MASTER CLINICIAN
R.G. "Wick" Alexander, DDS, MSD
(Editor's Note: Associate Editor Peter Sinclair conceived this department devoted to recognizing the Master Clinicians who have made the orthodontic specialty what it is today. Every few months in JCO, he will delve into the career story and treatment principles of one of these seminal figures. We welcome your nominees for future Master Clinicians.)
Effort = Results. This is the axiom that Wick Alexander has used to achieve success in four different aspects of orthodontics. As a clinician, he has developed techniques that have led to consistently high-quality treatment results. As an author, he has introduced an innovative, comprehensive treatment approach that many clinicians have found extremely effective. As a researcher, he has been at the forefront of the scientific evaluation of orthodontic treatment outcomes and stability. As an educator, he has been responsible for training hundreds, if not thousands, of residents and clinicians throughout the United States and the world.
In each area, he has led the way and set the standard for others to follow. Wick Alexander is indisputably an orthodontist from whom we can all learn, and we are pleased that he has agreed to share his philosophy with JCO in this first installment of the Master Clinician series.
PETER M. SINCLAIR, DDS, MSD
Similar articles from the archive:
- MASTER CLINICIAN Bjorn U. Zachrisson, DDS, MSD, PHD September 2012
- MASTER CLINICIAN Richard P. McLaughlin, DDS January 2013
- MASTER CLINICIAN Birte Melsen, DDS, DO October 2013
DR. SINCLAIR Who were your mentors?
DR. ALEXANDER My first mentor was my older brother Moody. Being four years older, he guided me everywhere during those early years. From high school to dental school, then the University of Texas Orthodontic Department in Houston, he always challenged and encouraged me to do better than he had done. He will always be my inspiration!
Other mentors included A.P. Westfall, chair of the University of Texas Orthodontic Department, who made my orthodontic career possible. A quiet, fatherly gentleman, he wanted his students to be exposed to the latest in orthodontics. During my two years in the department, he brought to the school Charles Tweed, the Holdaway Study Group, Fred Schudy, John Lindquist, Morris Stoner, Tod Dewel, Joseph Jarabak, Raleigh Williams, Jim Reynolds, Jay Barnett, Bob Ricketts, and others. It was like a group of superstars in orthodontics. We took the Tweed typodont course twice in school, taught by Col. George Bowden, who also taught in Tucson. Our patients were treated like typodonts.
You may recall that first-bicuspid-extraction cases were dominant in the 1960s. During this time, my wife Janna was being treated orthodontically by Fred Schudy. Ahead of his time, he extracted second premolars. Things I learned from Dr. Schudy included attention to facial profiles, centric relation equals centric occlusion, .018" slots, and nonextraction treatment. To this day, I consider him to be the best orthodontist in our history.
Another life-changing experience occurred when Dr. Westfall asked me to talk with my wife, who was a physical therapist working in the hospital, to arrange a tour of the new Texas Institute for Rehabilitation and Research, across the street from the dental school. Little did we know that it was the same time that the scoliosis patients were being treated. We walked into the room and saw all those patients wearing the Milwaukee braces. Dr. Westfall, observing their teeth, said, "Wick, here is your thesis subject." Eventually, this thesis won the 1965 AAO Milo Hellman Research Award. It would have never happened if we had visited on another day or another time!
After I had been in practice one year in Arlington, Bob Gaylord, Chairman of the Baylor Orthodontic Department in Dallas, asked me to continue my research at the Scottish Rite Hospital in Dallas. Dr. Gaylord then invited me to join the staff at Baylor, opening a new door of teaching, research, and lecturing. This motivated me to take and preserve the diagnostic records on all of our patients--now known as the Room of Truth.
Mentors can enter one's life under a myriad of circumstances. My first real lecture came when I was asked to speak to the Texas Tweed Orthodontic group in Fort Worth. The "headliner" was John Lindquist, a well-known and excellent educator. He attended my lecture on practice management and was impressed to the point that he later told Gene Gottlieb, Editor of JCO, about my presentation. Shortly thereafter, Gene called me and inquired about the possibility of publishing my presentation. Although completely thrilled, I reluctantly told him I had no manuscript--only some notes, several carousels of 35mm slides, and an amateurish tape recording. Undaunted, Gene asked me to send everything I had for him to review. After several weeks, he sent me manuscripts, outlines, and suggestions that eventually made my lecture publishable. "Practical Points to Practice Efficiency" was published by JCO in a series of four articles in 1975. Gene used a slide of me adjusting an archwire on the first cover. The exposure I received from that series of articles opened the door to a lifetime of lecturing.
DR. SINCLAIR What is your overall philosophy, and how does it guide you?
DR. ALEXANDER My philosophy can be divided into two doctrines. I attempt to live by the "I am third" philosophy: God, others, then me. This creed keeps me grounded, keeps my priorities in check, and helps me realize how blessed I am to have had so many opportunities.
I also created a formula from James Allen's book, As a Man Thinketh: "In all human affairs there are efforts and there are results, and the strength of the effort is the measure of the results." Effort = Results. Every day in my practice, I try to teach this to our patients. Every day as a parent, I share this concept with my children and grandchildren. Every day as a teacher, I try to give it my best. Every day as a friend, I want to be supportive. Every day that I am blessed to be on this earth, I want to leave no stone unturned. My efforts help determine the results.
DR. SINCLAIR What are your orthodontic treatment principles?
DR. ALEXANDER My principles are all contained in my book, 20 Principles of the Alexander Discipline (Quintessence, 2008). Today, I still believe in so many things that I was taught in graduate school: IMPA control, intercanine width control, uprighting mandibular first molars. But in school, all of our patients were treated with .022" slots using the Tweed technique. I clearly remember attempting to insert an .021" × .025" stainless steel archwire on a maxillary second molar. As I struggled along, I saw tears run down the patient's face. I immediately thought to myself, "I am not going to do this for the rest of my life."
