CASE REPORT
Compensatory Retreatment of an Adult Class II Deep-Bite Patient
When an adult patient presents for retreatment of a moderate skeletal Class II malocclusion and deep bite, both dental and facial characteristics must be carefully evaluated and weighed along with the patient's chief complaint.1,2 Camouflage treatment to mask the skeletal problem may be a viable alternative for adult patients, particularly those who do not want to face the additional costs and risks involved with orthognathic surgery.3-5 A treatment plan involving dental compensations must be fully discussed with the patient and should only be offered when the orthodontist is positive that satisfactory esthetic and functional results will be achieved.
Although an excessive vertical dimension and transverse deficiency of the maxilla may be associated with the development of a skeletal Class II, Hunter observed that the dysplasia in these patients occurs most often in the sagittal plane.6 When a full-step Class II without crowding is treated with the extraction of two upper premolars, the six upper anterior teeth must be retracted to fully occupy the premolar extraction spaces; thus, the canines will finish in a Class I relationship, while the molars remain in Class II.7 Anchorage control is a key to success. The introduction of titanium mini-implants has significantly improved the orthodontist's ability to achieve maximum anchorage for anterior retraction with minimal patient cooperation.8,9
This report describes compensatory orthodontic retreatment of an adult patient with a Class II, division 1 malocclusion and deep bite, using mini-implants for anchorage control after the extraction of both upper first premolars.
Similar articles from the archive:
- CASE REPORT Retreatment of a Class II Patient with Short-Root Anomaly October 2015
- CASE REPORT Retreatment of an Adult Skeletal Class II Patient September 2013
- An Approach to Incisor Retreatment February 1976
Diagnosis and Treatment Plan
A 25-year-old female sought orthodontic retreatment because she was dissatisfied with the results of the treatment performed when she was a teenager, especially her overbite. She also complained about gingival pain during mastication.
The clinical examination showed a symmetrical face, convex profile, incompetent lip seal at rest, and excessive maxillary incisor display upon smiling (Fig. 1).
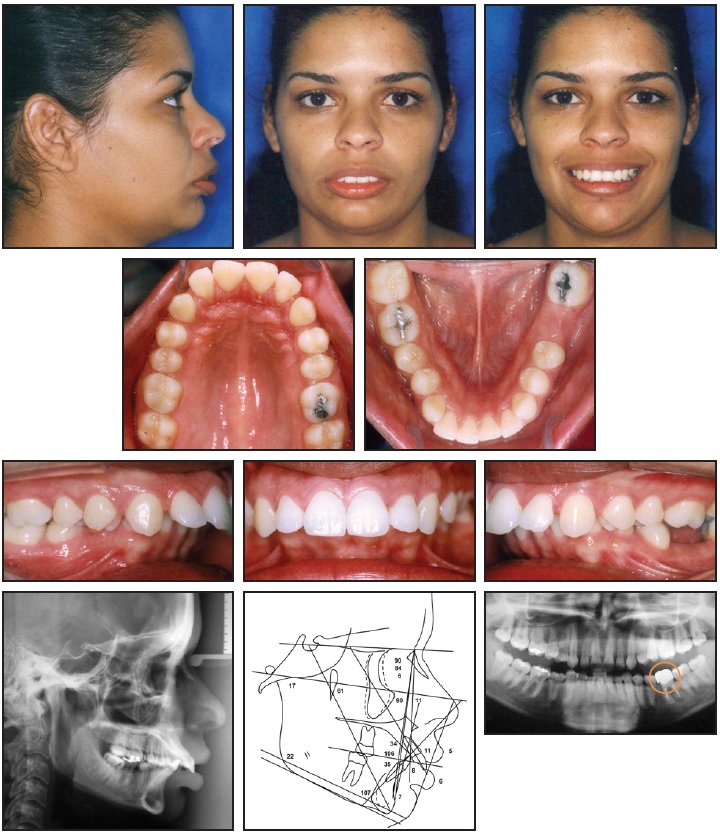
Fig. 1 25-year-old female patient with Class II, division 1 malocclusion and deep bite before treatment (circle on panoramic radiograph indicates first molar extracted due to lesion in furcation).
The panoramic radiograph indicated adequate levels of alveolar bone and the presence of all teeth, including the third molars. (Because the lower left first molar had a lesion in the region of the furcation, it was extracted before the initial photographs were taken.) Cephalometric analysis confirmed the Class II malocclusion (ANB = 6o, Wits appraisal = +5mm), as well as brachyfacial characteristics (SNGoGn = 22º and FMA = 17º). Functional analysis showed that centric relation was coincident with centric occlusion; there were no signs of TMD.
