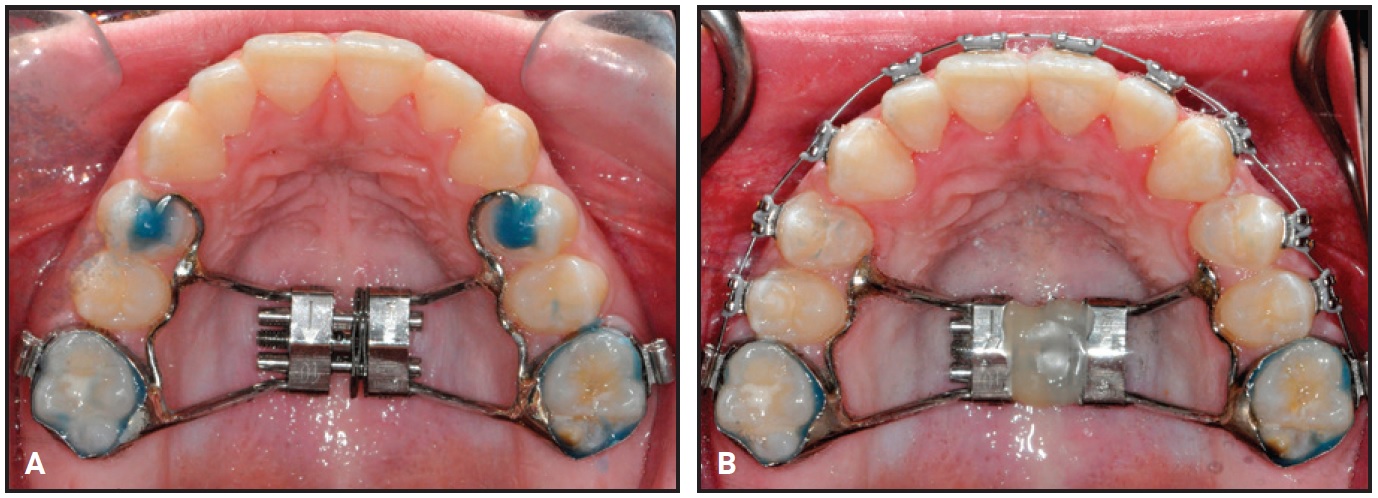
Fig. 2 Case 1. A. Memoria Leaf Spring Activated Expander*** cemented in place. B. After two and a half months of expansion, expansion screw stabilized with flowable composite.
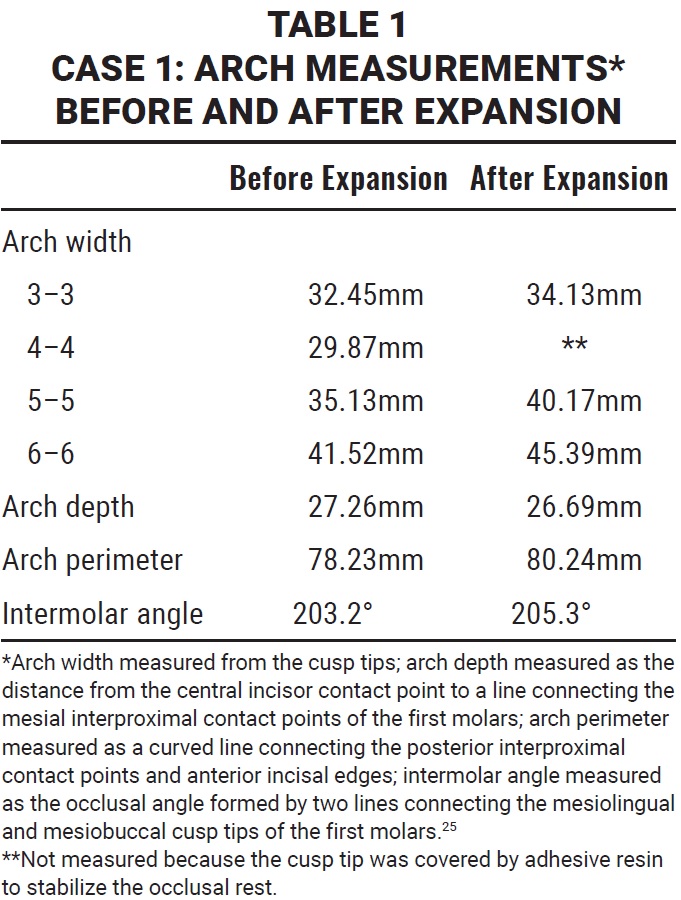
After intermolar expansion of 3.87mm had been obtained (Fig. 3, Table 1), flowable composite was placed in the expansion screw housing to stabilize the appliance. A maxillary impression was then obtained and digitized to evaluate the molar angulation changes (Fig. 4). Bony separation suggesting mild sutural disruption was indicated by radiolucency on the occlusal radiograph (Fig. 5).
