OVERVIEW
Predictability of Orthodontic Forced Eruption in Developing an Implant Site: A Systematic Review
(Editor’s Note: In this regular column, JCO provides an overview of a clinical topic of interest to orthodontists. Contributions and suggestions for future subjects are welcome.)
For teeth with a hopeless prognosis - periodontally weakened, severely mobile, grossly carious, or non-restorable - extraction and replacement are usually indicated. When an implant is considered in such a case, adequate bone and soft-tissue levels are essential to treatment success. Bony defects will inevitably compromise implant stability; gingival defects may lead to a poor esthetic appearance of the implant and impairment of oral hygiene.
Protocols for ridge preservation and augmentation, including guided bone regeneration, grafting techniques, ridge splitting, and distraction osteogenesis, have traditionally been used to improve the bony housing before or during implant placement.1 Corrective gingival surgeries such as connective-tissue grafts, coronally positioned flaps, and free gingival grafts have been proposed to address the problem of soft-tissue defects surrounding implants.2 Arguably, however, most of these techniques have shown limited success. While grafting can effectively augment bone in a horizontal direction, its ability to regenerate bone vertically has been poor.3 Soft-tissue grafting has also been linked to significant morbidity of the donor site and is prone to graft failure.4
Similar articles from the archive:
In an attempt to overcome such shortcomings, orthodontic forced eruption (OFE) has recently emerged as a viable nonsurgical alternative for developing the future implant site.5 It relies on the principle that a hopeless tooth should no longer be regarded as useless, but instead can be exploited by orthodontic means to regenerate bone and soft tissue. Under the application of a controlled orthodontic force, mechanical stresses on alveolar bone lead to the stimulation of angiogenic factors responsible for new bone formation. As the tooth is extruded, simultaneous stretching of periodontal fibers causes a coronal migration of the gingiva, resulting in an enhanced emergence profile of the implant restoration.
As evidenced by several studies, the benefits of OFE in terms of hard- and soft-tissue augmentation around implants cannot be overemphasized.6-8 Nevertheless, clinicians' concerns about the risks of treating a compromised tooth, the complexity of orthodontic treatment, the additional costs involved, the prolonged treatment time, and poor patient compliance have limited its application. The present systematic review was designed to quantify the predictability of this treatment modality in augmenting bone and keratinized soft tissue. Adverse events related to the use of OFE were also investigated.
Materials and Methods
The problem assessed was the presence of a hopeless tooth planned for later extraction and replacement with an implant. The treatment protocol involved intervention with OFE prior to implant placement. Primary outcomes included the amount of newly formed bone and the amount of soft-tissue augmentation that could be achieved as the tooth was extruded. Secondary outcomes were any adverse events related to such treatment.
Search Criteria
A systematic computerized search of articles published through July 2015 was conducted to identify case series or reports related to the use of OFE for implant-site development. Databases included in the search were Ovid Medline, Thomson's ISI Web of Science, PubMed, Embase, and the Cochrane library. Studies had to be written in English and include quantitative data describing improvement in the amount of bone or soft tissue. Exclusion criteria were as follows:
- Studies in which no quantitative comparisons of pre- and post-treatment changes were reported.
- Studies reporting forced eruption by means other than orthodontic treatment.
- Experimental studies in animals.
- Articles in which details about orthodontic treatment, implant placement, or the prosthodontic phase were missing.
- Letters, editorials, theses, abstracts, and unretrievable full-text articles.
- Articles with obvious sources of bias.
