The Pterygoid Anchorage Technique
Evidence-Based Considerations for Determining Appointment Intervals
(Editor's Note: In this quarterly column, JCO provides an overview of a clinical topic of interest to orthodontists. Contributions and suggestions for future subjects are welcome.)
A century ago, when orthodontic wires were constructed out of precious metals, their working range was relatively small, and office appointments had to be scheduled as often as once or twice a week. Over time, stainless steel replaced precious metals, and the orthodontist's working range improved, thanks to the ability to bend various loops and springs into the archwire. When elastomeric modules and stainless steel coil springs became the primary means of delivering force, monthly appointments were adequate. As the lattice structure of orthodontic wires evolved and working ranges further increased, a six-week interval became possible. In recent decades, the introduction of nickel titanium and superelastic wires has permitted appointments to be scheduled as far as 10 weeks apart in some cases.
It has long been established that optimum scheduling contributes to on-time finishing of orthodontic treatment.1 This article reviews current practices regarding intervals between visits and presents recommendations based on evidence from the literature.
Customary Appointment Intervals
In a 1988 study of 92 patients, Alger reported an average of 15.9 appointments over 22.0 months of treatment.2 Nonextraction cases (N = 37) averaged 13.9 appointments over 19.1 months, but extraction patients (N = 55) needed 16.9 visits over 23.7 months. Surgical-orthodontic cases required an average of 23 appointments over 30 months; patients with impacted teeth also took longer to treat, with a concomitant increase in the number of appointments.
Similar articles from the archive:
Alger routinely scheduled visits at six-week intervals, as opposed to the traditional four-week interval (although many patients were not seen for three to six months during summer holidays). Several practice-management issues arose as a result of these scheduling procedures, including fee-collection problems, since most patients were used to paying at their monthly visits.2 Alger concluded that extraction patients were probably best seen at four-week intervals, and that patients undergoing rapid maxillary expansion needed to be scheduled every one to two weeks for assessment of the expansion. He also surmised that patients who had poor oral hygiene or were undergoing compliance-dependent treatment (such as headgear or elastics) might need to be seen more frequently to foster psychological reinforcement and encouragement.
In an informal survey of 59 randomly selected practitioners in 2005, Sheridan found that the most common interval between appointments was five to six weeks, followed closely by seven to eight weeks.3 A four-week interval was uncommon, and only a few respondents reported booking patients at intervals longer than nine weeks or shorter than three weeks. The most frequently reported reasons for lengthening the period between appointments were the availability of highly resilient wires, constant-force springs, self-ligating brackets, and non-compliance mechanics such as the Herbst* appliance, as well as time constraints in families with two working parents and busy after-school schedules.
Sheridan's respondents noted that the treatment stage generally dictated the appointment interval: patients undergoing initial leveling and alignment could easily go six to eight weeks between visits, but the demands of finishing required a shorter interval of four to five weeks.3 Cases involving maxillary expansion, impacted teeth, or periodontal complications also needed more frequent appointments. Risk/benefit analysis indicated that longer appointment intervals reduced overall chairtime and overhead, freed up patients' schedules and resulted in less time out of school, and allowed practitioners to serve more patients. Disadvantages included a higher proportion of cases that were out of control or overcorrected, longer overall treatment periods, fee-collection problems, and inadequate monitoring of patients with poor oral hygiene.
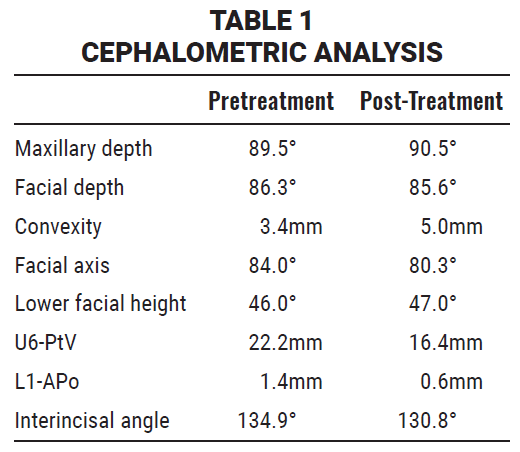
The 2008 AAO Patient and Member Census Study revealed that 40.6% of the 539 respondents scheduled appointments every six weeks, while another 23.4% preferred appointment intervals of seven to eight weeks4 (Table 1). These findings mirrored those of Sayers and Newton, who found that a slight majority of patients anticipated a visit every one to three months, including 20% who expected appointment intervals of between four and six weeks.5
Lindauer and colleagues found that patients who were behind in fee payments tended to miss more appointments6--an obvious pragmatic issue for practitioners. On the other hand, in Sondhi's experience, switching from a four-week to an eight-week appointment interval cut the total number of patient visits in half while doubling the fees collected per visit.7 Sondhi emphasized that the monthly payment plan must be dissociated from the number of office visits and archwire changes or adjustments, as well as the time spent at each visit.