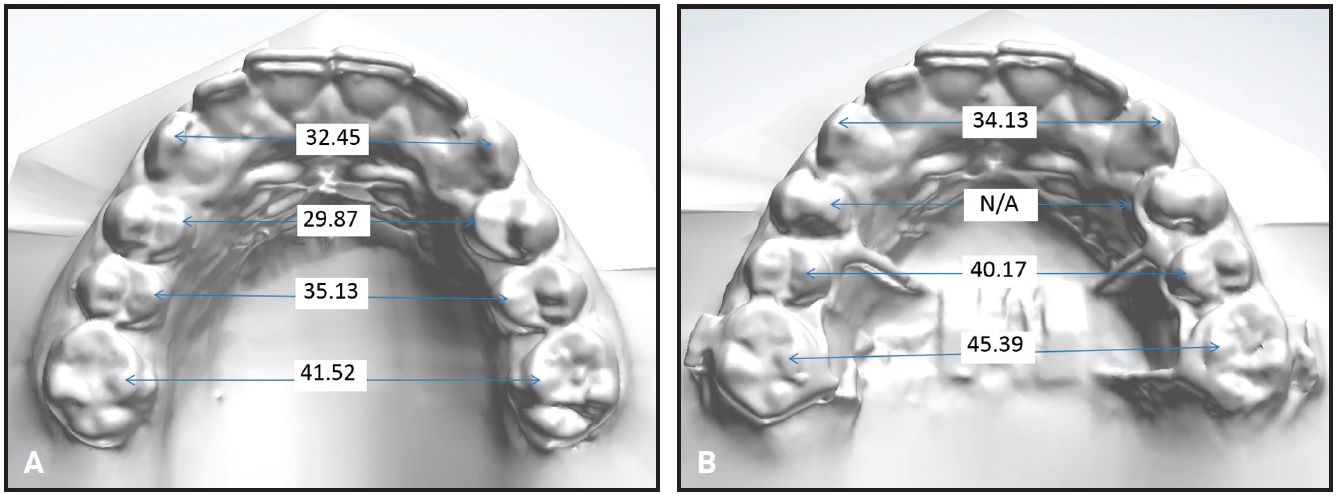
Fig. 3 Case 1. Maxillary dental arch-width measurements (mm) before (A) and after (B) expansion.
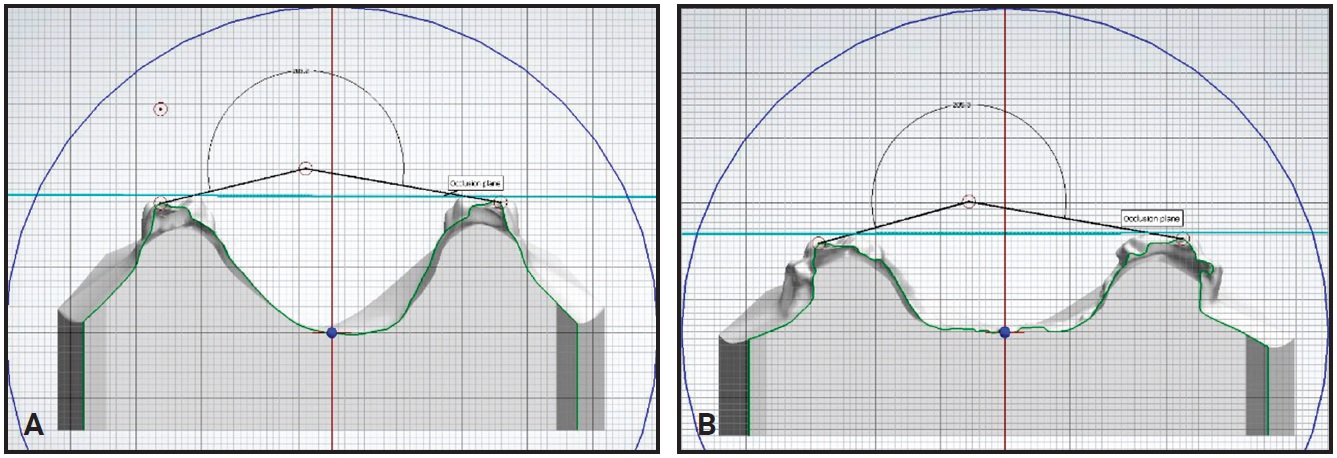
Fig. 4 Case 1. Molar angulation before (A) and after (B) expansion.