Around that time, there was a popular uprising of .018" slots with single brackets and tie wings, led by West Coast orthodontists such as Cecil Steiner, Howard Lang, and Paul D. Lewis. Working with one of my classmates, Robert Orr, I came up with a mixture of brackets and decided to use .018" slots. That was the birth of the "Vari-Simplex Discipline". Of course, it was before bonding, so each tooth had a band with the bracket spot-welded to it. I initially worked with three orthodontic manufacturing companies, then finally settled in with one company to produce our system.
During the same period, Larry Andrews made a revolutionary change in bracket design when he moved the torque from the archwire to the bracket. This enabled me to place -5º torque in the mandibular incisor brackets--a major key to eventual long-term stability (LTS) by controlling IMPA, as taught by Dr. Tweed.
Another influence from the Tweed technique was to place mandibular first-molar brackets with -6º angulation (tipback). I did this with my initial order and have used it throughout my career. Several studies have shown that this "uprighting" is maintained over the long term--a positive factor in LTS.
The philosophy of "begin with the end in mind" is good--if we can define "the end". It should be the same for all clinicians, regardless of the bracket system or philosophy of treatment. In my experience, the ideal finished case should demonstrate the following:
Dental
• IMPA--the 3º rule (finish within 3º of the original position in nonextraction patients). Exceptions: Class II, division 2 cases can be flared significantly; extraction cases should be uprighted as needed; bimaxillary protrusion cases can be uprighted significantly.
• Mandibular intercanine width--finish within 1mm of the original positions. Exception: when canines erupt lingually.
• Anterior root positioning--the mandibular lateral incisors need to be nearly parallel to the mandibular canines to be stable.
• Ovoid archform in every patient.
Skeletal
• Sagittal--ANB ± 2º.
• Vertical--maintain the original position.
• Transverse--34-38mm of maxillary intermolar width.
During the first few years of my practice, the majority of my patients were treated with extractions, and I was active in the Tweed Foundation. At one meeting, I was criticized for bringing nonextraction cases and was told never to do that again. As I drove home from that meeting, I can clearly remember it was like the umbilical cord had been cut, and I was free to be independent and become my own person.
My concern today is that every technique has its own rules. Is orthodontics an art or a science? If our specialty is ever going to progress, we all need to agree on our goals and priorities. For more than 100 years, our profession has swung back and forth like a pendulum, moving from nonextraction to extraction and back to nonextraction. My belief is that the best way we can come to agree on goals is to focus on long-term stability. And remember, in some cases it is OK to extract teeth! Studies show that extraction of permanent teeth in selected situations is viable, stable, and cosmetically pleasing.
DR. SINCLAIR What are the requirements to become a successful clinician?
DR. ALEXANDER Being a successful clinician depends upon your definition of "success". I believe that success is revealed through a combination of clinical and interpersonal achievements. First, one should produce the highest-quality results possible. This can be achieved by "beginning with the end in mind". Clinical knowledge is acquired through education, skill, manual dexterity, experience, self-examination, and the development of a technique that masters the problems faced in clinical orthodontics. Most important is the pursuit of excellence--knowing that you are giving your best even when no one else will ever know.
To be successful, one must also develop the ability to lead others--staff, patients, parents, doctors--to perform and master their responsibilities. This is done by demonstrating a passion for orthodontics that resonates in the clinic. Although an orthodontic practice can generate a substantial income, and enjoyment comes from the monetary rewards of the profession, it should not be one's first priority.
A beautifully treated patient satisfies our needs and is always the best referral source. We have a prescription that, if followed, can consistently produce excellent esthetic, functional, and stable results. Over the years, I have demonstrated these results by allowing more than 50 graduate students to examine and study our diagnostic records of 15,000 patients.
DR. SINCLAIR What diagnostic principles do you follow?
DR. ALEXANDER When diagnosing a case, the most critical factor is potential growth. With the exception of a Class III skeletal problem, if facial growth is harnessed properly, it can be our best friend--especially in the maxilla!
In the transverse dimension, the maxillary skeleton can be permanently altered with rapid palatal expansion, cervical facebows, and expanded archwires; in the anteroposterior dimension, we can inhibit maxillary horizontal growth with facebows and functional appliances. Dentoalveolar changes can be made by intrusion, extrusion, expansion, or constriction.
Although others may differ, I do not believe we can grow mandibles. All we can do is watch them grow. And that's OK! We must be aware of our limitations.
The Tetragon Plus cephalometric analysis is a condensed version of the most important measurements needed to diagnose the patient's skeletal pattern. A cephalogram provides the four angles of the Tetragon--SN-MP (vertical skeletal pattern), U1-L1, and IMPA and U1-SN (anterior torque positions)--along with ANB and the soft-tissue profile (Fig. 1).
In observing the study models, we need to look at the arch-length discrepancy, mandibular intercanine and maxillary intermolar widths, posterior occlusion, overbite, overjet, and Angle classification. As I study these numbers, I am thinking, "Can I treat this patient nonextraction without violating the 'rules'?" The panoramic x-ray will identify deciduous and permanent teeth; bone levels; root apices; impacted, missing or extra teeth; and, of course, third molars. Facial photos can tell us about symmetry, soft-tissue profile, and the smile line. We list all of these issues on a diagnostic chart or screen, along with the treatment plan and financial considerations.
