An Appliance for Treatment of Anterior Crossbite in an Epileptic Patient
Malocclusion and other orofacial problems are more prevalent in children and adolescents with developmental disorders than in the general population, according to Waldman and colleagues.1 Patients with special needs frequently require alteration or customization of orthodontic procedures or appliances for reasons including safety, comfort, and compliance. For example, although removable appliances are normally used in cases requiring early orthodontic intervention, such as anterior crossbite,2 an alternative approach may be required if patient cooperation is a concern.
We were confronted with such a situation when a 13-year-old male presented at our clinic with the chief complaint that his “top teeth bite behind those at the bottom” (Fig. 1).
The patient’s medical history included frequent epileptic seizures with loss of consciousness. Clinically, he was in the mixed dentition, with a Class I malocclusion and anterior crossbite of the maxillary central and lateral incisors.
The patient and his family requested limited treatment of only the anterior crossbite, with the goal of providing esthetic and functional improvement. A treatment plan was initially proposed involving a removable plate with fingersprings, but because of the risk of the appliance becoming dislodged during a seizure and being swallowed or aspirated, a fixed appliance with fingersprings was designed.
Similar articles from the archive:

Fig. 1 13-year-old male patient with anterior crossbite of upper right central and lateral incisors before treatment. Patient suffered from frequent epileptic seizures.
Appliance Design and Fabrication
1. A length of .035" stainless steel wire was adapted to the palatal surface of the plaster cast, extending anteriorly from the first molars with a single loop at the incisive papilla. After the wire was secured to the cast with wax, the ends were welded to the first-molar bands (Fig. 2A).
2. Fingersprings were formed from .032" stainless steel wire, with helices incorporated for flexibility. Retention loops were bent into the distal ends for attachment to the main wire’s anterior loop (Fig. 2B).
3. After the fingersprings were adapted to the plaster cast (Fig. 2C), each spring was tied to the anterior loop with ligature wire (Fig. 2D). The fingersprings were blocked out on the cast (Fig. 2E), and the distal retention loops were then welded to the main wire (Fig. 2F).
4. The appliance was finished and polished in preparation for insertion (Fig. 2G).
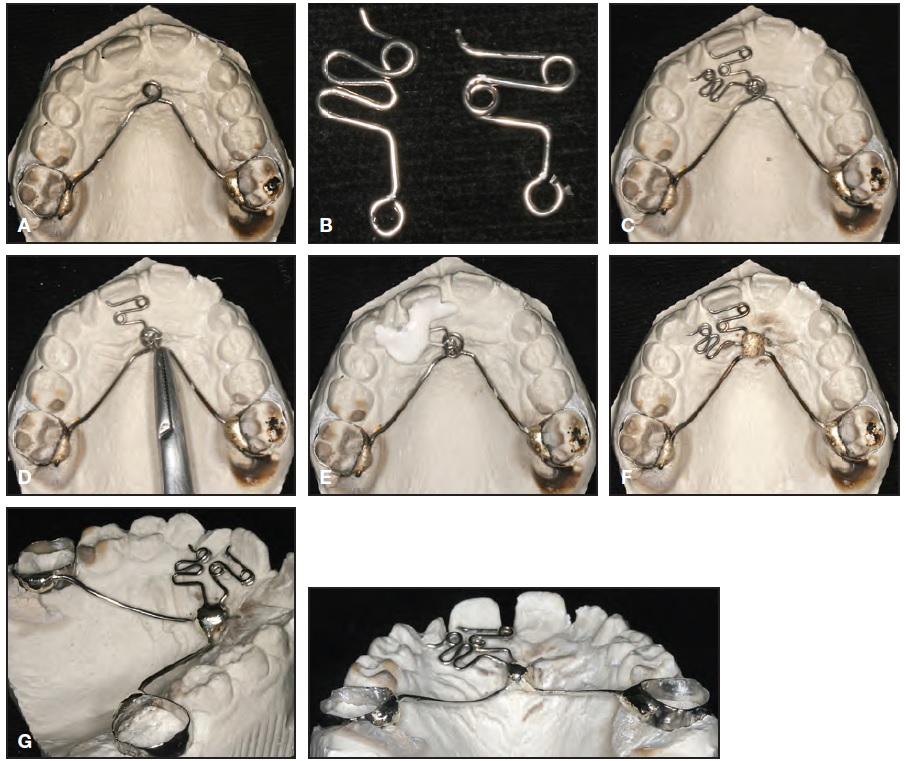
Fig. 2 Fabrication of appliance. A. .035" stainless steel wire adapted to palatal surface of cast, with anterior loop formed at incisive papilla. B. Fingersprings bent from .032" stainless steel wire. C. Springs adapted to plaster cast. D. Distal retention loop of each spring tied to main wire with ligature wire. E. Springs blocked out on cast. F. Springs welded to main wire. G. Appliance finished and polished.