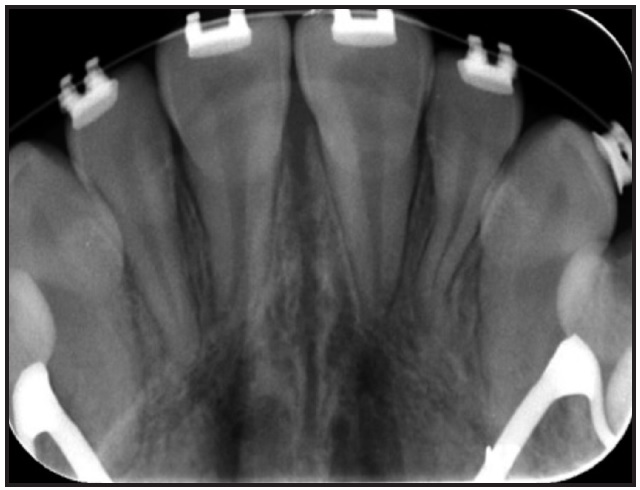
Fig. 5 Case 1. Occlusal radiograph indicating mild sutural disruption after expansion.
During three months of passive maintenance of the expansion, lower segmental .016" × .022" nickel titanium archwires were used in .018" brackets. The remaining teeth were then bonded, and leveling and alignment were accomplished with .014" cobalt nickel titanium, .016" nickel titanium, and .016" × .022" stainless steel archwires. Once the final wires were inserted in both arches, the DynaFlex CS2000 system was placed, with the housing nuts allowed to slide passively on the archwires. The Class III malocclusion and dental midline discrepancy were almost completely corrected in one month; detailing movements were carried out using conventional interarch elastics. Upper and lower wraparound Hawley retainers were delivered for six months of full-time wear, followed by nighttime wear indefinitely.
Case 2
A 12-year-old female presented with the chief complaint that “my tooth is coming in a little high.” She had a straight profile with an obtuse mentolabial sulcus, symmetrical face, and thin lips, but she appeared tired because of dark infraorbital circles. The patient showed 100% incisal display on smiling, with 2.5mm of gingival display and wide buccal corridors. We noted a Class I molar relationship, moderate crowding in both arches, and a Class III skeletal relationship due to a prognathic mandible and a slightly low mandibular plane angle (Fig. 6). The patient had a 50% overbite, along with a 2mm maxillary anterior Bolton deficiency. There was inadequate space for the upper canines, which were beginning to erupt. The angulation of the canines was appropriate, however, and no resorption of the lateral incisors was observed.

Fig. 6 Case 2. 12-year-old female patient with Class III skeletal and Class I molar relationships, 50% overbite, and moderate crowding in both arches.
Panoramic radiography revealed enlarged nasal turbinates; all permanent teeth were present, and the third molar buds were developing. Cephalometric analysis indicated retroclined mandibular incisors, slightly proclined maxillary incisors, and a cervical vertebral maturation stage 2.24
The objectives of treatment were to evaluate the airway, expand the upper arch to provide room for the canines to erupt, alleviate the crowding, maintain the Class I molar and canine relationships, and correct the deep bite. Alternatives for maxillary expansion included Quad-Helix,†† Haas, or Hyrax expanders; in addition, expanded upper and lower archwires with open-coil springs could have achieved adequate results. Because of the wide buccal corridors, however, we believed that an auxiliary expansion device was needed. A treatment plan was formulated utilizing the nickel titanium Memoria Leaf Spring Activated Expander to expand the maxillary arch, followed by a three-month passive retention phase. Airway evaluation by an otolaryngologist was recommended. Expanded archwires were planned to upright the mandibular buccal segments. The lower incisors would be flared to alleviate the crowding, and the canines would be brought into the arch once sufficient space was obtained. The need for a facemask or Class III elastics would be evaluated during treatment. The patient and parents were told that future Class III growth might occur, and that further treatment could be required if such unfavorable changes occurred.
