Targeted Mechanics for Treatment of Patients with Severe Short-Root Anomaly
Short-root anomaly (SRA), which was first described by Lind in 1972,1 is characterized by abnormally short and plump roots.1,2 It is commonly misdiagnosed as root resorption, but is in fact a developmental defect with an unknown etiology. SRA affects mainly upper central incisors and premolars, but the entire permanent dentition can be affected in rare cases.3,4 A genetic component with an autosomal dominant inheritance pattern for SRA has been identified in several families affected by this condition.4,5
SRA has been related to other dental anomalies such as agenesis, invagination, supernumerary teeth, ectopic canines, and taurodontia.2,5 Disorders including type I dentin dysplasia6 and hypophosphatemia7 and syndromes such as Stevens-Johnson8 and Rothmund-Thomson9 have also been associated with the formation of short roots.
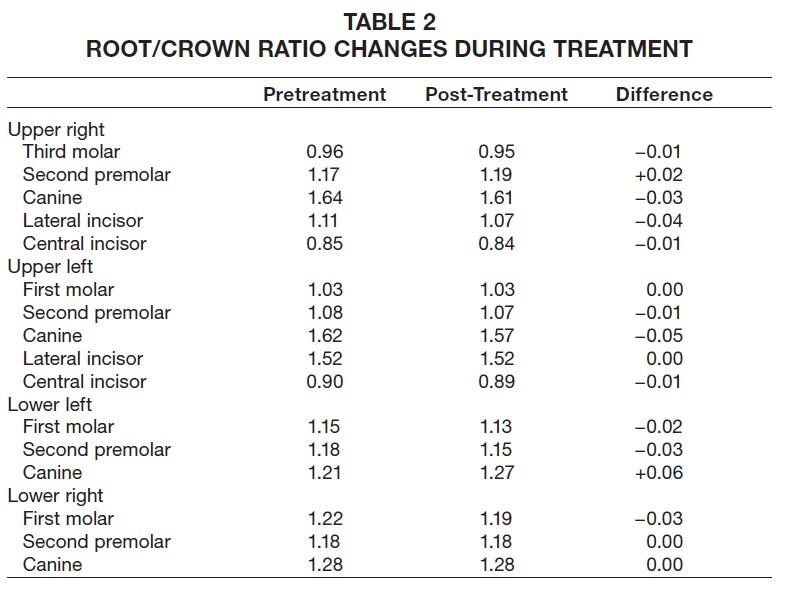
The average root/crown ratio is 1.6 for healthy teeth but only 1.1 for teeth affected with SRA.1 Generalized cases of SRA tend to exhibit even lower root/crown ratios than in localized cases.4 It has been suggested that SRA affects the dentition bilaterally, so that there is usually a symmetrical root/crown ratio between contralateral affected teeth.2,4,5 Although there are no long-term studies on the stability of the root/crown ratio in SRA patients, it does not seem to change substantially over time.4
The few published orthodontic case reports involving SRA suggest that with careful mechanics, treatment will produce little or no additional root shortening.5,10,11 Because root resorption may significantly worsen the prognosis of teeth with a reduced root/crown ratio, however, the consensus advice is to avoid orthodontic forces in patients with severe, generalized SRA.1,12
Similar articles from the archive:
Treatment Procedure
We recently proposed a “targeted mechanics” approach, in which the pretreatment buccal occlusion is maintained by avoiding movement of those teeth while correcting problems in the anterior segments by means of mini-implant anchorage.13 This technique was modified from a method described by Kim and colleagues, who proposed anterior retraction using mini-implant anchorage without involving the posterior teeth.14 After canine retraction, appliances are bonded to the rest of the dentition for final alignment and space closure. Under this approach, the teeth most commonly affected by SRA—the incisors and premolars—do not receive any orthodontic forces during the majority of treatment.
Case Report
A 17-year-old male presented to the orthodontic clinic at the University of Connecticut with the chief complaint of crooked teeth. Although the patient had not had any previous orthodontic treatment, he mentioned an earlier consultation with another orthodontist, who recommended no treatment due to the condition of the dental roots. The patient had a convex soft-tissue profile with protrusive lips, a Class I molar relationship, a 50% overbite, and a 7mm overjet (Fig. 1). There was 4mm of crowding in the maxillary arch and 8mm of crowding in the mandibular arch; the mandibular dental midline was deviated 3mm to the left in relation to the facial midline.