5. The customized appliance was cemented to the maxillary molars, and the fingersprings were activated (Fig. 3).
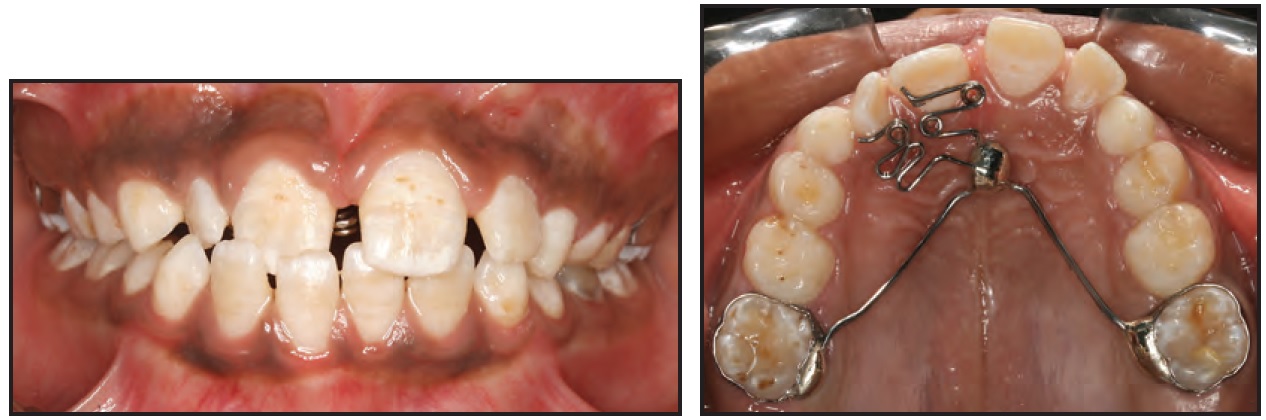
Fig. 3 Appliance cemented to maxillary first molars and activated.
The crossbite was corrected in only four weeks, but the appliance was left passively in place for another four weeks before removal (Fig. 4).

Fig. 4 Appliance removed after eight weeks, including four weeks of active treatment.
Discussion
Epilepsy is a chronic and potentially debilitating neurological condition affecting more than 50 million people worldwide.3 About 75% of cases have no identifiable cause, although there is a familial trend; the other 25% can be traced to brain damage from injury, infection, birth trauma, or cerebrovascular accidents.4 A majority of epileptic patients are able to control their symptoms using medication and to lead entirely normal lives, but about a third continue to suffer from seizures.5 A seizure occurs when a short, strong electrical surge lasting from a few seconds to a few minutes affects part or all of the brain. Symptoms vary from blank staring to jerking movements of the extremities to convulsions and loss of consciousness.3
In addition to an increased risk for dental caries and oral trauma, epileptic patients may also present with medication-induced gingival hyperplasia, bleeding gums, and delayed healing.6 When orthodontic treatment is required, non-removable appliances are vastly preferred; if a removable appliance must be used, it should be designed for maximum retention and fabricated from high-impact acrylic to lessen the risk of breakage during a seizure (which could leave sharp fragments in the oral cavity).3,7
An immediate esthetic improvement is especially important in enhancing a patient’s self-image in a child or adolescent suffering from epilepsy’s more debilitating and potentially embarrassing symptoms. In the case shown here, a fixed appliance was easily fabricated at low cost and was effective in a short period of treatment.
REFERENCES
- 1. Waldman, H.B.; Perlman, S.P.; and Swerdloff, M.: Orthodontics and the population with special needs, Am. J. Orthod. 118:14-17, 2000.
- 2. Franco, A.A.; D’Abreu, C.E.C.; Santana, F.F.; and Cevidanes, L.H.S.: Tratamento ortodôntico de mordida cruzada anterior no paciente adulto, Rev. Ortod. Soc. Paulista Ortod. 41:303-313, 2008.
- 3. Epilepsy Foundation website, www.epilepsyfoundation.org.
- 4. Patel, A.; Burden, D.J.; and Sandler, J.: Medical disorders and orthodontics, J. Orthod. 36:1-12, 2009.
- 5. American Epilepsy Society, 63rd Annual Scientific Conference, Boston, 2009.
- 6. Oral Health Fact Sheet for Dental Professionals: Children with Epilepsy, University of Washington School of Dentistry, Seattle, 2012.
- 7. Fiske, J. and Boyle, C.: Epilepsy and oral care, Dent. Update 29:180-187, 2002.



