Gradual Grinding of a Talon Cusp During Orthodontic Treatment
Dens evaginatus is a developmental aberration of a tooth resulting in formation of an accessory cusp that has been described as an abnormal tubercle, elevation, protuberance, excrescence, extrusion, or bulge. This uncommon anomaly projects above the adjacent tooth surface, with enamel covering a dentinal core that usually contains pulp tissue; occasionally, a slender pulp horn can extend the full length of the tubercle's dentin core.1
Similar articles from the archive:
- Precision Grinding June 1971
The phenomenon was first described by Mitchell in 18922 and was termed "talon cusp" by Mellor and Ripa in 19703 because of its resemblance to an eagle's talon. Talon cusps occur more frequently in the permanent dentition (75%) than the primary dentition (25%).4 The maxillary lateral incisors are most frequently involved (67%), followed by the maxillary central incisors (24%) and canines (9%).4-6
Early diagnosis and management of a talon cusp is important to prevent occlusal interference, compromised esthetics, formation of carious developmental grooves, periodontal problems due to excessive occlusal forces, and irritation of the tongue during speech and mastication.7-9 Treatment of the talon may not be required, however, unless esthetics or function is affected. Developing caries, severe attrition, or sharp cusp edges also call for resolution of the anomaly.10-11
During orthodontic treatment, a talon cusp may hinder anterior retraction and establishment of proper occlusion. This article describes the successful management of a talon cusp in an orthodontic patient.
Case Report
A 16-year-old male presented with the chief complaint of irregular upper front teeth. Clinical examination indicated a convex profile and a well balanced face. The patient had a Class I molar relationship with severe crowding in both arches (Fig. 1).
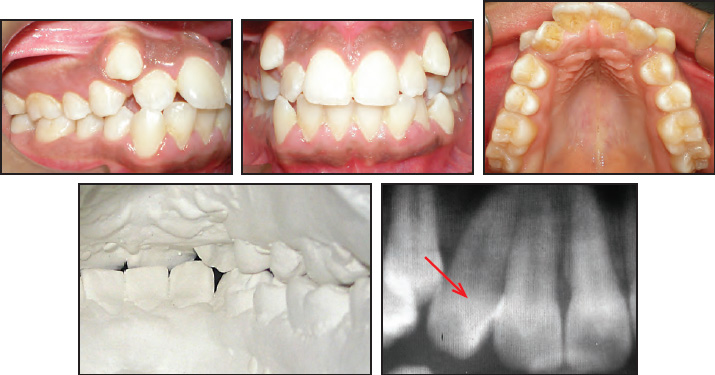
Fig. 1 16-year-old male patient with talon cusp on palatal surface of upper right lateral incisor before treatment.
A pyramidal talon cusp measuring 5.28mm in length (incisocervically), 4.66mm in width (mesiodistally), and 2.96mm in thickness (labiolingually) was noted on the palatal surface of the maxillary right lateral incisor (Fig. 2).

Fig. 2 Measurement of length, width, and thickness of talon cusp.
The tip of the cusp was attached to the crown of the incisor, which was in crossbite with the mandibular canine. No developmental grooves were noted at the junction of the talon cusp and the palatal surface of the incisor.
After extraction of the four first premolars, orthodontic treatment was initiated with standard edgewise brackets. Because of the anterior cross-bite, there was no occlusal interference from the talon cusp at first. After initial leveling and alignment, however, the cusp came into contact with the opposing teeth (Fig. 3), and the patient was referred to the Department of Conservative Dentistry and Endodontics for appropriate treatment.
The lateral incisor was causing no pain or discomfort, and vitality tests using an ice stick were positive. The patient was prescribed desensitizing toothpaste at the start of the talon-cusp treatment. At the first appointment, the palatal projection of the talon was ground enough to eliminate the premature contact. Thereafter, the talon cusp was reduced gradually, using a watercooled, flame-shaped diamond bur in a high-speed handpiece, at six-to-eight-week intervals (Fig. 4).

Fig. 3 Dental casts show occlusal interference from talon cusp after initial leveling and alignment.
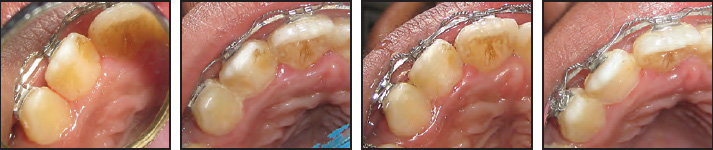
Fig. 4 Talon cusp reduced by grinding over four consecutive appointments at six-to-eight-week intervals.
Pulpal health was assessed with a cold test before each grinding session. After three further 1mm reductions of the cusp along the palatal surface, the palatal topography was similar to that of the contralateral tooth.
At the final grinding appointment, a thin layer of composite resin was applied over the palatal surface of the lateral incisor (Fig. 5).

Fig. 5 A. Thin layer of composite resin placed on palatal surface of lateral incisor following completion of talon-cusp grinding. B. Occlusion after reduction of talon cusp.
Pulpal health of the tooth was assessed at each succeeding visit over three months, while orthodontic treatment proceeded with upper space closure (Fig. 6).