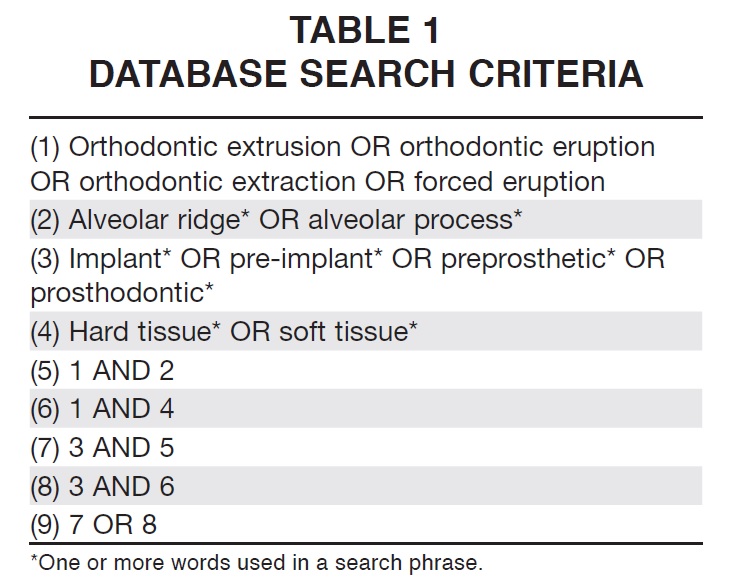
Similar keywords were used whenever possible, but terms were truncated and combined as appropriate (Table 1). The reference lists of all selected articles were also searched manually to identify any studies that may have been missed in the electronic search. To better refine the quality of data, whenever more than one publication about the same patient group was identified, the most informative and relevant article was selected for inclusion. It should be noted that no authors were contacted.
Study Selection and Data Extraction
Once the computerized search was completed, studies were selected in a two-stage process. In the first stage, two reviewers (Drs. Somar and Mohadeb) screened the databases, removed any duplicates, and read the article abstracts. In the second stage, the full texts of selected articles were retrieved and independently scrutinized by both reviewers. Any disagreement during this phase was discussed, and a third reviewer (Dr. Huang) was consulted when necessary. Data-extraction forms covering general descriptive characteristics and details of the orthodontic and post-orthodontic treatment phases were compiled and cross-checked by two reviewers.
Quality evaluation of the case reports and series was performed using the Case Report (CARE) guidelines, which include 13 key clinical components.9 These guidelines were chosen over the Yang Scale10 because of their flexibility in weighting and their proven efficacy in evaluating non-randomized controlled trials.
Results
Study Selection
The primary search returned a total of 491 articles (Fig. 1). After the first stage of screening, only 65 full-text articles were retrieved for a more detailed evaluation. Twenty-seven of these articles did not meet the selection criteria, resulting in a total of 38 potentially appropriate articles. Two pertinent articles were added from the manual search, for a total of 40.
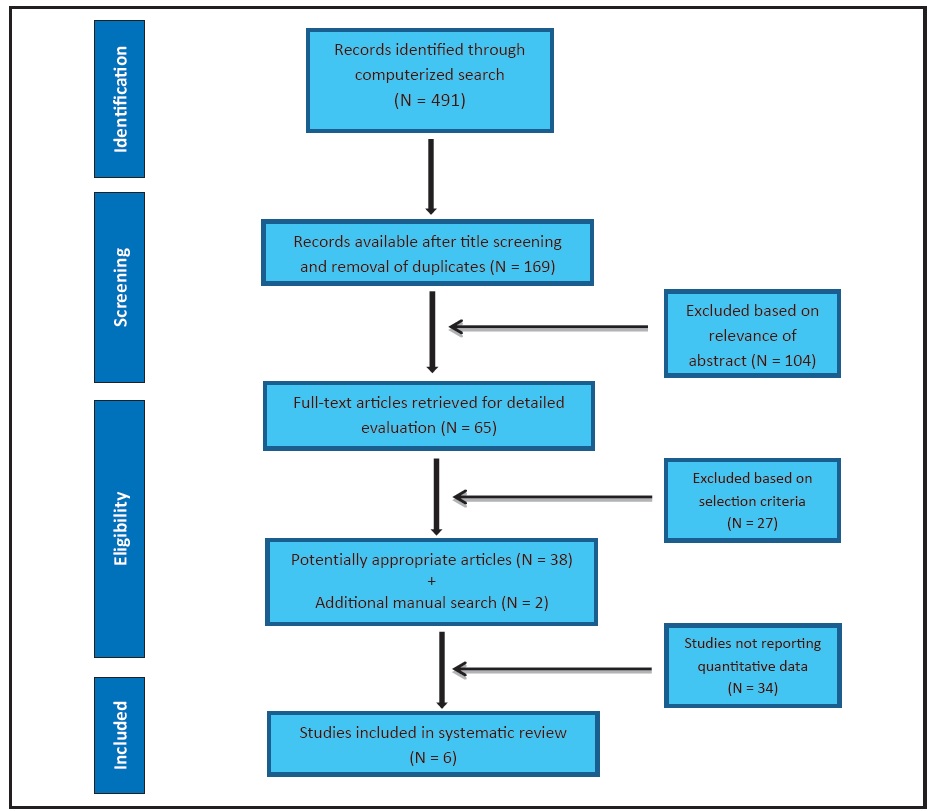
Fig. 1 Flow chart illustrating selection of relevant articles.