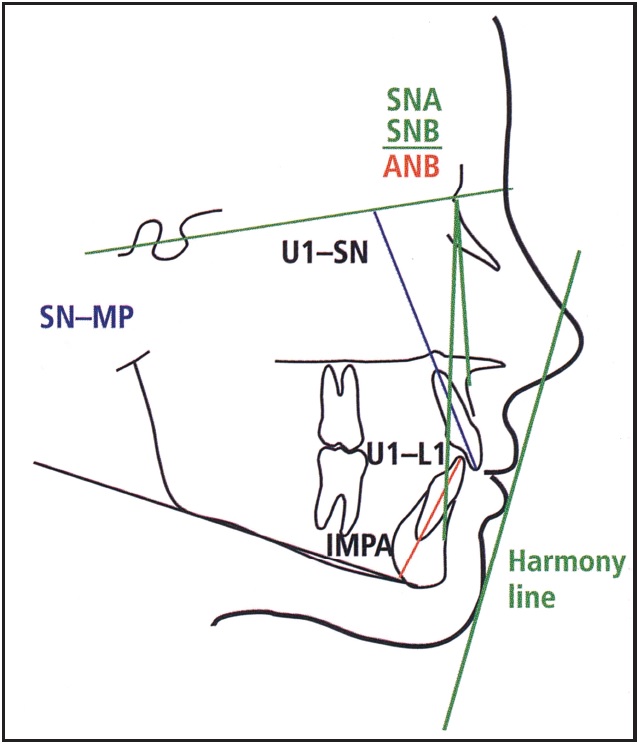
Fig. 1 Tetragon Plus cephalometric analysis. (Reprinted with permission from The 20 Principles of the Alexander Discipline, Quintessence, Hanover Park, IL, 2008.)
DR. SINCLAIR When do you initiate treatment?
DR. ALEXANDER Timing of orthopedic correction is critical, yet as a science, we have not been able to accurately determine when the patient will grow. I hope that someday we will be able to use a saliva test to determine when to expect a growth spurt. For now, I rely on the patient's maturity, the mother's observations, etc. Generally speaking, females grow earlier (10-12 years old); boys grow later (12-15 years old). But every case is unique, so detailed observations--including dental age, menarche, facial hair, and size in comparison to the parent--can be very helpful in anticipating growth.
Dentally, the ideal time to begin treatment is when the patient has lost all deciduous teeth except the mandibular Es. This allows the use of "E" space in borderline cases. (If the other permanent teeth have not erupted, a lingual arch may be indicated.) Also, the mandibular second molars should not be too far away from eruption. The patient is growing at this time, too.
One of the biggest mistakes we all have made is to initiate treatment earlier than necessary! But do not delay too long and take a chance of missing the patient's growth spurt.
DR. SINCLAIR How would you describe your typical treatment technique?
DR. ALEXANDER Although exceptions are always possible when dealing with human beings, for the vast majority of our patients, a simple treatment plan will be successful. We call it the KISS Principle: Keep It Simple, Stupid!
We seldom use sectional or utility archwires. We try to accomplish our mechanics one step at a time. The sequence of treatment is simple, straightforward, and very predictable. Minor changes or adjustments will be needed to address the needs of the specific patient.
If the maxilla is the "controllable" jaw, it makes sense to initiate treatment on that jaw. In Class I and II skeletal patterns, we can develop the maxillary arch to fit the untreated mandibular arch, both orthodontically and orthopedically, which is helpful for LTS. Early in treatment, we develop orthopedic forces using a cervical facebow worn eight hours daily (Class II normal angle), a combi or high-pull headgear (Class II high angle), or a facemask (Class III).
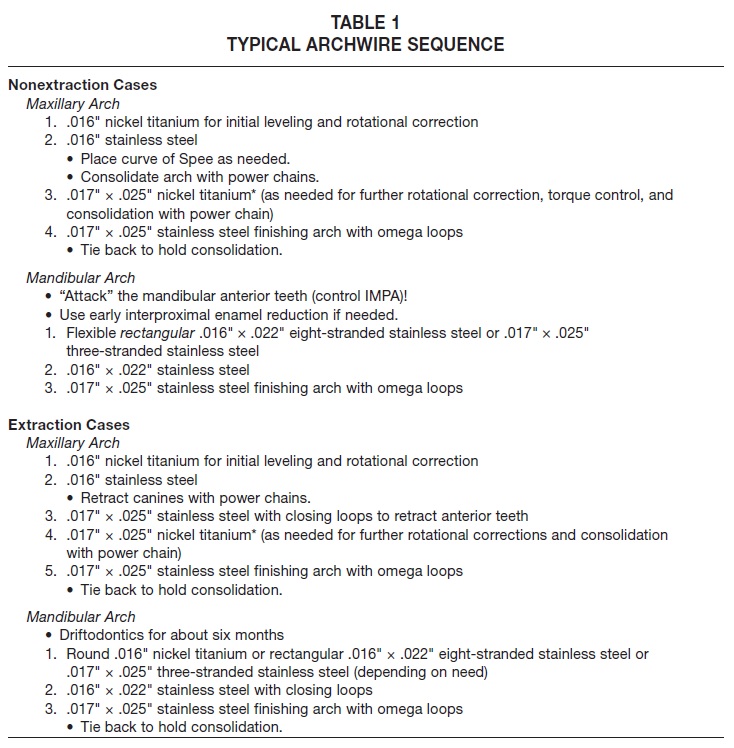
Brackets with .018" slots use smaller archwires, but gain superior torque control because the slot is filled. Single brackets provide additional interbracket space, enabling earlier engagement with rectangular archwires (Table 1). Tie wings facilitate rotational control. The goal is to get into the finishing archwire quickly and "let it cook!"
Bracket prescriptions should have angulations designed to spread the maxillary and mandibular anterior roots. In nonextraction cases, we focus on controlling mandibular incisor torque with the initial archwire (-5º torque). Upright mandibular first molars (-6º tip) improve LTS (except in open-bite cases). We routinely band the mandibular second molars.
In coordinating the arches, we aim for a specific ovoid archform (Fig. 2*). How is the mandibular archform selected? It's really very simple, based on the original intercanine width, upright mandibular incisors, and expanded premolars and molars to fit the maxillary premolars and molars (our long-term studies have shown that expanded premolars and molars can be stable).