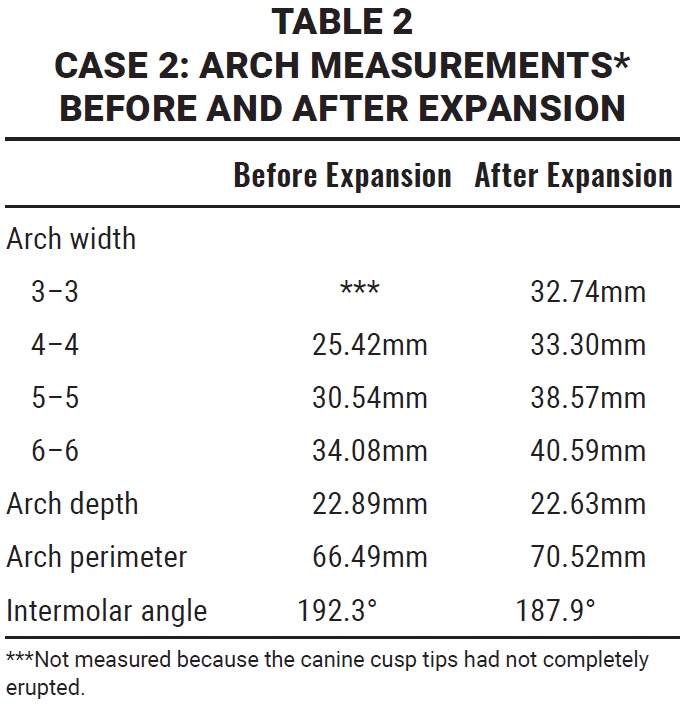
A nickel titanium Memoria Leaf Spring Activated Expander was placed (Fig. 7) and activated 10 times at each monthly appointment for six months, until about 6.5mm of intermolar expansion had been obtained (Fig. 8, Table 2). The expander was then made passive by adding flowable composite to stabilize the springs. A maxillary impression was taken and digitized to evaluate the molar angulation changes (Fig. 9). The occlusal radiograph revealed no noticeable sutural disruption (Fig. 10).
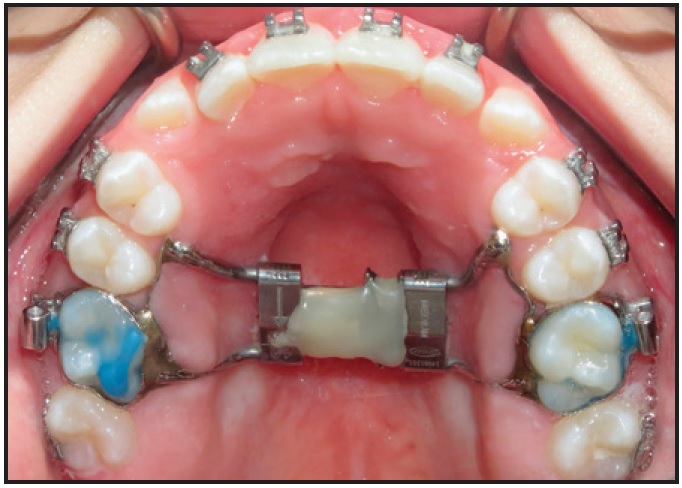
Fig. 7 Case 2. After about six months of expansion, expander stabilized with flowable composite.