While most of the articles reported qualitative data, only six studies clearly quantified the post treatment changes resulting from OFE; therefore, these were the only studies considered in our review.11-16 Two articles from the same author were combined since they included details of the same patient.15,16
Quality of Data and Assessment of Bias
Interexaminer agreement during the selection process was considered reliable: there were only two inconsistencies, and those articles were subsequently rejected because the preoperative measurements were inadequately reported. Quality grading of the included studies using the CARE guidelines ranged from medium to high.
Study Characteristics
Seventeen patients were assessed among the five sets of authors, with OFE used on a total of 41 teeth for implant site development (Table 2).
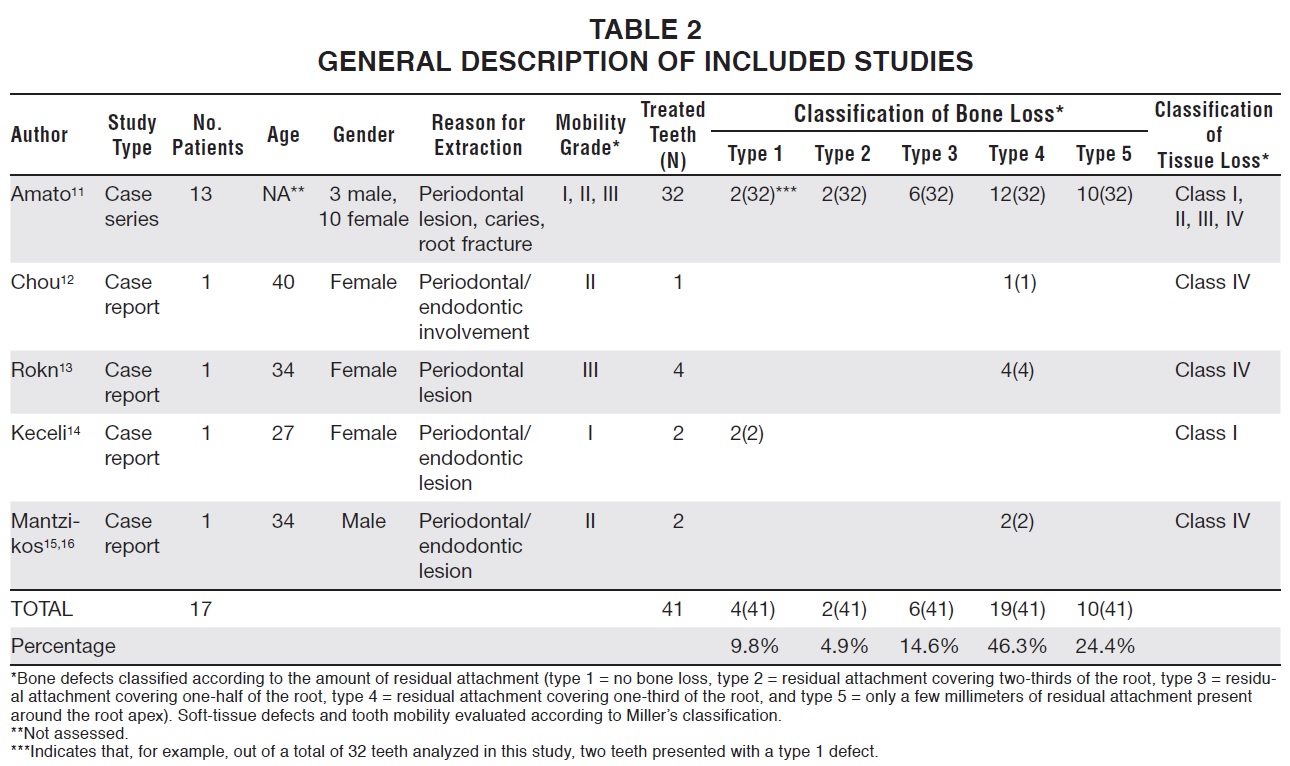