After the patient is in finishing archwires, we use "zigzag" elastics designed for the malocclusion (Fig. 3).
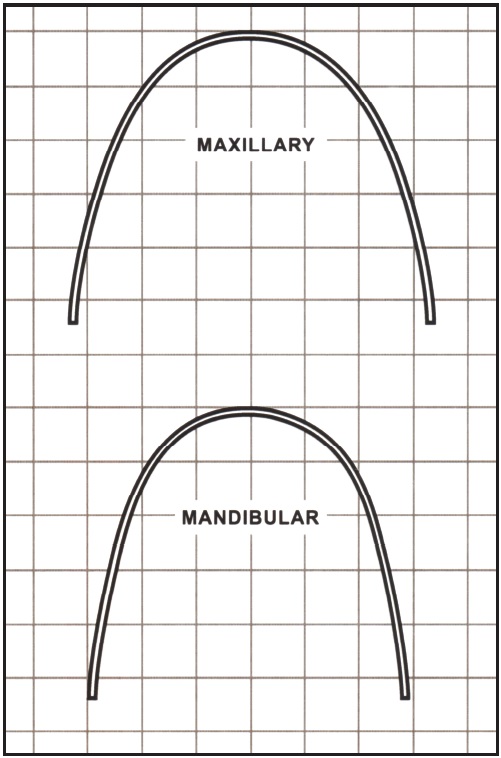
Fig. 2 Ovoid archforms.*
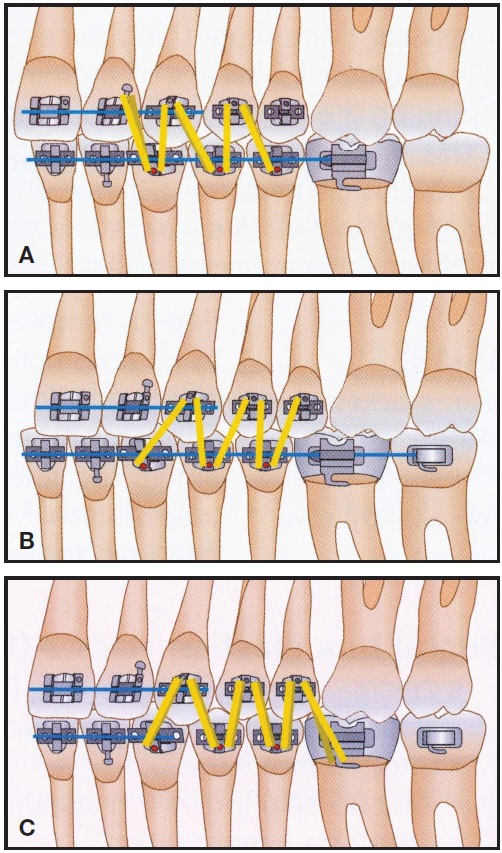
Fig. 3 Zigzag elastics. A. “W” with a tail (Class II). B. “M” with a tail (Class III). C. Finishing (Class I). (Reprinted with permission from The 20 Principles of the Alexander Discipline, Quintessence, Hanover Park, IL, 2008.)
Our retention protocol is simple, using a maxillary wraparound removable retainer (worn at night only) and a mandibular bonded 3-3 lingual retainer (.0215" multistranded wire).
Bottom line: Focus on the mandibular anterior teeth, and build the rest of the arches and occlusion around them for long-term stability.
DR. SINCLAIR Are there any other clinical tips you'd like to mention?
DR. ALEXANDER Heat-treat all stainless steel archwires. Polish the ends of the archwires for easier tube engagement. Learn proper ligation with a ligature-tying plier.
When in doubt, tie back! With omega loops placed 1mm anterior to the maxillary and mandibular molar tubes, tying back consolidates the arch and holds the teeth together, preventing spaces from opening during elastic wear. It also eliminates the need for "lacing" the teeth--very im-portant! Tying back in the maxillary arch changes the facebow from a "distalizing" appliance to an "orthopedic" appliance.
Surround yourself with staff and associates who can do it as well as you. Superior training of clinical staff will allow delegating without compromising. In our practice, the doctor prepares archwires for specific procedures (curve of Spee, torque, archform), but we teach the assistants to bend omega loops.
"We are only as good as our patients." Take time to learn how to motivate the patients!
Educate patients on oral hygiene, facebow use, and elastic wear. Communicate constantly with patients and parents.
DR. SINCLAIR What are your greatest clinical challenges?
DR. ALEXANDER Attempting to treat an adult surgical case nonsurgically has been my greatest clinical challenge. Skeletal growth allows us to be more adventuresome. Lack of growth reduces our ability to alter the facial bones nonsurgically.
Another difficult situation is a case with impacted maxillary canines. We try to expose them as quickly as possible to move them into the arch.
A severe clinical challenge is to treat patients who do not have a "full deck of cards" (missing permanent teeth). We always communicate with the patient and parents, but the best choice is usually to close space. Long-term stability is good in these patients, as the following case demonstrates.
Case 1
A 26-year-old male presented with several severe problems (Fig. 4). Both maxillary lateral incisors, the maxillary right second premolar, and both mandibular second premolars were congenitally missing. The deciduous second molars were still present on the maxillary right side and in both mandibular "E" spaces. The molars were Class I on the right side but Class II on the left; anterior overbite was 5mm.