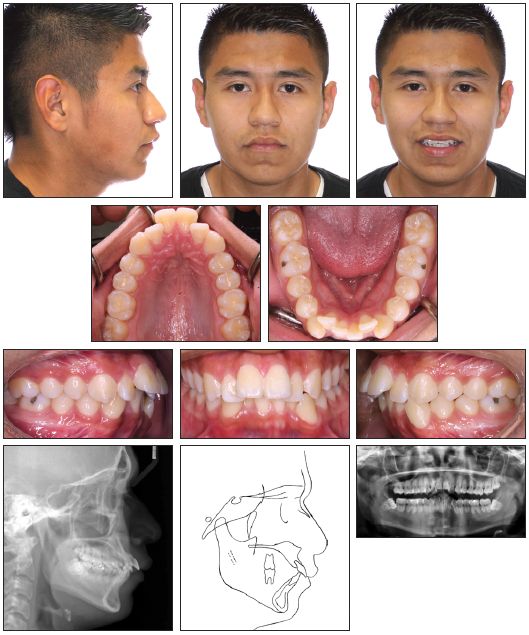
Fig. 1 17-year-old male patient with generalized short-root anomaly, severe anterior crowding, flared upper incisors, excessive overjet, and buccal occlusion before treatment.
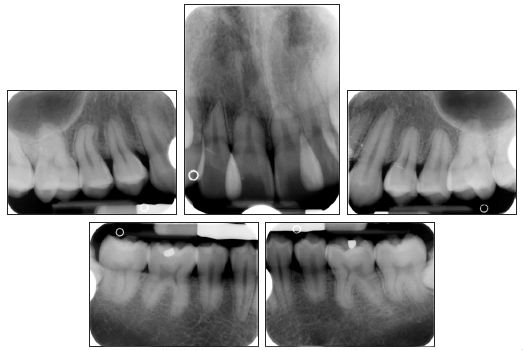
Fig. 1 (cont.) 17-year-old male patient with generalized short-root anomaly, severe anterior crowding, flared upper incisors, excessive overjet, and buccal occlusion before treatment.
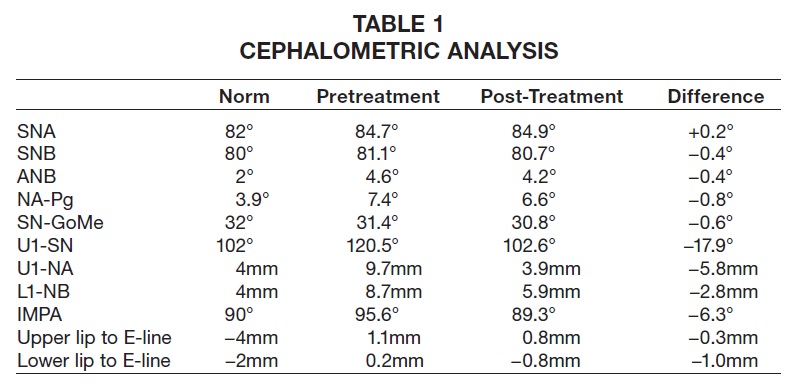
Cephalometric analysis indicated a Class II skeletal base and a convex profile due to a prognathic maxilla. The upper incisors were proclined, and both lips were protruded in relation to the E-line (Table 1). The panoramic radiograph revealed generalized short roots, impacted lower third molars, and a missing upper right third molar.
The root/crown ratios for the first molars, premolars, canines, and upper incisors were calculated as proposed by Lind.1 The most affected teeth were the upper right and left central incisors, with root/crown ratios of .85 and .90, respectively (Table 2).
The patient and his mother reported that no other family members had been diagnosed with short roots. Two brothers of the patient had been previously treated in our clinic and did not present with generalized SRA, but one displayed mild shortening of the premolars—a condition that worsened slightly during orthodontic treatment (Fig. 2).
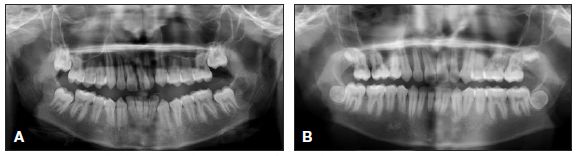
Fig. 2 Patient’s brother before (A) and after (B) orthodontic treatment.