Age, gender, degree of tooth mobility, and amount of bone or soft-tissue destruction did not appear to present any limitations to the technique. With the exception of the study by Chou and colleagues,12 in which OFE was used to extrude a lower molar, all treatments were carried out in the maxillary esthetic zone. In two different articles (by Amato and colleagues11 and Keceli and colleagues14), both involving type 1 bone defects and Class I gingival defects, OFE was used to overbuild the implant sites as a means of ridge preservation.
Tooth movement was achieved with either a partial or full orthodontic bracket setup (Table 3).
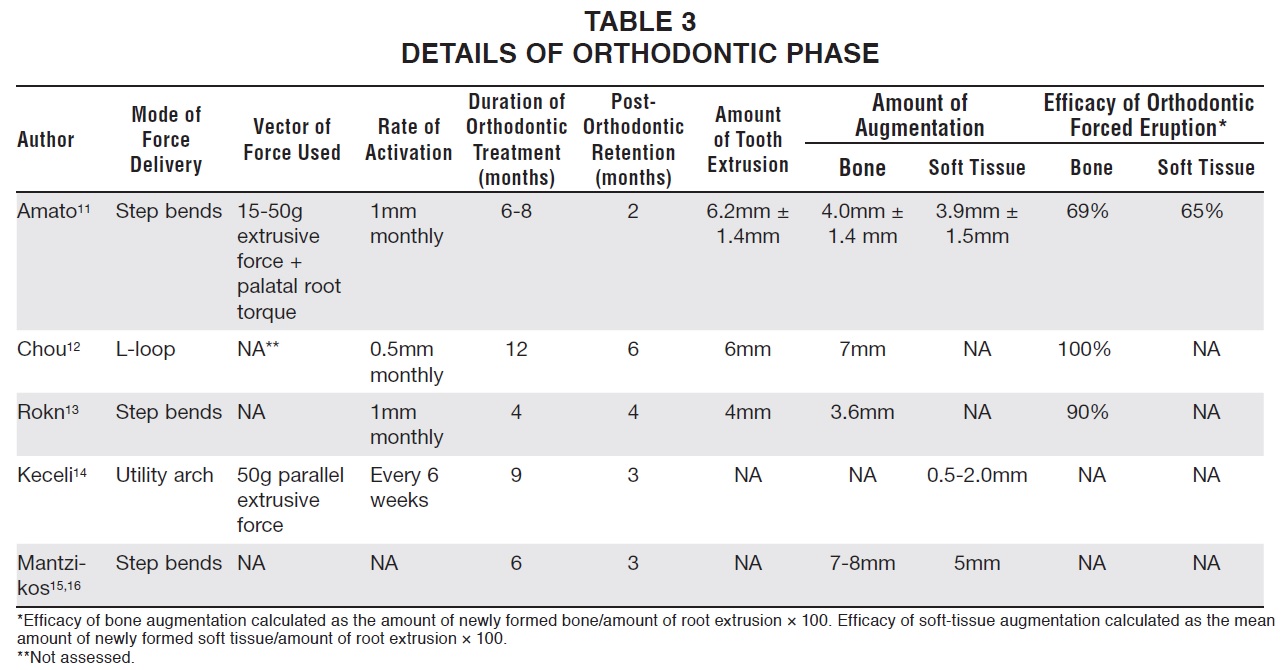
In two studies (by Chou and colleagues12 and Keceli and colleagues14), OFE was performed as an adjunct to adult orthodontic treatment. Overall, the orthodontic treatment duration ranged from six to 12 months, followed by a retention period of two to six months.