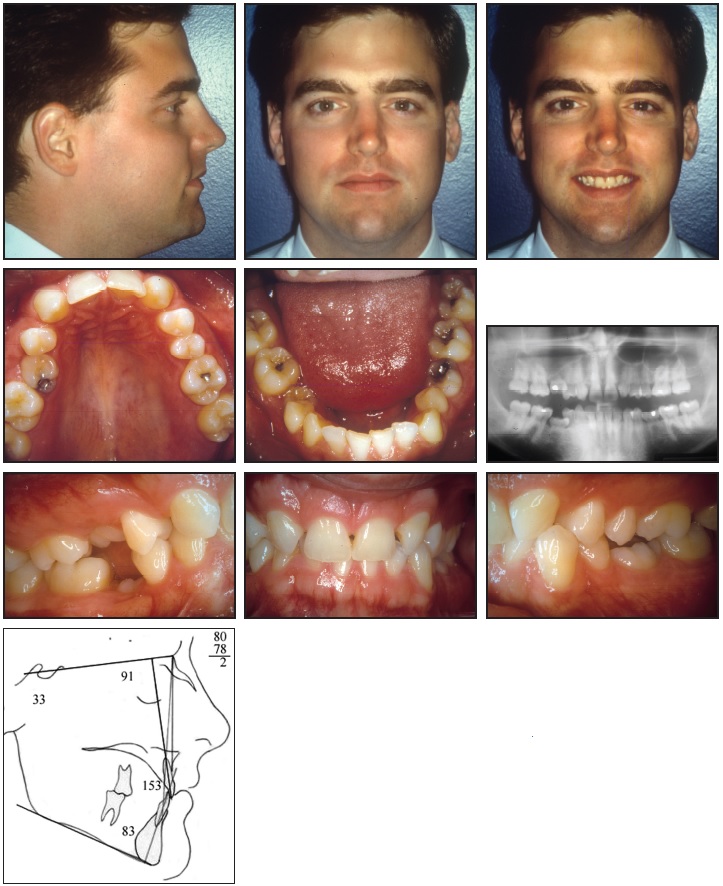
Fig. 4 Case 1. 26-year-old male patient with congenitally missing maxillary lateral incisors, maxillary right second premolar, and mandibular second premolars before treatment.
The big question was whether to open or close spaces. We made our decisions based on the spaces available in the areas of missing teeth. In the maxillary anterior region, the plan was to close spaces by substituting the canines for the missing lateral incisors (Fig. 5), using special bracket positioning (Fig. 6). The space for the maxillary right premolar was large enough to place an implant or a bridge, so the treatment plan there was to keep the space open. Because the mandibular right "E" space was partially closed, we decided to close the remaining space. The large mandibular left "E" space would be maintained.
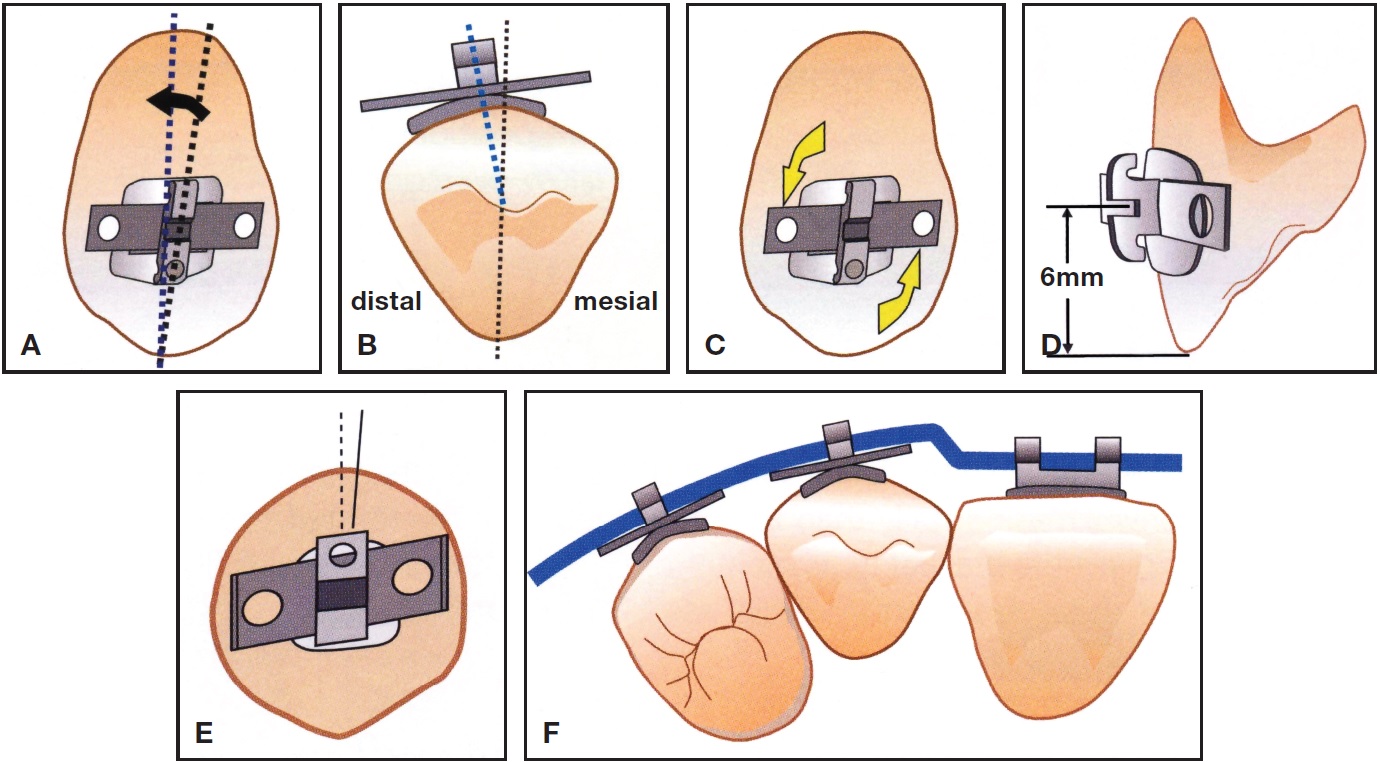
Fig. 5 Substitution of maxillary canines for missing lateral incisors. A. Inverted canine bracket with reduced angulation of 3-4° (arrow). B. Mesiodistal bracket placement on canine. C. Inverted canine bracket with +3° torque. D. Canine bracket height. E. Canine bracket on first premolar. F. Compensating wire bend for canine substitution. (Reprinted with permission from The 20 Principles of the Alexander Discipline, Quintessence, Hanover Park, IL, 2008.)