The main treatment objectives in this case were to address the patient’s chief request of resolving maxillary and mandibular alignment, retract the upper incisors to improve their inclination and overjet, reduce lip protrusion, and maintain the molars and canines in a Class I occlusion. The first treatment option involved extraction of all first premolars to correct the alignment and overjet. Given the patient’s generalized SRA, we planned to use a targeted mechanics approach, as described above. The second option was nonextraction treatment to align the maxillary and mandibular dentition. This would increase the labial inclination of the incisors and likely impair the smile esthetics, however, and the duration of the required orthodontic forces might be detrimental to the affected teeth, especially the central incisors. The third option was no treatment, which was a reasonable consideration since the risk of root resorption could compromise the longevity of the teeth. After discussion, the patient and his mother consented to the first treatment plan.
The patient was referred to his general dentist for extraction of the upper and lower first premolars. Four LOMAS* 1.5mm × 9mm, 022"/.028" slot mini-implants were placed in the maxilla, two on each side, in a vertical configuration between the first molar and second premolar. The mini-implants on each side were splinted together with a mesh of stainless steel ligature ties and composite resin. A molar tube was then bonded to each stabilized mini-implant structure to engage the base archwire (Fig. 3).

Fig. 3 Targeted mechanics for canine retraction: four mini-implants placed in maxilla and two in mandible, .022" preadjusted edgewise brackets bonded to upper and lower canines, .016" × .022" stainless steel archwires passively adapted to engage slots of canines and mini-implant brackets, and nickel titanium coil springs attached from canine brackets to mini-implants.
Two additional mini-implants were placed in the mandible, one on each side, between the first molar and second premolar.
Preadjusted .022" edgewise brackets** were bonded to the upper and lower canines, and .016" × .022" stainless steel archwires were passively adapted to engage the slots of the canine and mini-implant brackets. Canine retraction was initiated by attaching nickel titanium coil springs with 120-150g of force from the canines to the mini-implants. Six months later, some spontaneous alignment of the upper and lower incisors was observed as a result of the anterior space creation (Fig. 4). A progress panoramic radiograph indicated translation of the upper canines and lower left canine; the lower right canine was slightly tipped.
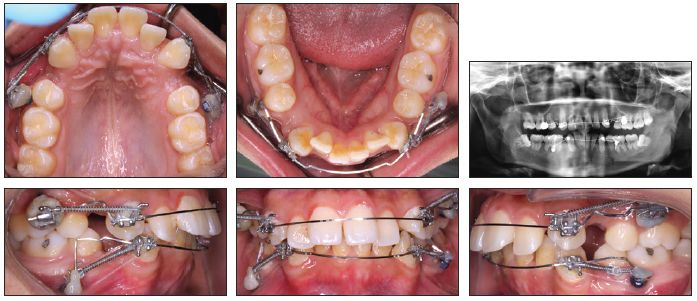
Fig. 4 After six months of canine retraction, incisor alignment spontaneously improved.
After 11 months of canine retraction, we noted additional spacing in the incisor regions and further spontaneous alignment of the upper and lower incisors, along with substantial movement of the left canines (Fig. 5). Some 3-4mm of space remained distal to the right canines.

Fig. 5 After 11 months of canine retraction, transpalatal arch soldered to upper canine bands and elastomeric chains attached from extension arms to mini-implants.
The maxillary mechanics were then modified for transverse control, with an .030" stainless steel transpalatal arch soldered to bands on the upper canines. Extension arms were soldered to the buccal surfaces of the bands so that the lines of force would pass close to the canine centers of resistance, and canine retraction was continued with elastomeric chains from the extension arms to the mini-implants. The previous mechanics were maintained in the mandibular arch.
Both upper canines and the lower left canine were fully retracted after 20 months of treatment. At this stage, both arches were bonded with .022" preadjusted edgewise brackets, and mini-implants were removed (Fig. 6).

Fig. 6 Both arches bonded with .022" preadjusted edgewise brackets, mini-implants removed, and leveling and alignment initiated after 20 months of treatment.
