Anterior Torque Correction with Bracketless Fixed Orthodontics
Torque correction is one of the most difficult and critical procedures performed during the finishing phase of orthodontic treatment.1 Proper torque positions the root in a physiological periodontal situation because it ensures both appropriate occlusal-force distribution and adequate thickness of the vestibular cortical plate. In a case where gingival recession is combined with significant torque abnormality, can torque correction also induce an improvement of the periodontal lesion? This article addresses that question with a periodontal application of a lingual beta titanium spring,2,3 using bracketless fixed orthodontics.3
Appliance Design and Activation
The torquing system consists of a round passive lingual retainer and an overlaid U-shaped spring. The passive retainer is bonded to the tooth requiring torque correction and to the adjacent anchorage tooth or teeth. Round wires ranging from .014" to .018" nickel titanium or a five-stranded .0175" stainless steel wire can be used for the retainer, with differing elasticity resulting in various degrees of crown movement. At the tooth requiring torque correction, a thin layer of orthodontic wax applied to the retainer before bonding will prevent adhesion between composite and wire, permitting the tooth to rotate around the retainer.
Similar articles from the archive:
The spring unit is fabricated from a segment of .016" x .022" beta titanium wire in a squared-U shape, with two vertical arms connected by a horizontal segment. The spring is preactivated by applying torsion to the connecting segment, forming an angle of 25-60° (depending on the amount of torque needed) between the two vertical arms.
The spring is bonded directly to the lingual surfaces using flowable composite resin. The first leg is bonded to an anchor tooth with the arm parallel to the tooth's long axis (Fig. 1), keeping the horizontal segment as parallel and close as possible to the underlying retainer. The second arm is then bonded after pressing it firmly against the lingual surface of the tooth to be torqued.
The spring should be reactivated every three to four weeks by removing the composite from only the tooth being torqued. The composite is first thinned down with an air-turbine diamond bur under irrigation, avoiding direct contact with the spring; the last layer of composite is broken and removed with a probe. Intraoral reactivation is performed by stabilizing the horizontal segment with a utility tool and simultaneously increasing the angle between the two vertical arms with a Weingart plier. The remaining composite is then roughened with a diamond bur, and the spring is rebonded to the tooth using liquid resin and flowable composite without etching.
Case Report
A 25-year-old male patient presented with vestibular root torque and Miller Class III gingival recession4 (Table 1) on both lower lateral incisors after seven years of fixed retention, following orthodontic treatment to correct a Class II malocclusion and mild mandibular crowding (Fig. 2).
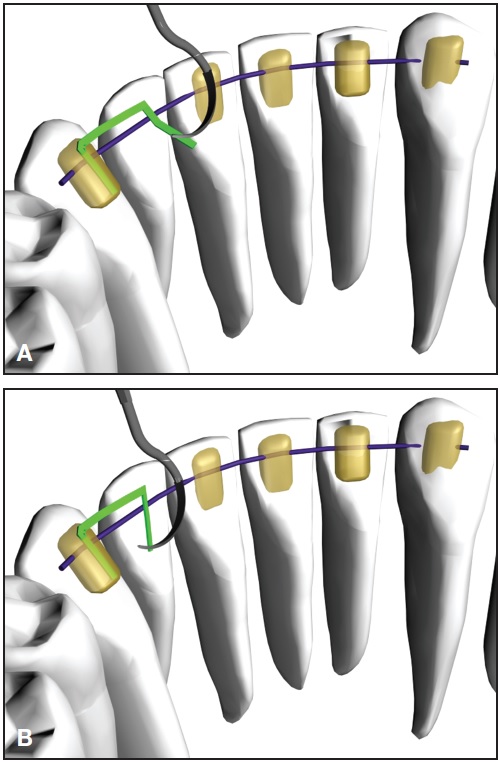
Fig. 1 A. After activation of torquing spring, first leg of spring bonded to anchor tooth adjacent to lateral incisor requiring torque correction. B. Second leg then pressed against lingual surface of lateral incisor for bonding.

Fig. 2 25-year-old male patient with altered vestibular root torque and Miller Class III gingival recession4 on both lower lateral incisors seven years after end of orthodontic treatment, showing five-stranded .0175" stainless steel upper and lower retainer wires still in place.
Upper and lower 3-3 passive lingual retainers made from five-stranded, braided .0175" stainless steel wire had been placed prior to debonding and were still intact.
The patient was referred to a periodontist for nonsurgical treatment and evaluation of local etiological factors. No systemic metabolic alterations or outside factors could be correlated with the patient's periodontal status. A bracketless torquing spring was prepared as described above. A round .018" Nitinol* wire, adjusted to the patient's archform, was bonded from canine to canine to act as a hinge axis during the lateral incisor torquing and to limit buccal displacement of the incisor crowns (Fig. 3). Two .016" x .022" beta titanium torquing springs, each activated about 30°, were bonded between the lower lateral incisors and canines.
To limit reciprocal torquing movements of the two canines, passive .017" x .025" stainless steel wire splints were bonded to the buccal surfaces of the lower canines and first and second premolars (Fig. 4).

Fig. 3 .018" round Nitinol lingual wire adjusted passively to patient’s lower archform and bonded from canine to canine; two torquing springs bonded between right and left canines and lateral incisors to initiate correction of lateral incisor root positions.