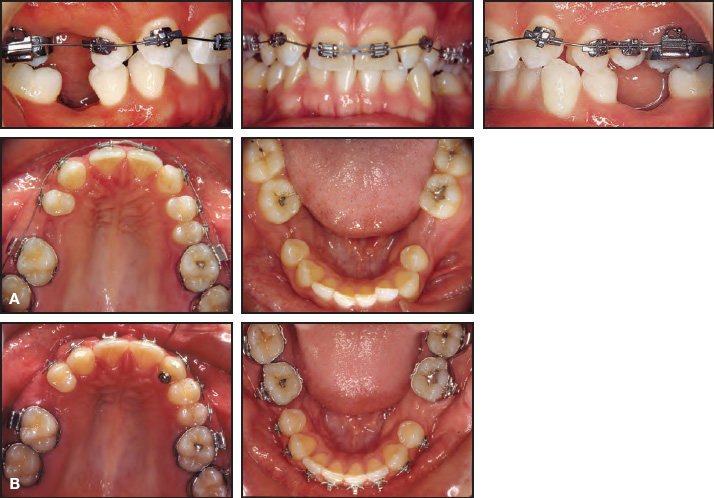
Fig. 6 Case 1. A. After two months of treatment, unique bracket placement on maxillary canines with initial .016" nickel titanium maxillary archwire. B. After 22 months of treatment, both arches ready for implants.
Treatment time (35 months) was extended because of delays in insurance coverage for the implant surgery (Fig. 7). The full crowns were mistakenly placed on the wrong teeth (implants), but have had no negative consequences.
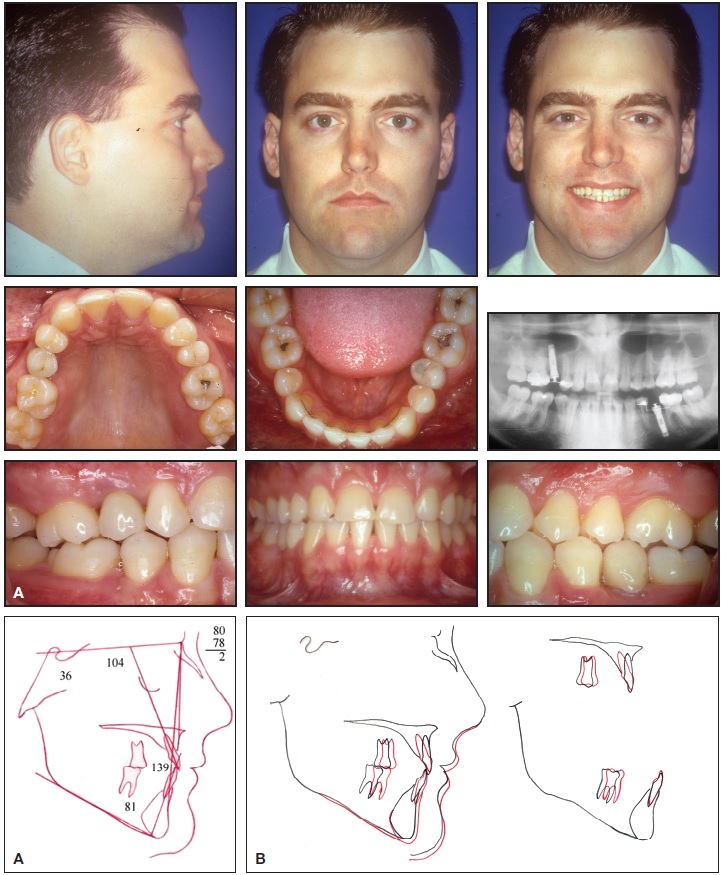
Fig. 7 Case 1. A. Patient after 35 months of treatment. B. Superimposition of cephalometric tracings before and after treatment.
Eighteen years after treatment, the patient continues to show healthy, functional, and stable results (Fig. 8). If he wanted to go to Hollywood, he could always have veneers placed on the maxillary anterior teeth. My belief is that veneers on large-rooted canines are much better than implants with all their potential problems.

Fig. 8 Case 1. Patient 18 years after treatment.
Case 2
Open-bite cases are another clinical challenge. A 21-year-old female presented with a highangle skeletal pattern (SN-MP = 48º) and Class I open-bite malocclusion (Fig. 9). She refused surgery, and because of her soft-tissue bimaxillary protrusion, the decision was made to extract four first premolars and four third molars.