The magnitude and direction of orthodontic force varied among the studies. Unlike the other authors, who reported .5-1mm of active extrusion per month, Keceli and colleagues demonstrated successful treatment with an activation rate of 1mm per week followed by three weeks of inactivation.14 The efficacy of bone augmentation ranged from 69% to 100%; only one study (by Amato and colleagues) reported keratinized soft-tissue augmentation, at an average efficacy of 65%.11
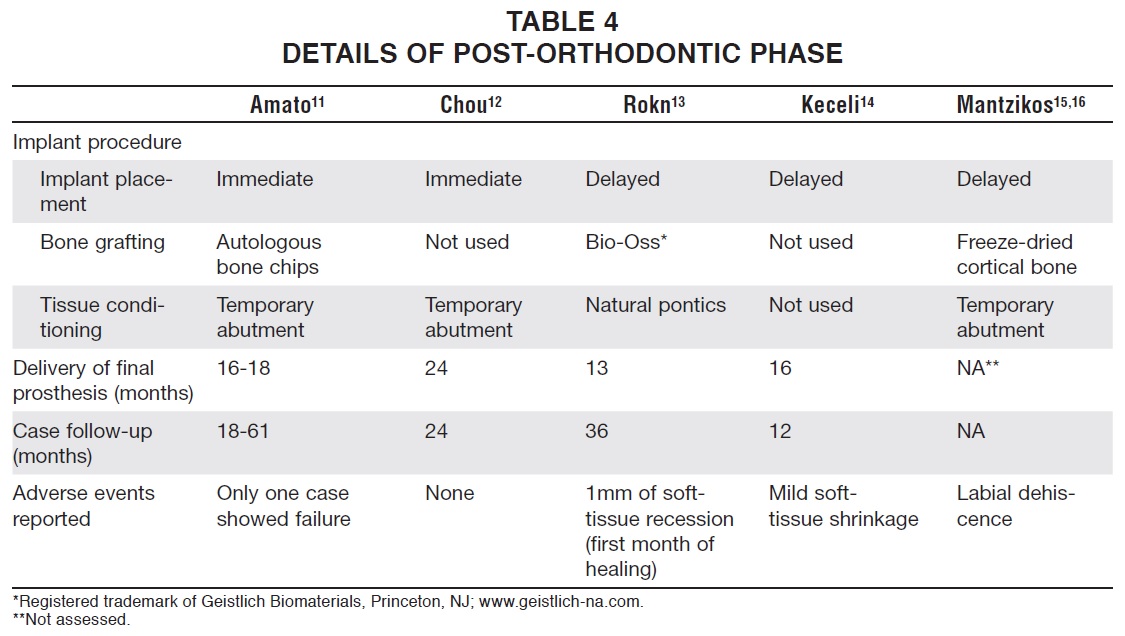
In a few cases, bone grafts were employed for secondary bone coverage (Table 4). While most authors used artificial prostheses to maintain the soft-tissue improvements, Rokn and colleagues described a newer alternative in which the extracted teeth were shaped to function as natural pontics during healing.13 Even after one to two years of follow-up, the survival of the implants in these augmented sites was not compromised.