Over four months of leveling and alignment, archwires progressed to .019" × .025" stainless steel in the maxilla and .017" × .025" beta titanium in the mandible. The residual spaces around the lower right canine and upper incisors were closed with light elastomeric chain, requiring another three months. Finishing bends were added during the last two months of treatment, but the patient wore no intermaxillary elastics for anchorage or finishing. After a total 27 months of treatment, appliances were removed and vacuum-formed retainers were delivered (Fig. 7A).
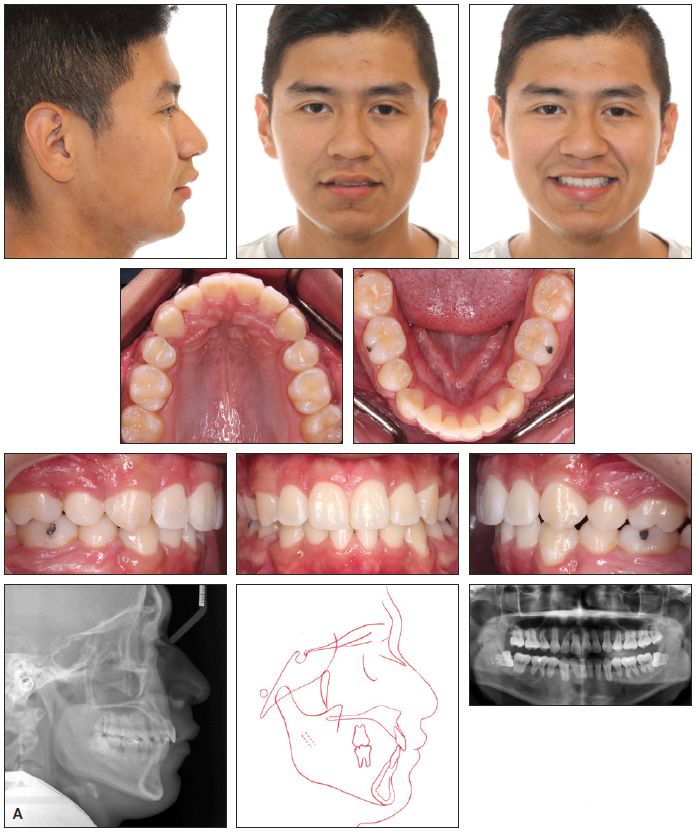
Fig. 7 A. Patient after 27 months of treatment.
Favorable dental and soft-tissue relationships were achieved, and the patient was pleased with the results. Both arches were well aligned; a Class I buccal occlusion was maintained on the right side, but the avoidance of intermaxillary elastics resulted in a slight loss of anchorage on the left side during final incisor retraction. The overjet was substantially reduced (from 7mm to 2mm), improving the lip position, smile esthetics, and profile. Cephalometric superimpositions indicated a slight decrease in the ANB angle and convexity (Fig. 7B).
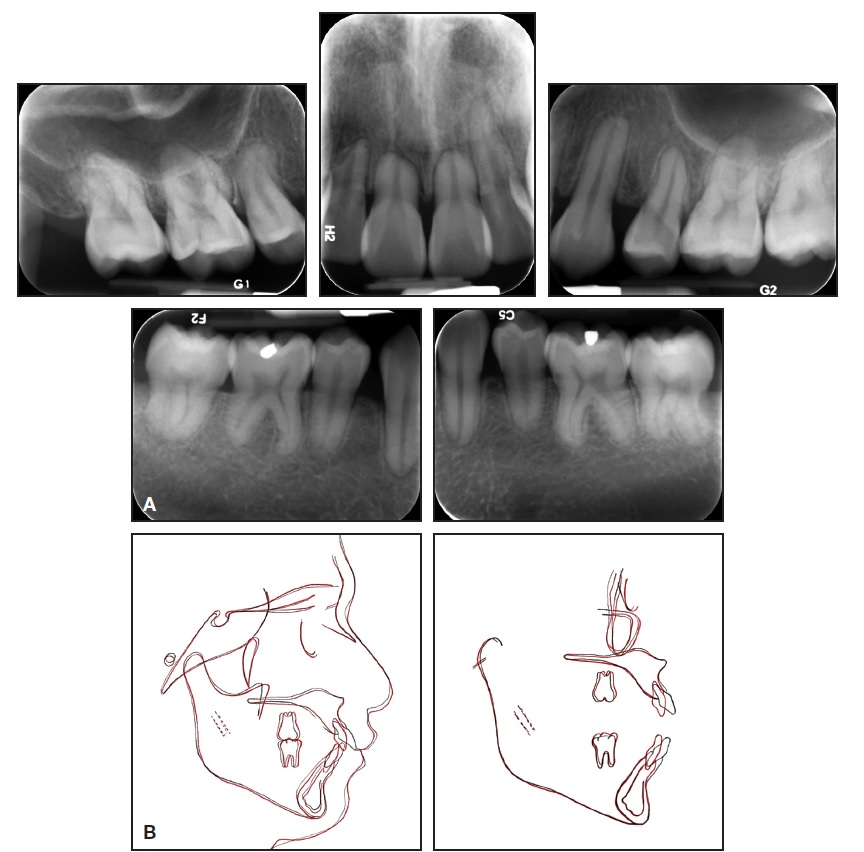
Fig. 7 (cont.) B. Superimposition of pre- and post-treatment cephalometric tracings.