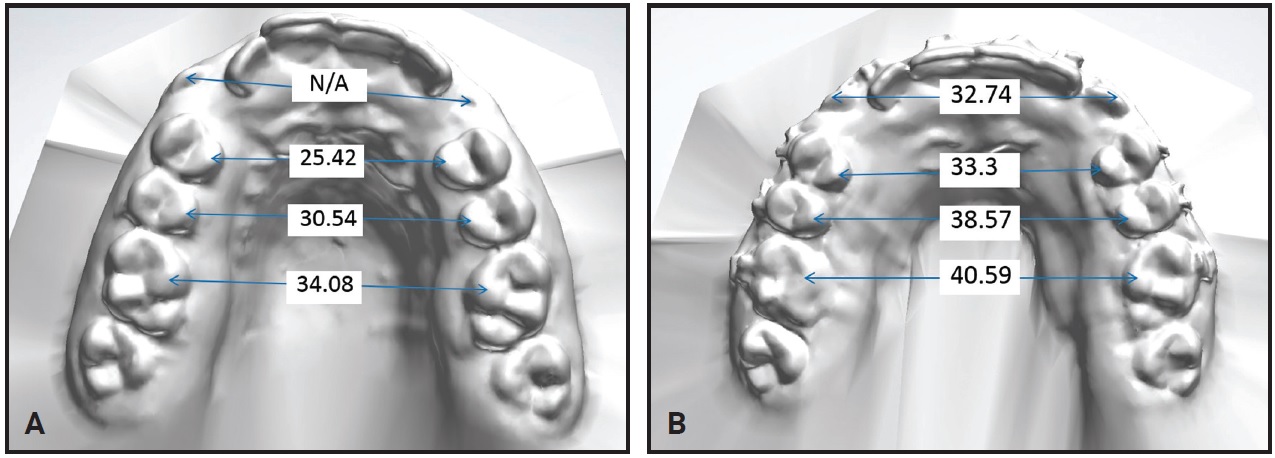
Fig. 8 Case 2. Maxillary dental arch-width measurements (mm) before (A) and after (B) expansion.
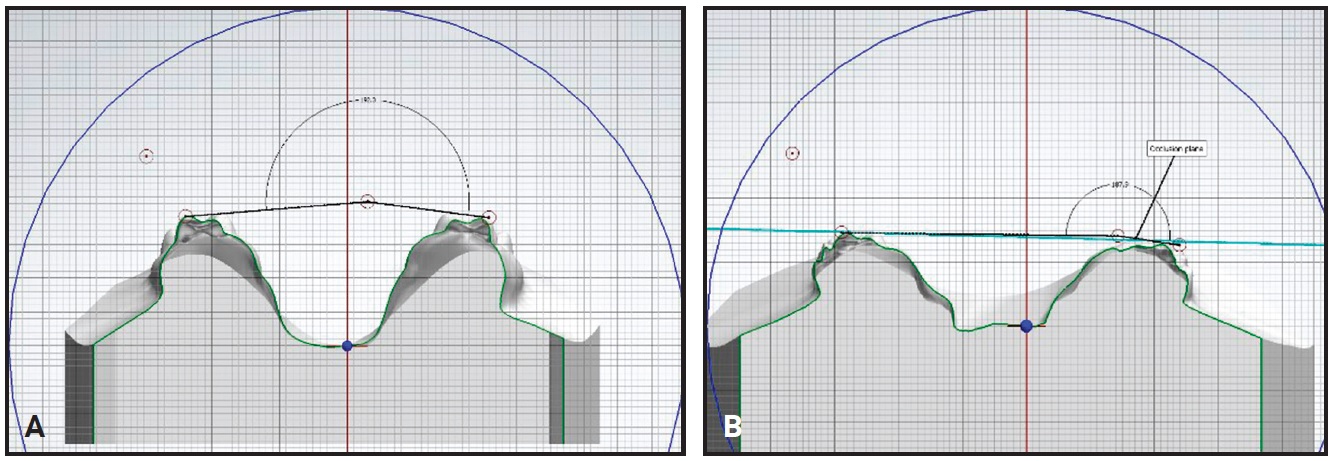
Fig. 9 Case 2. Molar angulation before (A) and after (B) expansion.