Periodontal Considerations
The most commonly accepted hypothesis of how teeth move is the pressure-tension theory. According to Proffit, when light, prolonged pressure is placed on teeth, the periodontal ligament (PDL) is partially compressed on the pressure side and stretched on the tension side, resulting in tooth movement within the socket.8 This histophysiological phenomenon occurs within hours of force application. Frontal resorption results when the force levels are kept low and continuous, thus facilitating gradual tooth movement. Higher force levels create undermining resorption due to a delay in breakdown of the adjacent bone, resulting in tooth movement marked by alternating periods of movement and stasis. Although Proffit questioned whether the forces generated in clinical practice can produce the most efficient tooth movement, he strongly advised the use of low and continuous pressure to ensure optimal tooth movement and patient comfort.
Cellular activity is slower in elderly individuals than in children. Moreover, the PDL does not regenerate when periodontal tissue is inflamed. In patients with active periodontal disease, orthodontic tooth movement exacerbates the disease process, resulting in rapid and severe periodontal destruction.9 In almost every case, however, orthodontics is associated with small amounts of alveolar crestal bone loss, slight increases in gingival recession, and transient increases in pocket depths.10
The appointment interval has a definite effect on periodontal status. Orthodontic appliances are plaque traps that are either in contact with or in close proximity to the supporting periodontal structures for extended lengths of time. Because patient hygiene is monitored less often when the appointment interval is longer, there is a greater risk of delay in diagnosing periodontal disease.
Root Resorption
Root resorption is an iatrogenic consequence of orthodontic treatment. A systematic review of 24 articles concluded that while the causes of root resorption are multifactorial, there are direct correlations among overall treatment duration, the use of fixed appliances, dental root morphology, individual susceptibility, and the type of tooth movement.11 Fortunately, this effect is usually of minor clinical significance. One study found mild root resorption of 1.9%, 3.2%, 4.9%, and 8.6% in orthodontic patients at the beginning of treatment, the six- and 12-month marks, and the end of treatment, respectively.12 When moderate resorption was discovered, the authors diminished the forces applied to the teeth, employed resting periods, and reduced the overall treatment time. They recommended that patients who exhibit root resorption within the first year of treatment should be observed monthly.
Since root remodeling is always a concomitant of orthodontic tooth movement, the permanent loss of tooth structure essentially results from a lack of cemental repair. Overly frequent activation of orthodontic appliances interferes with the normal process of breakdown and repair,8,13 which suggests that a longer appointment interval can prevent or at least minimize the resorptive process. When an appliance delivers light, continuous forces that produce frontal (as opposed to undermining) resorption, there is little need to activate it more often.
Decalcification
Enamel decalcification in the form of whitespot lesions appears when plaque is retained on the tooth surface for a prolonged period of time. Half of all orthodontic patients exhibit at least one area of decalcification, with most lesions appearing in the maxillary anterior segment or mandibular posterior area.14 Ranging in intensity from slight discoloration to cavitated lesions, decalcification has the potential to reach depths of 75-100 microns, with 25% mineral loss in as little as four weeks. The incidence of decalcification does not appear to differ between patients treated for short (15-month) vs. long (36-month) periods of time.14 Since the major risk factor is the patient's oral hygiene, a longer appointment interval may compromise the practitioner's ability to diagnose and manage this problem in a timely manner.