The upper incisors were substantially retracted, and the lower incisor inclination was reduced. There was improvement in the lip projection, especially the lower, in relation to the E-line (Table 1). The length of the roots—including those of the canines, which underwent active retraction for about 20 months—was basically unchanged from the initial radiograph (Table 2). Because the lower third molars showed significant mesial angulation, they were recommended for removal, along with the unopposed upper left third molar.
Discussion
Patients with SRA do not display any systemic or local conditions that would explain their arrested root development. One report attempted to identify the molecular mechanism of SRA by analyzing the expression of matrix metalloproteinases (MMPs) in the gingival crevicular fluid of five patients with the condition.15 Although the activation of MMPs has been associated with tissue-destructive conditions such as periodontitis,16 this analysis found no significant resorptive or pathological activity in the crevicular fluid of teeth affected by SRA, supporting the conclusion that it is a developmental condition.15
Although the prevalence of SRA has been reported as 10% in the Japanese population,17 2.4% in the Swedish population,18 and 1.3% among Finnish young adults,2 it is probably higher since SRA is usually asymptomatic and frequently misdiagnosed as root resorption. In a recent cohort study conducted in the United States, 26 of the 27 patients with SRA were Latino, involving two families and 16 unrelated persons. Two of these 26 patients showed severe, generalized SRA.4 Our patient’s family is originally from Mexico, which may tend to confirm this apparent predilection for SRA among the Latino population.
Conventional orthodontic treatment is contraindicated in patients with SRA because of the increased risk of root resorption.19 A finite element model study of orthodontic forces showed that short roots experienced greater loading and stress than occurred with normal root configurations.20 As demonstrated by our case, careful mechanics and minimal forces are required for successful maintenance of root/crown ratios.1,5,10,11 Periodic radiographic monitoring and maintenance of periodontal health during orthodontic treatment can also prevent further damage.12
In this case, we performed a two-step space closure involving only canine retraction with mini-implant anchorage, followed by a quick completion of space closure and finishing. We used two splinted mini-implants on each side of the maxilla to create a rigid system and avoid rotational moments that might have caused failure of the skeletal anchorage units.21,22 This versatile method can be used in various situations to maintain a favorable buccal occlusion while correcting anterior problems, or when limited orthodontic treatment is necessary.
FOOTNOTES
- *Mondeal Medical Systems GmbH, Muhlheim a.d. Donau, Germany; www.mondeal.de.
- **Henry Schein Orthodontics, Melville, NY; www.henryschein.com.
REFERENCES
- 1. Lind, V.: Short root anomaly, Eur. J. Oral Sci. 80:85-93, 1972.
- 2. Apajalahti, S.; Hölttä, P.; Turtola, L.; and Pirinen, S.: Prevalence of short-root anomaly in healthy young adults, Acta Odontol. Scand. 60:56-59, 2002.
- 3. Edwards, D.M. and Roberts, G.J.: Short root anomaly, Br. Dent. J. 169:292-293, 1990.
- 4. Puranik, C.P.; Hill, A.; Henderson Jeffries, K.; Harrell, S.N.; Taylor, R.W.; and Frazier-Bowers, S.A.: Characterization of short root anomaly in a Mexican cohort—Hereditary idiopathic root malformation, Orthod. Craniofac. Res. 18 suppl. 1:62-70, 2015.