Treatment goals were to establish a Class I canine relationship and achieve ideal overjet and overbite, with a mutually protected functional occlusion. The ideal treatment plan presented to the patient involved orthognathic surgery to advance the mandible. Because she had no complaints about her facial appearance and did not wish to assume the costs and risks involved with the surgical orthodontic option, however, she elected to undergo compensatory orthodontic treatment. This plan involved leveling the curve of Spee and correcting the overjet after the extraction of both upper first premolars. Titanium mini-implants would be inserted between the upper second premolars and first molars to provide anchorage for maximum retraction of the anterior teeth. The space resulting from extraction of the lower left first molar would be maintained for an implant-supported restoration.
Treatment Progress
A maxillary alginate impression was obtained for fabrication of a removable full-coverage maxillary splint to open the bite and allow bonding of the mandibular fixed appliances (Fig. 2).
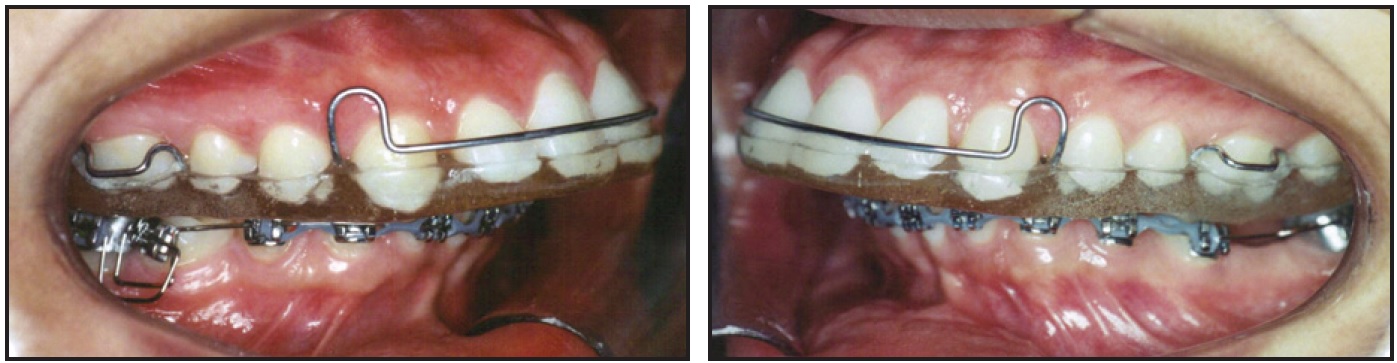
Fig. 2 Full-coverage maxillary splint and initial mandibular standard edgewise appliances.
The splint was adjusted with the patient in centric relation, following Dawson's bilateral manipulation technique to ensure simultaneous bilateral contacts of similar intensity in centric occlusion.7
Mandibular .022" x .028" standard edgewise appliances* were bonded from second molar to second molar for leveling and alignment, with archwires progressing up to .020" stainless steel*. The maxillary splint was adjusted at each monthly appointment to eliminate potential interferences created by the changes in tooth positions. Six months into treatment, the patient was able to occlude without contacting the lower brackets, and the splint was discontinued.
At this point, .022" x .028" standard edgewise appliances were bonded in the maxillary arch, taking care to allow enough space between the first-molar and second-premolar roots for miniscrew insertion. Leveling and alignment progressed to an .018" x .025" stainless steel rectangular archwire** with rounded edges.
After nine months of treatment, the miniscrews*** were inserted, and the patient was referred for extraction of the first premolars. One week after the extractions, 100g nickel titanium closed-coil springs† were attached between the miniscrews and a crimpable hook positioned mesial to the canine brackets to move these teeth independently (Fig. 3).
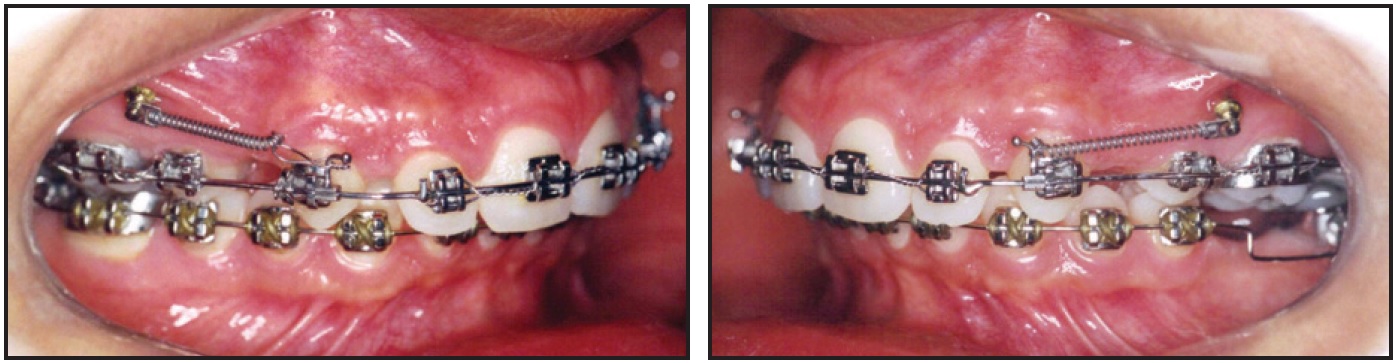
Fig. 3 Maxillary canine retraction with miniscrew anchorage.