Discussion
Six studies providing quantitative data on OFE were used to report the outcomes of implant-site development for this review.11-16 One study was a case series, while the others were clinical case reports. Because case reports and series are considered to be the lowest level of the evidencebase pyramid, they are usually omitted in systematic reviews. Expecting to find randomized controlled trials of OFE, however, would have been unreasonable due to the nature of the intervention. We therefore determined that case reports and case series represented the only available source of scientific information on this treatment modality.
Predictability of OFE in Bone Augmentation
Inadequate bone height, width, or quality can compromise implant positioning. Interventions to correct these conditions have been classified as horizontal or lateral augmentation (increasing ridge width) or vertical ridge augmentation (increasing height). OFE has reportedly been effective in ridge-width augmentation, and a few authors have observed labial bone formation when combining a vertical extrusive force with a torqueing movement.17,18 Since they provided no quantitative data, however, we could not predict an associated success rate in this review.
Evidence from the included studies shows that an efficacy of 69-100% in vertical bone augmentation can be expected following OFE, even if less than one-third of the residual attachment remains around the involved tooth. Amato and colleagues reported an overall efficacy of 69% in bone formation, attributing the lost 31% to the eruption of the tooth through the periodontal pocket.11 Chou and colleagues reported a greater amount of bone formation (more than 100%) from forced eruption of a lower posterior tooth,12 while Rokn and colleagues noted an average 90% efficacy of bone formation during the extrusion of four anterior teeth.13 In summary, for every 1mm of vertical tooth extrusion, an average .69-1mm of bone apposition can be expected, depending on the direction and magnitude of force.
In general, forces of low magnitude are recommended, with the reported activation rate ranging from 1mm per month to 1mm per week. Heavier forces or accelerated movement may lead to tissue damage or ankylosis, limiting the amount of new bone formation.19 A vertically directed force along the tooth axis has traditionally been used to effectuate tooth movement, resulting in bone formation in both the apical and marginal regions, as an initially uncalcified organic matrix of osteoid tissue attains full maturation in around 24 weeks. Experimental studies have confirmed that this pattern of bone apposition is greater in the apical area than in the coronal area.20 Uribe and colleagues recently recommended a modification in the direction of force to maximize the clinical benefits of OFE.21 Considering the conical shape of the dental root, they suggested that a greater cross sectional area of the root would be involved by tipping the tooth in the direction of the angular defect as it was extruded, thereby increasing the amount of bone formation.
Predictability of OFE in Keratinized Soft-Tissue Augmentation
Although soft tissue exhibits more variation than hard tissue in development and distribution, changes in soft-tissue architecture accompanying the extrusion of a hopeless tooth reportedly influence both the width of attached or interdental gingiva and the gingival thickness. As reported by only one study in our review, changes in the width of the attached gingiva can range from negligible to 100% efficacy, with an average of 65%.11 This finding disagrees with a previous experimental study of monkeys, in which Kajiyama and colleagues noted a much greater augmentation of 90% in the free gingiva and 80% in the attached gingiva.22
When attempting to predict the growth of keratinized soft tissue in an implant site, several diagnostic factors should be considered. In a patient with only mild soft-tissue damage before treatment (mucogingival junction firmly attached to bone, attached gingiva connected to the dental root, and no periodontal pockets), the efficacy of soft-tissue augmentation can be even greater than 65% - meaning that for every 1mm the tooth is extruded, the width of attached gingiva increases by at least .65mm. Conversely, in a case with more severe soft-tissue damage (weak attachment of the mucogingival junction to bone and of gingiva to the dental root, with persistent periodontal pockets), there will be no improvement in soft-tissue development, only bone formation.
We were unable to find any quantitative evidence regarding changes in the interpapillary gingiva. Although Keceli and colleagues documented adequate preservation of the papillary height during OFE, they did not provide data on the rate of extrusion, making it impossible to determine the efficacy of the technique.14 Based on the findings of Tarnow and colleagues, soft-tissue formation follows the osseous contour; therefore, if the contact point is at least 5mm from the osseous crest before treatment, an effective papillary formation can be anticipated.23 Other authors have indicated that adequate periodontal attachment of the adjacent teeth is a prime determinant of papillary formation.24 In other words, OFE of a failing tooth will not improve the height of the interproximal papilla without a healthy periodontal attachment on the adjacent teeth.