- 5. Apajalahti, S.; Arte, S.; and Pirinen, S.: Short root anomaly in families and its association with other dental anomalies, Eur. J. Oral Sci. 107:97-101, 1999.
- 6. Fulari, S.G. and Tambake, D.P.: Rootless teeth: Dentin dysplasia type I, Contemp. Clin. Dent. 4:520-522, 2013.
- 7. Beltes, C. and Zachou, E.: Endodontic management in a patient with vitamin D-resistant Rickets, J. Endod. 38:255-258, 2012.
- 8. De Man, K.: Abnormal root development, probably due to erythema multiforme (Stevens-Johnson syndrome), Int. J. Oral Surg. 8:381-385, 1979.
- 9. Roinioti, T.D. and Stefanopoulos, P.K.: Short root anomaly associated with Rothmund-Thomson syndrome, Oral Surg. Oral Med. Oral Path. Oral Radiol. Endod. 103:e19-e22, 2007.
- 10. Farret, M.M. and Farret, M.M.: Retreatment of a Class II patient with short-root anomaly, J. Clin. Orthod. 49:659-665, 2015.
- 11. Marques, L.S.; Generoso, R.; Armond, M.C.; and Pazzini, C.A.: Short-root anomaly in an orthodontic patient, Am. J. Orthod. 138:346-348, 2010.
- 12. Valladares Neto, J.; Rino Neto, J.; and de Paiva, J.B.: Orthodontic movement of teeth with short root anomaly: Should it be avoided, faced or ignored? Dent. Press J. Orthod. 18:72-85, 2013.
- 13. Librizzi, Z.T.; Janakiraman, N.; Rangiani, A.; Nanda, R.; and Uribe, F.A.: Targeted mechanics for limited posterior treatment with mini-implant anchorage, J. Clin. Orthod. 49:777-783, 2015.
- 14. Kim, S.H.; Hwang, Y.S.; Ferreira, A.; and Chung, K.R.: Analysis of temporary skeletal anchorage devices used for en-masse retraction: A preliminary study, Am. J. Orthod. 136:268-276, 2009.
- 15. Apajalahti, S.; Sorsa, T.; and Ingman, T.: Matrix metalloproteinase -2, -8, -9, and -13 in gingival crevicular fluid of short root anomaly patients, Eur. J. Orthod. 25:365-369, 2003.
- 16. Ingman, T.; Tervahartiala, T.; Ding, Y.; Tschesche, H.; Haerian, A.; Kinane, D.F.; Konttinen, Y.T.; and Sorsa, T.: Matrix metalloproteinases and their inhibitors in gingival crevicular fluid and saliva of periodontitis patients, J. Clin. Periodontol. 23:1127-1132, 1996.
- 17. Ando, S.; Kiyokawa, K.; Nakashima, T.; Shinbo, K.; and Sanka, Y.: Studies on the consecutive surgery of succedaneous and permanent dentition in Japanese children, 4. Behavior of short-rooted teeth in the upper bilateral central incisors, J. Nihon Univ. Sch. Dent. 9:67-82, 1967.
- 18. Jakobsson, R. and Lind, V.: Variation in root length of the permanent maxillary central incisor, Scand. J. Dent. Res. 81:335-338, 1973.
- 19. Thongudomporn, U. and Freer, T.J.: Anomalous dental morphology and root resorption during orthodontic treatment: A pilot study, Aust. Orthod. J. 15:162-167, 1998.
- 20. Oyama, K.; Motoyoshi, M.; Hirabayashi, M.; Hosoi, K.; and Shimizu, N.: Effects of root morphology on stress distribution at the root apex, Eur. J. Orthod. 29:113-117, 2007.
- 21. Lee, J.S.; Kim, D.H.; Park, Y.C.; Kyung, S.H.; and Kim, T.K.: The efficient use of midpalatal miniscrew implants, Angle Orthod. 74:711-714, 2004.
- 22. Leung, M.T.; Rabie, A.B.; and Wong, R.W.: Stability of connected mini-implants and miniplates for skeletal anchorage in orthodontics, Eur. J. Orthod. 30:483-489, 2008.