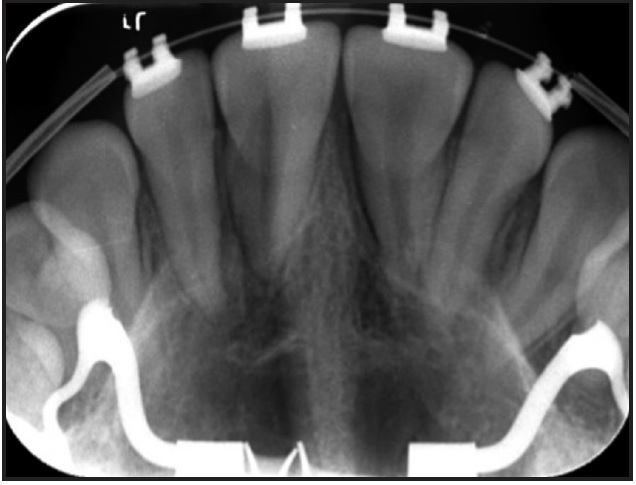
Fig. 10 Case 2. Occlusal radiograph showing no noticeable sutural disruption after expansion.
The expander was kept in place for another three months to prevent relapse. During the expansion phase, .014" cobalt nickel titanium and .016" nickel titanium archwires were used to level and align the lower arch. One month prior to stabilizing the expansion screw, an .014" nickel titanium upper archwire was placed. During the passive maintenance phase, .016" × .022" nickel titanium archwires were followed by .016" × .022" stainless steel archwires. Conventional interarch and finishing elastics were used to correct the remaining minor sagittal and transverse discrepancies. A fixed lower 3-3 retainer was bonded, and an upper wraparound Hawley retainer was prescribed to be worn full-time for six months, then at night indefinitely.
Discussion
Although few clinicians in the United States have implemented the Memoria Leaf Spring Activated Expander into routine clinical care at this point, orthodontic laboratories have informed us that the total cost of the system ranges from $105 to $120. The expansion screw itself costs $40-55. Although this appliance is therefore more costly than traditional rapid palatal expanders ($80-88) or Quad-Helix devices ($52-67), it requires no patient compliance and can be activated intraorally using a standardized protocol. Unlike a Quad-Helix, it does not need to be removed for reactivation, and a more calibrated amount of expansion can be achieved.
Clinical experience has demonstrated that the Memoria Leaf Springs are capable of producing slow intermolar expansion in the permanent dentition when the proper design and procedures are used. We recommend banding the maxillary first molars and bonding mesial extension arms to the first premolars for anchorage. Because the protocol of 10 turns per monthly visit often leads to lengthy active expansion periods, however, further investigation is needed to determine whether increasing the number of monthly activations might increase the applied force and reduce the time needed for expansion. It should be noted that the springs apply the greatest amount of force when they are within a millimeter of full compression. This suggests that if 10 activations are performed when the leaves are fully decompressed, the amount of force being delivered will likely be far lower than the maximum. A revised protocol with biweekly activation visits could ensure that the optimal force is being delivered more continuously, potentially shortening the period of active expansion.
Since the leaf springs come fully compressed from the lab, the preactivation should theoretically result in roughly 4mm of expansion as the springs decompress over time. The force expressed by the leaf springs diminishes after 2mm of decompression, however, so that in our experience, a clinician can assume that only half of this preactivation will be expressed. If 1mm of expansion can be obtained for every 10 activations of the expansion screw, as confirmed by the two cases shown here, another 2mm should be added to the total to account for preactivation of the appliance.
FOOTNOTES
- *Henry Schein Orthodontics, Melville, NY; www.henryschein.com.
- **Forestadent GmbH, Pforzheim, Germany; www.forestadent.com.
- ***Registered trademark of American Tooth Industries, Oxnard, CA; www.americantooth.com.
- †Registered trademark of Dentaurum, Inc., Newtown, PA; www.dentaurum.com.
- ‡Trademark of DynaFlex, St. Ann, MO; www.dynaflex.com.
- ††Rocky Mountain Orthodontics, Denver, CO; www.rmortho.com.
REFERENCES
- 1. Zegan, G.; Dascalu, C.G.; Mavru, R.B.; and Golovcencu, L.: Risk factors and predictors of crossbite at children, Rev. Med. Chir. Soc. Med. Nat. Iasi. 119:564-571, 2015.
- 2. Kutin, G. and Hawes, R.R.: Posterior cross-bites in the deciduous and mixed dentitions, Am. J. Orthod. 56:491-504, 1969.
- 3. Brunelle, J.A.; Bhat, M.; and Lipton, J.A.: Prevalence and distribution of selected occlusal characteristics in the U.S. population, 1988-1991, J. Dent. Res. 75:706-713, 1996.