A thicker soft-tissue biotype, being more resistant to mechanical and surgical insults, can positively affect the esthetic outcome of an implant restoration after OFE. Fu and colleagues reported such results when using controlled facial and vertical extrusive forces.25 More recently, Le and Borzabadi-Farahani demonstrated a high correlation between an implant's labial bone thickness and the labial soft-tissue thickness.26 As the alveolar ridge width increases under the influence of a controlled facial extrusive force, the labial soft tissue will obviously thicken.
Adverse Events Associated with OFE
Patients in the studies included in this review were generally followed for 12-36 months, during which implant failure rates were negligible. Primary implant stability was achieved by the deposition of natural bone, and grafts were used only for secondary coverage. At the soft-tissue level, only slight tissue shrinkage was reported over several years. When low and controlled forces were used to effectuate tooth movement, no perforation of cortical plates was reported. Overall, patient satisfaction was high and expectations were successfully met.
Conclusion
Our review indicates that OFE can be effective in both ridge-height and ridge-width augmentation, although its contribution to soft-tissue development needs to be confirmed by future case reports using newer techniques and more accurate measurements. Before undertaking vertical extrusion of a compromised tooth, a preliminary assessment of the mucogingival junction attachment to bone, the gingival attachment to the dental root, the depth of periodontal pockets, the underlying bone topography, and the attachment level of adjacent teeth should be performed to determine the prognosis for successful treatment. Given careful planning and case selection, a compromised tooth can effectively augment bone and soft tissue with minimal adverse effects.
REFERENCES
- 1. Rocchietta, I.; Fontana, F.; and Simion, M.: Clinical outcomes of vertical bone augmentation to enable dental implant placement: A systematic review, J. Clin. Periodontol. 35:203- 215, 2008.
- 2. Thoma, D.S.; Buranawat, B.; Hämmerle, C.H.; Held, U.; and Jung, R.E.: Efficacy of soft tissue augmentation around dental implants and in partially edentulous areas: A systematic review, J. Clin. Periodontol. 41:S77-S91, 2014.
- 3. Tonetti, M.S.; Hammerle, C.H.; and European Workshop on Perdiodontology Group C: Advances in bone augmentation to enable dental implant placement: Consensus Report of the Sixth European Workshop on Periodontology, J. Clin. Periodontol. 35:168-172, 2008.
- 4. Hatipoglu, H.; Keceli, H.G.; Guncu, G.N.; Sengun, D.; and Tozum, T.F.: Vertical and horizontal dimensional evaluation of free gingival grafts in the anterior mandible: A case report series, Clin. Oral Investig. 11:107-113, 2007.
- 5. Salama, H. and Salama, M.: The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: A systematic approach to the management of extraction site defects, Int. J. Period. Res. Dent. 13:312-333, 1993.
- 6. Korayem, M.; Flores-Mir, C.; Nassar, U.; and Olfert, K.: Implant site development by orthodontic extrusion: A systematic review, Angle Orthod. 78:752-760, 2008.
- 7. Brindis, M.A. and Block, M.S.: Orthodontic tooth extrusion to enhance soft tissue implant esthetics, J. Oral Maxillofac. Surg. 67:49-59, 2009.
- 8. Farahani, A. and Zadeh, H.H.: Adjunctive orthodontic applications in dental implantology, J. Oral Implantol. 41:501-508, 2015.
- 9. Gagnier, J.J.; Kienle, G.; Altman, D.G.; Moher, D.; Sox, H.; Riley, D.; and CARE Group: The CARE guidelines: Consensus-based clinical case report guideline development, J. Clin. Epidemiol. 67:46-51, 2014.