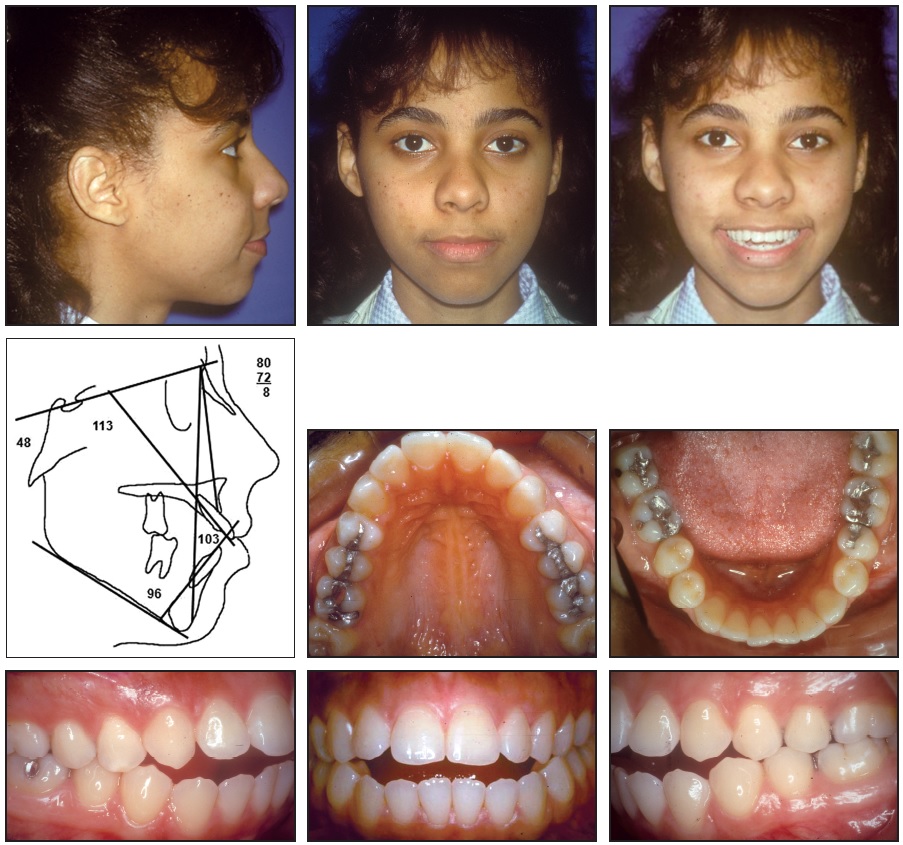
Fig. 9 Case 2. 21-year-old female patient with high-angle skeletal pattern and Class I open-bite malocclusion before treatment.
Full fixed appliances were placed at the beginning of treatment, and a high-pull facebow was worn at night. The patient was taught tongue-therapy exercises, which she practiced regularly.
To retract the mandibular anterior teeth, when the .016" x .022" stainless steel closing-loop archwire was activated (Fig. 10), the patient wore Class III elastics with the high-pull facebow.

Fig. 10 Case 2. Maxillary stainless steel closing-loop archwire and mandibular .016" × .022" stainless steel closing-loop archwire after 11 months of treatment.
This accentuated the curve of Spee by retracting and extruding the mandibular incisors. The maxillary arch was treated in the usual manner by first retracting the canines, then the four incisors. The big difference from normal or deep-bite cases was that the curve of Spee was reduced and the closing loops overactivated. This has the effect of tipping and extruding the incisors and closing the open bite; I call it "sloppy mechanics". It also makes a nice improvement in the smile line, showing more of the maxillary anterior clinical crowns. Appropriate elastics (Class II, buccal box, and finishing) were used throughout this case.
Treatment time was a reasonable 25 months (Fig. 11). Observing the profile change caused by retraction of the anterior teeth, one might wonder if surgery would have substantially improved the patient's appearance.
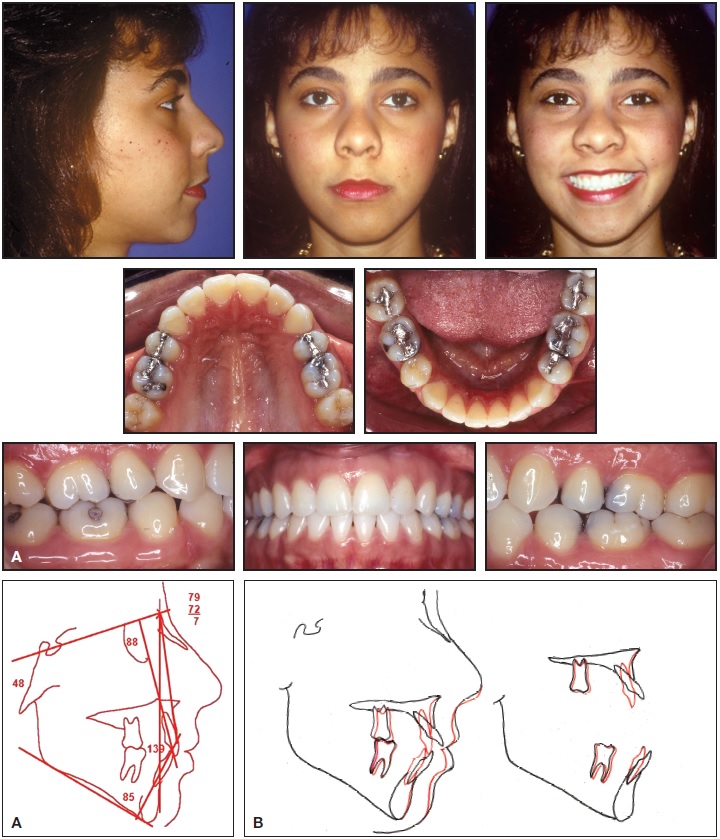
Fig. 11 Case 2. A. Patient after 25 months of treatment. B. Superimposition of cephalometric tracings before and after treatment.
One of the greatest hazards in treating open-bite malocclusions is the tendency for the anterior bite to relapse. The secret to stability is the patient's ability to swallow properly and continue squeezing. We also recommend that the patient refrain from drinking liquids when swallowing food.
This patient received our usual maxillary wraparound retainer and requested a removable mandibular retainer as well. She slept in both retainers as needed for several years. Thirteen years after treatment, the open bite has not relapsed (Fig. 12).

Fig. 12 Case 2. Patient 13 years after treatment.
DR. SINCLAIR What else can you tell us about long-term stability?