Four weeks later, once the upper canines were in a Class I relationship, an .019" x .025" closing-loop archwire with Bull loops distal to the lateral incisors was placed for incisor retraction (Fig. 4).
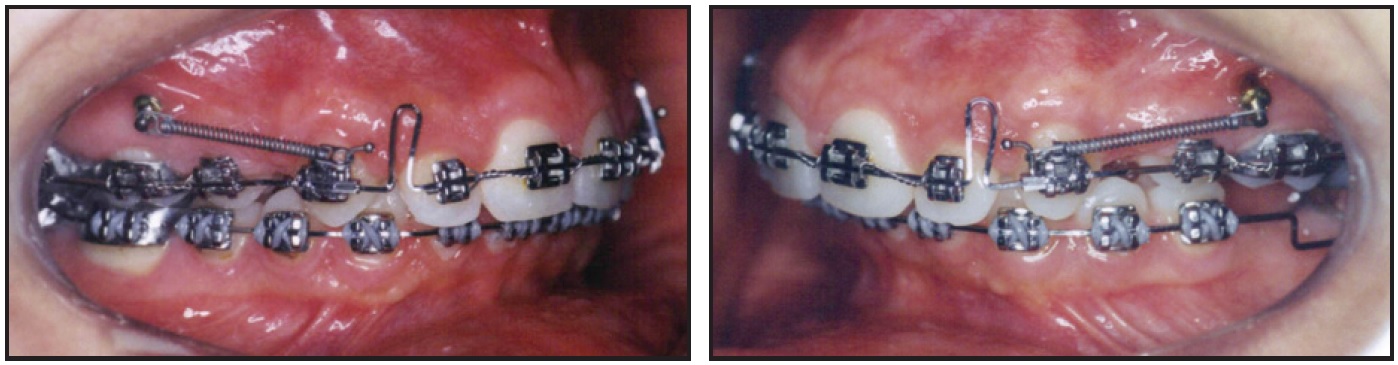
Fig. 4 Closing-loop archwire used for maxillary incisor retraction.
Sixteen months into treatment, the upper-incisor retraction had been completed, and a panoramic radiograph was obtained to check for root parallelism. An .019" x .025" stainless steel ideal archwire was bent to finish detailing of the occlusion. Six months before appliance removal, the patient was referred to a periodontist and a prosthodontist for an implant-supported restoration of the lower left first molar.
After a total 36 months of treatment, all brackets were debonded. A lower fixed 3-3 retainer wire (.028" stainless steel) was placed, and an upper wraparound retainer was delivered to be worn full-time for the first year and 12 hours per day for the following year.
Treatment Results
Post-treatment records confirmed that the main treatment goals were achieved (Fig. 5A).

Fig. 5 A. Patient after 36 months of treatment. B. Superimposition of pre- and post-treatment cephalometric tracings.
A significant improvement was seen in facial esthetics due both to the reduced labial protrusion and to a better labiomental sulcus angle with proper lip seal at rest. The smile contour remained pleasant because the inclination of the upper incisors had been controlled during their retraction. In the final occlusion, the Class II molar relationship had been maintained while the canines were moved into a Class I relationship. Periapical radiographs showed no significant root resorption of either the upper or lower incisors, despite the extensive upper-incisor retraction.
Cephalometric superimpositions showed that the SNA angle remained unchanged, even with the incisor retraction (Fig. 5B). There was a small counterclockwise mandibular rotation, as demonstrated by a reduction in the vertical dimension.
The patient was highly cooperative and wore her upper retainers as recommended. Treatment results remained stable three years after debonding (Fig. 6).