- 4. Malandris, M. and Mahoney, E.K.: Aetiology, diagnosis and treatment of posterior cross-bites in the primary dentition, Int. J. Paediat. Dent. 14:155-166, 2004.
- 5. Betts, N.J.; Vanarsdall, R.L.; Barber, H.D.; Higgins-Barber, K.; and Fonseca, R.J.: Diagnosis and treatment of transverse maxillary deficiency, Int. J. Adult Orthod. Orthog. Surg. 10:75-96, 1995.
- 6. Ramires, T.; Maia, R.A.; and Barone, J.R.: Nasal cavity changes and the respiratory standard after maxillary expansion, Braz. J. Otorhinolaryngol. 74:763-769, 2008.
- 7. Higley, L.B.: Crossbite—mandibular malposition, ASDC J. Dent. Child. 35:221-223, 1968.
- 8. Lewis, P.D.: The deviated midline, Am. J. Orthod. 70:601-616, 1976.
- 9. Da Silva Filho, O.G.; Valladares Neto, J.; and Rodrigues de Almeida, R.: Early correction of posterior crossbite: Biomechanical characteristics of the appliances, J. Pedod. 13:195-221, 1989.
- 10. Myers, D.R.; Barenie, J.T.; Bell, R.A.; and Williamson, E.H.: Condylar position in children with functional posterior crossbites: Before and after crossbite correction, Pediat. Dent. 190-194, 1980.
- 11. Barner, R.E.: The early expansion of deciduous arches and its effect on the developing permanent dentition, Am. J. Orthod. 42:83-97, 1956.
- 12. Harberson, V.A. and Myers, D.R.: Midpalatal suture opening during functional posterior cross-bite correction, Am. J. Orthod. 74:310-313, 1978.
- 13. Agostino, P.; Ugolini, A.; Signori, A.; Silvestrini-Biavati, A.; Harrison, J.E.; and Riley, P.: Orthodontic treatment for posterior crossbites, Cochrane Database Syst. Rev. CD000979, 2014.
- 14. Isaacson, R.J. and Ingram, A.H.: Forces produced by rapid maxillary expansion, Part II: Forces present during treatment, Angle Orthod. 34:261-270, 1964.
- 15. Hicks, E.P.: Slow maxillary expansion: A clinical study of the skeletal versus dental response to low-magnitude force, Am. J. Orthod. 73:121-141, 1978.
- 16. Romanyk, D.L.; Lagravere, M.O.; Toogood, R.W.; Major, P.W.; and Carey, J.P.: Review of maxillary expansion appliance activation methods: Engineering and clinical perspectives, J. Dent. Biomech. 2010:496906, 2010.
- 17. Storey, E.: Tissue response to the movement of bones, Am. J. Orthod. 64:229-247, 1973.
- 18. Arndt, W.V.: Nickel titanium palatal expander, J. Clin. Orthod. 27:129-137, 1993.
- 19. Corbett, M.C.: Slow and continuous maxillary expansion, molar rotation, and molar distalization, J. Clin. Orthod. 31:253-263, 1997.
- 20. Wichelhaus, A.; Geserick, M.; and Ball, J.: A new nickel titanium rapid maxillary expansion screw, J. Clin. Orthod. 38:677-680, 2004.
- 21. Gianolio, A.; Lanteri, C.; Lanteri, V.; and Cherchi, C.: A new device for calibrated maxillary expansion: The nickel titanium Memoria Leaf Spring Activated Expander, OrthoNews 38:1, 2015.
- 22. Scommegna, G., Research and Development Director, Leone SpA, Florence, Italy: Personal communication, Oct. 26, 2016.
- 23. Lanteri, C.; Beretta, M.; Lanteri, V.; Gianolio, A.; Cherchi, C.; and Franchi, L.: The Leaf Expander for patients in the mixed dentition, J. Clin. Orthod. 50:552-560, 2016.
- 24. Baccetti, T.; Franchi, L.; and McNamara, J.A. Jr.: An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth, Angle Orthod. 72:316-323, 2002.
- 25. McNamara, J.A. Jr.; Baccetti, T.; Franchi, L.; and Herberger, T.A.: Rapid maxillary expansion followed by fixed appliances: A long-term evaluation of changes in arch dimensions, Angle Orthod. 73:344-353, 2003.