Fig. 6 Space closure in upper arch without interference from talon cusp.
Discussion
According to the classification of Hattab and colleagues,4 our patient's anomaly was a Type I (Talon): an additional cusp projecting from the palatal surface of an anterior tooth and extending at least one-half the distance from the cementoenamel junction to the incisal edge. Most talon cusps contain extensions of pulp tissue similar to pulp horns.12 Since the talon cusp and its pulpal extension are superimposed over the main pulp chamber, however, the extent of the extra pulp horn becomes difficult to distinguish.13 In the present case, a pulp horn could not be confirmed.
Gradually grinding the talon cusp over several consecutive appointments has been recommended to preserve pulpal health.4,5,14 Considering the absence of occlusal trauma, periapical complications, and unsightly appearance related to the pathology in this case, there was no urgency in removing the interference. Our approach reduced the risk of pulp exposure and avoided the discomfort of deep dentinal cutting without hindering the progress of orthodontic treatment. Since most of the odontoblasts lie along the length of the cusp, rather than at the tip, the grinding was done on the side of the cusp to promote reparative dentin deposition.15 As advised by previous authors, a fluoride desensitizing toothpaste was prescribed to relieve any tooth sensitivity,16-18 and a thin layer of composite resin was applied on the final visit to cover the exposed dentin.19
The protocol presented here will not be appropriate in all situations, particularly if occlusal interference is severe. In such cases, a complete, immediate reduction of the cusp may be required, usually accompanied by pulp therapy such as rootcanal treatment or a partial pulpotomy.20
REFERENCES
- 1. Neville, B.; Damm, D.; Allen, C.; and Bouquot, J.: Oral and Maxillofacial Pathology, 2nd ed., W.B. Saunders, Philadelphia, 2002, pp. 77-79.
- 2. Mitchell, W.: Case report, Dent. Cosmos, 34:1036, 1892.
- 3. Mellor, J.K. and Ripa, L.W.: Talon cusp: A clinically significant anomaly, Oral Surg. Oral Med. Oral Pathol. 29:225-228, 1970.
- 4. Hattab, F.N.; Yassin, O.M.; and al-Nimri, K.S.: Talon cusp in permanent dentition associated with other dental anomalies: Review of literature and reports of seven cases, ASDC J. Dent. Child. 63:368-376, 1996.
- 5. Hattab, F.N.; Yassin, O.M.; and al-Nimri, K.S.: Talon cusp—Clinical significance and management: Case reports, Quintess. Int. 26:115-120, 1995.
- 6. Chen, R.J. and Chen, H.S.: Talon cusp in primary dentition, Oral Surg. Oral Med. Oral Pathol. 62:67-72, 1986.
- 7. Segura, J.J. and Jiménez-Rubio, A.: Talon cusp affecting permanent maxillary lateral incisors in 2 family members, Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 88:90-92, 1999.
- 8. Balciog˘lu, H.A.; Keklikog˘lu, N.; and Kökten, G.: Talon cusp: A morphological dental anomaly, Rom. J. Morphol. Embryol. 52:179-181, 2011.
- 9. Ozcelik, B. and Atila, B.: Bilateral palatal talon cusps on permanent maxillary lateral incisors: A case report, Eur. J. Dent. 5:113-116, 2011.
- 10. Mader, C.L.: Mandibular talon cusp, J. Am. Dent. Assoc. 105:651-653, 1982.
- 11. Mader, C.L.: Talon cusp, J. Am. Dent. Assoc. 103:244-246, 1981.
- 12. Shafer, W.G.; Hine, M.K.; and Levy, B.M.: A Textbook of Oral Pathology, 4th ed., W.B. Saunders, Philadelphia, 1983, pp. 40-41.
- 13. Mader, C.L. and Kellogg, S.L.: Primary talon cusp, ASDC J. Dent. Child. 52:223-226, 1985.
- 14. Al-Omari, M.A.O.; Hattab, F.N.; Darwazeh, A.M.; and Dummer, P.M.: Clinical problems associated with unusual cases of talon cusp, Int. Endod. J. 32:183-190, 1999.
- 15. Ekambaram, M.; Yiu, C.K.; and King, N.M.: An unusual case of double teeth with facial and lingual talon cusps, Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 105:e63-e67, 2008.
- 16. Myers, C.L.: Treatment of a talon-cusp incisor: Report of case, ASDC J. Dent. Child. 47:119-121, 1980.
- 17. Shey, Z. and Eytel, R.: Clinical management of an unusual case of dens evaginatus in a maxillary central incisor, J. Am. Dent. Assoc. 106:346-348, 1983.
- 18. Richardson, D.S. and Knudson, K.G.: Talon cusp: A preventive approach to treatment, J. Am. Dent. Assoc. 110:60-62, 1985.
- 19. Levitan, M.E. and Himel, V.T.: Dens evaginatus: Literature review, pathophysiology and comprehensive treatment regimen, J. Endod. 32:1-9, 2006.
- 20. Abbott, P.V.: Labial and palatal “talon cusps” on the same tooth: A case report, Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 85:726-730, 1998.