DR. ALEXANDER One of the advantages of growing older is the ability to see former patients bring their children into the office. This also allows me time to study their long-term records and to see what really worked--which eventually led to a book called The Alexander Discipline: Long-Term Stability (Quintessence, 2011). Interestingly, my studies have shown that the requirements for stability have not changed much in all this time. The focus is on the mandibular anterior teeth: IMPA, intercanine width, root spread, and interproximal enamel reduction (Table 2).
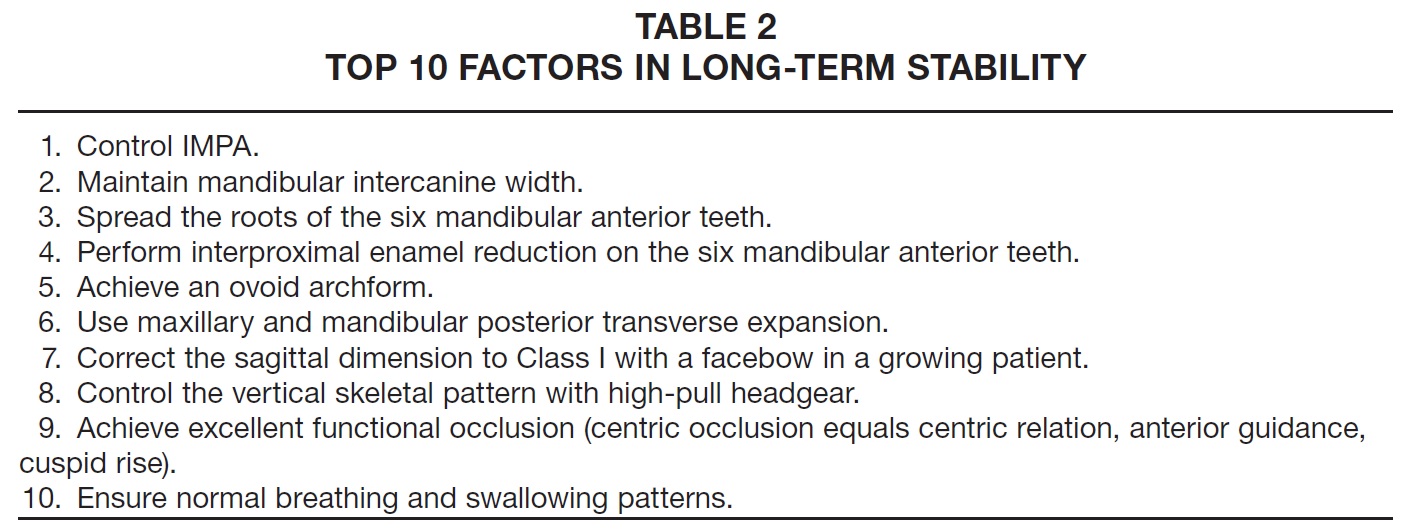
Over the last 30 years, clinicians have gone crazy attempting to resolve the skeletal Class II problem by substituting various appliances for the cervical facebow! But these appliances resolve the skeletal issue by "sacrificing" the mandibular incisors, which can be flared anteriorly into unstable positions. The result can be lifetime retention or relapse. Is it because of our success with the cervical facebow in countless patients--not placing undue forces on the mandibular anterior teeth--that our long-term results have been remarkably stable?
In reflecting on my passion for learning, then teaching orthodontic mechanics and philosophy, I always come back to the Room of Truth. I was taught to take complete diagnostic records, pretreatment and post-treatment. Eventually, the practical problem faced by all orthodontists is the additional time and space necessary to take these records and then store them. Fortunately, when I built my office I included additional rental space, which today is used for the Room of Truth. My son, J. Moody, now owns the building and continues to take final records and support the Room of Truth with his own patients.
I share this experience because it is responsible for more than 50 research studies from more than 10 universities. There is no technique to my knowledge that has been so scrutinized and yet has produced comparable results, especially regarding long-term stability. Our doors are still open for any qualified student to evaluate our case records. My former patients keep bringing their children in for treatment, and so we obtain more LTS patients.
Although there remain doubters, I am convinced there is such a thing as LTS. The future direction of orthodontic mechanics will depend on whether LTS remains a treatment goal. The good news is that it is not difficult to achieve these stable results.
DR. SINCLAIR What has been your greatest joy in orthodontics?
DR. ALEXANDER Beginning with nothing, I have had the pleasure of sharing my orthodontic beliefs with doctors literally around the world, creating life-long friends and, I hope, improving the quality of orthodontic treatment for their patients. But my greatest joy in orthodontics is having my sons, Chuck and J. Moody, and my nephew, Cliff (Fig. 13), follow in our footsteps--and become better orthodontists than we are!
Orthodontics has provided the vehicle for reaching people on many levels. My sons Chuck and Moody are impacting lives both inside and outside their clinics. Chuck is reaching young men as a part-time high-school football coach. Moody has created a dental mission, EthiopiaSmile--a group of doctors and lay people caring for dental needs of the destitute on annual trips to Ethiopia.
Our goal continues to be to "leave it better than we found it", and this is still a challenge every day. The joy of practicing orthodontics continues to flow through our family to our 12 grandchildren, who are the "cream of the crop"--and we're hoping for a third generation!

Fig. 13 The Alexander family of orthodontists, clockwise from left: Dr. Charles Alexander, Dr. C. Moody Alexander, Dr. Cliff Alexander, Dr. J. Moody Alexander, Dr. R.G. “Wick” Alexander.
Thank you so much for allowing me to share my thoughts about this wonderful profession. I must admit I am concerned about our future. I am concerned about excessive marketing focusing on the wrong issues. Are your patients better off today? Will the orthodontic specialty of the future offer the same opportunities as it did for me and my sons? It's up to each of us to leave it better than we found it. Thank you!
FOOTNOTES
- *Preformed LTS archwires, American Orthodontics, Sheboygan, WI; www.americanortho.com.