Fig. 4 Passive bilateral .017" × .025" stainless steel splints bonded to buccal surfaces from lower canines to second premolars to limit reciprocal torquing movement of canines.
After three months of active treatment and three reactivations, lingual root repositioning of the lateral incisors was achieved (Fig. 5).
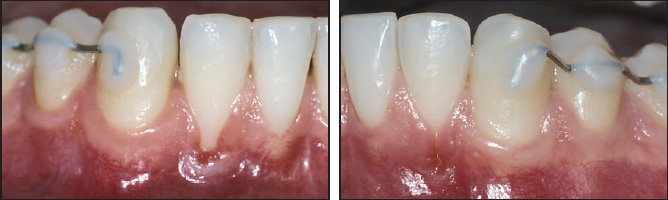
Fig. 5 Lingual repositioning of lateral incisor roots after three months of active treatment.
No appreciable side effects on the canine positions were noted, and there was no sign of gingival inflammation. The clinical appearance of gingival recession had improved, although the heights of the epithelial attachments were unchanged. The bracketless technique allowed for careful control of oral hygiene during treatment; the patient was highly cooperative and happy to be treated without labial appliances.
After a new retainer wire was bonded, the patient was referred for periodontal reevaluation, but decided not to undergo mucogingival surgery. One-year follow-up records showed further spontaneous improvement of the gingival recession (Fig. 6).

Fig. 6 Patient one year after treatment, showing further spontaneous improvement of gingival recession.
Discussion
With more social awareness of the appearance of anterior teeth, especially among adults, esthetic tooth-movement procedures continue to gain in popularity. Our bracketless torquing technique is well accepted by patients needing limited treatment and requires no special compliance.
Another point in its favor is the reduced risk of white-spot lesions--which are significantly more likely to develop on the facial and buccal surfaces than on the lingual surfaces.5-7
The .016" x .022" beta titanium wire's load/deflection ratio has proven appropriate for the torquing spring's shape and size, providing satisfactory control of tooth movement and forces that are safe and biologically compatible with periodontal tissues. The passive nickel titanium retainer wire allows better control of crown movements by shifting the center of rotation occlusally.
Because the activation of the torquing spring results in mutual torque between two adjacent teeth, a passive anchorage unit must be applied unless the neighboring tooth requires an inverse correction. In the case shown here, the two bonded buccal splints controlled the canine positions, so that the torque correction was exerted mainly on the lateral incisors. The lingual root movement of the lateral incisors improved the patient's gingival health and changed the vestibular architecture, thus reducing the potential for further recession. After treatment, the patient's gingival recessions could be reclassified as Miller Class II, and his periodontal prognosis could be considered more favorable,4,8 even though he declined further periodontal treatment.
Tissue grafts are recommended in orthodontic patients with gingival recession to increase the amount of gingival tissue at the margins of the lesions and thus enhance tissue resistance to orthodontic forces.9 Careful planning of orthodontic movements and the use of biomechanically compatible devices and forces may require interdisciplinary cooperation.10,11 In the case shown here, the beneficial root movements resulted in increased thickness of gingival tissues at the margins of the recessions12--a prerequisite for adequate trophism of a periodontal tissue graft.13
Based on Miller's diagnostic and prognostic evaluation,4 we suggest that appropriate orthodontic treatment may improve the prognosis of subsequent mucogingival surgery.
Although our patient's spontaneous improvement one year after orthodontic treatment cannot be considered predictive, it encourages further investigation. New insights are needed into this approach to the treatment of gingival recessions.
FOOTNOTES
- *3M Unitek, Monrovia, CA; www.3mUnitek.com.
REFERENCES
- 1. Yang-Powers, L.C.; Sadowsky, C.; Rosenstein, S.; and BeGole, E.A.: Treatment outcome in a graduate orthodontic clinic using the American Board of Orthodontics grading system, Am. J. Orthod. 122:451-455, 2002.
- 2. Fiorelli, G. and Melsen, B.: Biomechanics in Orthodontics CD-ROM, release 3.0, Libra Ortodonzia Ed., Arezzo, Italy, 2008.
- 3. Musilli, M.: Bracketless fixed orthodontics: Nine years of clinical experimentation, Prog. Orthod. 9:72-91, 2008.
- 4. Miller, P.D.: A classification of marginal tissue recession, Int. J. Period. Restor. Dent. 5:9-13, 1985.
- 5. Lucchese, A. and Storti, E.: Morphological characteristics of primary enamel surfaces versus permanent enamel surfaces: SEM digital analysis, Eur. J. Paediat. Dent. 12:179-183, 2011.
- 6. Lucchese, A.; Bertacci, A.; Chersoni, S.; and Portelli, M.: Primary enamel permeability: A SEM evaluation in vivo, Eur. J. Paediat. Dent. 13:231-235, 2012.
- 7. Lucchese, A. and Gherlone, E.: Prevalence of white-spot lesions before and during orthodontic treatment with fixed appliances, Eur. J. Orthod., in press.
- 8. Hamdan, A.; Nadir, B.; and Anil, S.: Surgical management of gingival recession: A clinical update, Saud. Dent. J. 21:83-94, 2009.
- 9. Wennstrom, J. and Pini Prato, G.P.: Mucogingival therapy, in Clinical Periodontology and Implant Dentistry, 3rd ed., ed. J. Lindhe, Munksgaard, Copenhagen, 1998, pp. 550-596.
- 10. Boyd, R.L.; Leggott, P.J.; Quinn, R.S.; Eakle, W.S.; and Chambers, D.: Periodontal implications of orthodontic treatment in adults with reduced or normal periodontal tissues versus those of adolescents, Am. J. Orthod. 96:191-199, 1989.
- 11. Lucchese, A.; Porcù, F.; and Dolci, F.: Effects of various stripping techniques on surface enamel, J. Clin. Orthod. 35:691-695, 2001.
- 12. Tugnait, A. and Clerehugh, V.: Gingival recession--its significance and management, J. Dent. 29:381-394, 2001.
- 13. Zachrisson, B.U.: Clinical implications of recent orthodonticperiodontic research findings, Semin. Orthod. 2:4-12, 1996.