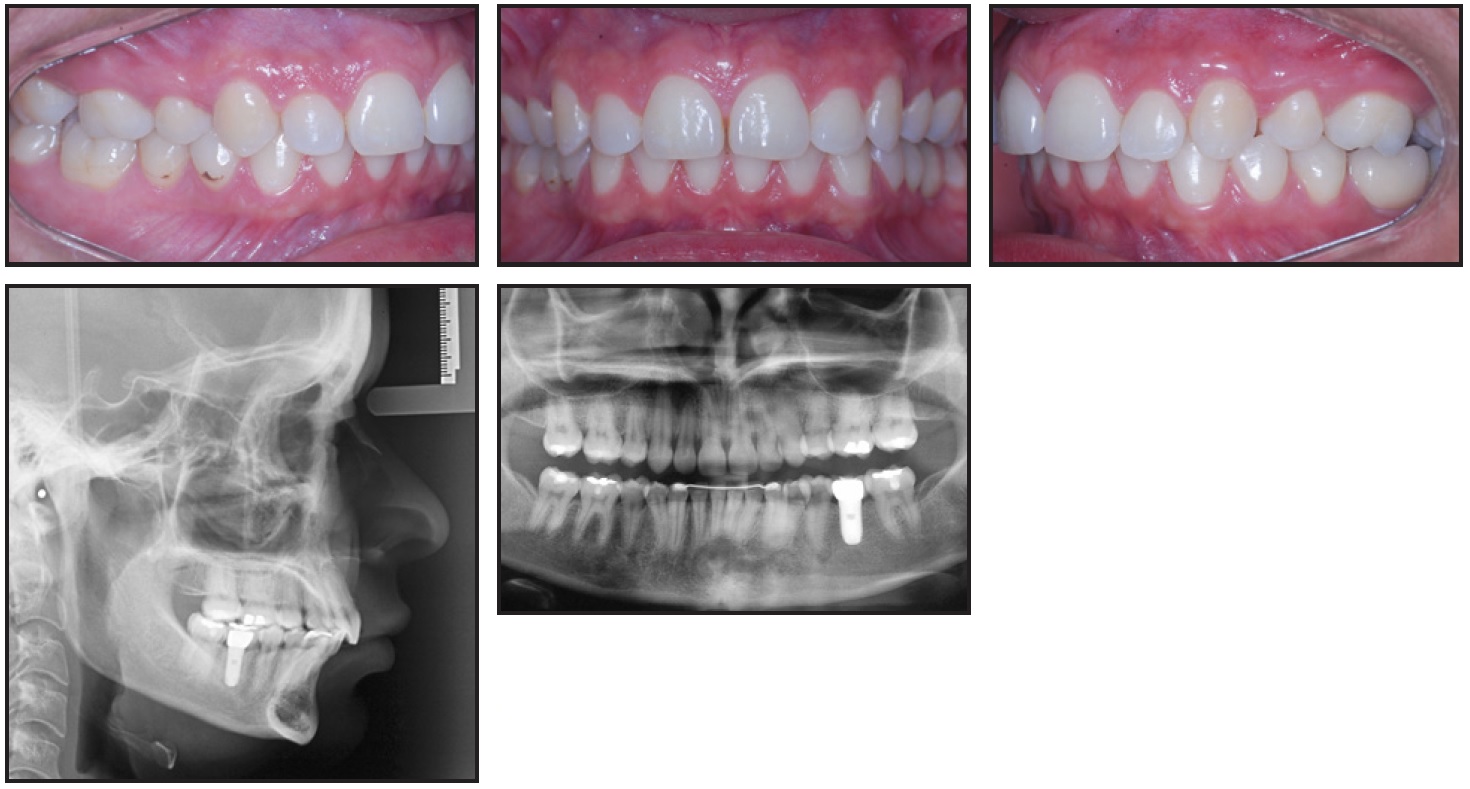
Fig. 6 Patient three years after treatment.
Discussion
Before deciding whether to perform compensatory orthodontic treatment, the clinician should conduct a detailed facial analysis.10 The comprehensive analysis developed by Arnett and colleagues, used for both orthodontic and surgical planning, includes 19 main facial traits in the frontal and profile views.11,12 The patient is examined in natural head position, with the condyles positioned in the articular fossae (centric relation) and the lips relaxed. Despite our patient's visible mandibular deficiency, as verified by the profile analysis, we agreed to proceed with compensatory treatment because the quantity of mental bone defining the contour of the chin-neck line significantly improved her prognosis.
Another aspect of the treatment plan discussed with the patient was the full-time wear of a splint to open the bite until the mandibular curve of Spee had been corrected. Many devices have been developed to prevent contact of the upper teeth with lower brackets in patients with deep overbite, including fixed mandibular activators, fixed or removable anterior biteplanes, and lingual appliances incorporating the biteplane in the brackets.13,14 In our patient, the objective of constructing a splint with simultaneous bilateral contacts was to provide greater comfort during mastication.