- 10. Yang, A.W.; Li, C.G.; Da Costa, C.; Allan, G.; Reece, J.; and Xue, C.C.: Assessing quality of case series studies: Development and validation of an instrument by herbal medicine CAM researchers, J. Altern. Complement. Med. 15:513- 522, 2009.
- 11. Amato, F.; Mirabella, A.D.; Macca, U.; and Tarnow, D.P.: Implant site development by orthodontic forced extraction: A preliminary study, Int. J. Oral Maxillofac. Implants 27:411- 420, 2012.
- 12. Chou, Y.H.; Du, J.K.; Chou, S.T.; Hu, K.F.; Tsai, C.C.; Ho, K.Y.; Wu, Y.M.; and Ho, Y.P.: An interdisciplinary treatment approach combining orthodontic forced eruption with immediate implant placement to achieve a satisfactory treatment outcome: A case report, Clin. Implant Dent. Relat. Res. 15:113-120, 2013.
- 13. Rokn, A.R.; Saffarpour, A.; Sadrimanesh, R.; Iranparvar, K.; Saffarpour, A.; Mahmoudzadeh, M.; and Soolari, A.: Implant site development by orthodontic forced eruption of nontreatable teeth: A case report, Open Dent. J. 6:99-104, 2012.
- 14. Keceli, H.G.; Guncu, M.B.; Atalay, Z.; and Evginger, M.S.: Forced eruption and implant site development in the aesthetic zone: A case report, Eur. J. Dent. 8:269-275, 2014.
- 15. Mantzikos, T. and Shamus, I.: Case report: Forced eruption and implant site development, Angle Orthod. 68:179-186, 1998.
- 16. Mantzikos, T. and Shamus, I.: Forced eruption and implant site development: An osteophysiologic response, Am. J. Orthod. 115:583-591, 1999.
- 17. Zuccati, G. and Bocchieri, A.: Implant site development by orthodontic extrusion of teeth with poor prognosis, J. Clin. Orthod. 37:307-311, 2003.
- 18. Nozawa, T.; Sugiyama, T.; Yamaguchi, S.; Ramos, T.; Komatsu, S.; Enomoto, H.; and Ito, K.: Buccal and coronal bone augmentation using forced eruption and buccal root torque: A case report, Int. J. Period. Res. Dent. 23:585-591, 2003.
- 19. Buskin, R.; Castellon, P.; and Hochstedler, J.L.: Orthodontic extrusion and orthodontic extraction in preprosthetic treatment using implant therapy, Pract. Period. Aesthet. Dent. 12:213-219, 2000.
- 20. Van Venrooy, J.R. and Yukna, R.A.: Orthodontic extrusion of single-rooted teeth affected with advanced periodontal disease, Am. J. Orthod. 87:67-74, 1985.
- 21. Uribe, F.; Taylor, T.; Shafer, D.; and Nanda, R.: A novel approach for implant site development through root tipping, Am. J. Orthod. 138:649-655, 2010.
- 22. Kajiyama, K.; Murakami, T.; and Yokota, S.: Gingival reactions after experimentally induced extrusion of the upper incisors in monkeys, Am. J. Orthod. 104:36-47, 1993.
- 23. Tarnow, D.P.; Magner, A.W.; and Fletcher, P.: The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla, J. Periodontol. 63:995-996, 1992.
- 24. Wang, H.L.; Shotwell, J.L.; Itose, T.; and Neiva, R.F.: Multidisciplinary treatment approach for enhancement of implant esthetics, Implant Dent. 14:21-29, 2005.
- 25. Fu, J.H.; Lee, A.; and Wang, H.L.: Influence of tissue biotype on implant esthetics, Int. J. Oral Maxillofac. Implants 26:499- 508, 2011.
- 26. Le, B.T. and Borzabadi-Farahani, A.: Labial bone thickness in area of anterior maxillary implants associated with crestal labial soft-tissue thickness, Implant Dent. 21:406-410, 2012.