Considering possible protocols for treating a skeletal Class II malocclusion, Janson and colleagues verified that the extraction of two upper premolars provides better control of the vertical dimension compared to nonextraction treatment or the extraction of four premolars, because it does not require distalization of the upper molars and allows correction of the anteroposterior discrepancy between the arches.15 In such treatment, the upper anterior segment must be distalized by the width of a premolar (7mm), so that the canines move into a Class I relationship while the molars remain in Class II. To avoid any loss of maxillary posterior anchorage in the case shown here, we elected to use mini-implants as direct support for the anterior retraction. This kind of skeletal anchorage has been increasingly used in recent years for cases where insufficient dental anchorage is available, or simply to make treatment less complex and more predictable for the orthodontist without requiring special cooperation from the patient.8,9,16
FOOTNOTES
- *Morelli Ortodontia, Sorocaba, São Paulo, Brazil; www.morelli.com.br.
- **TP Orthodontics, Inc., La Porte, IN; www.tportho.com.
- ***Sin, São Paulo, Brazil; www.sinimplante.com.br.
- †Dentsply GAC, Islandia, NY; www.dentsply.com.
REFERENCES
- 1. Johal, A.; Alyaqoobi, I.; Patel, R.; and Cox, S.: The impact of orthodontic treatment on quality of life and self-esteem in adult patients, Eur. J. Orthod. 37:233-237, 2015.
- 2. Tai, K. and Park, J.H.: Orthodontic treatment of an adult patient with severe crowding and unilateral missing premolars, J. Clin. Orthod. 48:405-414, 2014.
- 3. Janson, G.; Janson, M.R.; Cruz, K.S.; Henriques, J.F.; and de Freitas, M.R.: Unusual orthodontic retreatment, Am. J. Orthod. 123:468-475, 2003.
- 4. Schmitz, D.: Adult orthodontic and TMJ retreatment with elastodontic appliance: An early progress report, Funct. Orthod. 7:35-40, 1990.
- 5. Choi, Y.J.; Lee, J.S.; Cha, J.Y.; and Park Y.C.: Total distalization of the maxillary arch in a patient with skeletal Class II malocclusion, Am. J. Orthod. 139:823-833, 2011.
- 6. Hunter, W.S.: The vertical dimensions of the face and skeletodental retrognathism, Am. J. Orthod. 53:586-595, 1967.
- 7. Janson, G.; Barros, S.E.; de Freitas, M.R.; Henriques, J.F.; and Pinzan, A.: Class II treatment efficiency in maxillary premolar extraction and nonextraction protocols, Am. J. Orthod. 132:490-498, 2007.
- 8. Kanomi, R.: Mini-implant for orthodontic anchorage, J. Clin. Orthod. 31:763-767, 1997.
- 9. Kuroda, S.; Sugawara, Y.; Deguchi, T.; Kyung, H.M.; and Takano-Yamamoto T.: Clinical use of miniscrew implants as orthodontic anchorage: Success rates and postoperative discomfort, Am. J. Orthod. 131:9-15, 2007.
- 10. Pithon, M.M.; dos Santos, R.L.; Sampaio, G.A.; de Meneses, I.H.; and Coqueiro, R.S.: Anteroposterior and vertical changes in skeletal class II patients treated with modified Thurow appliance, Braz. Dent. J. 25:170-174, 2014.
- 11. Arnett, G.W. and Bergman R.T.: Facial keys to orthodontic diagnosis and treatment planning, Part II, Am. J. Orthod. 103:395-411, 1993.
- 12. Arnett, G.W. and Bergman, R.T.: Facial keys to orthodontic diagnosis and treatment planning, Part I, Am. J. Orthod. 103:299-312, 1993.
- 13. Bergersen, E.O.: A longitudinal study of anterior vertical overbite from eight to twenty years of age, Angle. Orthod. 58:237-256, 1998.
- 14. Haegglund, P. and Segerdal, S.: The Swedish-style integrated Herbst appliance, J. Clin. Orthod. 31:378-390, 1997.
- 15. Janson, G.; Brambilla Ada, C.; Henriques, J.F.; de Freitas, M.R.; and Neves, L.S.: Class II treatment success rate in 2- and 4-premolar extraction protocols, Am. J. Orthod. 125:472-479, 2004.
- 16. Jeon, J.M.; Yu, H.S.; Baik, H.S.; and Lee, J.S.: En-masse distalization with miniscrew anchorage in Class II nonextraction treatment, J. Clin. Orthod. 40:472-476, 2006.