Treatment options for decalcification include observation (with the expectation of eventual remineralization) and restorative procedures.15,16 Decalcification can be minimized by prescribing a .2% sodium fluoride rinse, particularly one with a low pH,17 or by using a fluoride-releasing glass ionomer adhesive.18
Biomaterials
The development of round and rectangular nickel titanium wires and coil springs revolutionized clinical orthodontics. A nickel titanium archwire has two clinically relevant properties: shape memory19 and superelasticity.20 The nonlinear unloading characteristics of the wire, as it changes phases from martensitic to austenitic, results in the transmission of less force to the teeth over a greater working range, thus inducing a more physiologic movement (frontal resorption) while improving patient comfort. Increasing the interbracket distance or bypassing specific teeth during initial leveling and alignment also reduces force levels. Because the wire stiffness increases toward the end of activation, archwires do not need to be changed as often; according to Viazis, two-month appointment intervals are usually sufficient.21
From a scheduling perspective, the longer a low force can be delivered, the more efficient tooth movement becomes. Therefore, the orthodontist should use appropriately sized multistranded stainless steel archwires (in cases of mild interdental distortion), superelastic nickel titanium archwires (in cases of mild-to-moderate interdental distortion), or copper nickel titanium archwires (in cases involving severe interdental distortion or requiring early torque control) and should leave each wire in place longer before progressing to the next size. Overtreatment with unnecessary or frequent archwire changes will inhibit the full expression of the wire's working range and hence its biomechanical advantages.22
Elastomeric chain and nickel titanium coil springs are the two other force-delivery systems most commonly used to move teeth. In a study comparing these two modules, a chain was placed in one quadrant and an open-coil spring applied to the contralateral side, with each stretched to produce the same amount of force.23 Patients were scheduled at four-to-six-week appointment intervals (although some did not return for four to five months). Elastomeric chain retained an average of 53% of its initial force over one to 15 weeks, while nickel titanium coil springs maintained an average of 52% over a one-to-22-week period. In both samples, the degree of degradation correlated with the strength of the initial force. Space closure occurred at the rate of .21mm per week for elastomeric chain and .26mm per week for the coil spring--virtually the same--and both systems had sufficient residual force to accommodate appointment intervals longer than six weeks.
Orthodontic brackets have been intentionally omitted from this review. Opinions are currently mixed on whether one type of bracket is more efficient than another.24,25
Recommendations
The evidence indicates that when scheduling orthodontic appointments, one size does not fit all. Appropriate intervals can be as short as one to two weeks or as long as eight to 10 weeks, based on the following considerations:
1. Patient age. Because of a slower cellular response and a higher risk for periodontal disease, adult patients should be seen at shorter intervals (four to six weeks) than children.
2. Type of archwire and force-delivery system. Nickel titanium archwires should be used for initial leveling and alignment and left undisturbed as long as possible. During space closure, appointment intervals of six to eight weeks are generally acceptable, regardless of the force-delivery system, as long as sliding mechanics are employed. The interval can be extended to as long as 10 weeks under clinically appropriate circumstances.
3. Periodontal status. Patients with a history of periodontal disease or poor oral hygiene should bescheduled at intervals of four weeks or less. Whether to extend the treatment interval to the eight-week range for specific procedures, such as space closure with sliding mechanics, should be premised on the patient's periodontal health.
4. Extraction vs. nonextraction. Longer appointment intervals (six to eight weeks) may be routinely used in nonextraction cases. Patients undergoing extraction treatment should be scheduled in four-to-six-week blocks unless straightforward sliding mechanics are used for space closure, in which case a six-to-eight-week interval is acceptable.
5. Surgical and impacted cases. Patients undergoing orthognathic surgery should be scheduled according to whether extraction is part of their treatment plan. Four-week intervals are recommended during presurgical finishing to minimize overcorrection. Patients with impactions should be seen every four weeks to be checked for side effects secondary to the eruptive mechanics, periodontal sequelae, and root resorption.
6. Compliance vs. non-compliance mechanics. Patients being treated with compliance-dependent appliances such as headgear or elastics should be seen at shorter intervals (four weeks). Although rapid maxillary expansion is not a compliance issue, these patients should be seen at one-to-two-week intervals so their expansion can be monitored. Patients undergoing treatment with non-compliance mechanics may be scheduled at intervals as long as eight weeks.
7. Decalcification and white-spot lesions. Patients with decalcification and poor oral hygiene must be seen at four-week intervals, without exception.
8. Root resorption. Assuming a progress x-ray is taken about nine months into treatment, patients exhibiting mild resorption (blunting only) may be seen every six weeks. Those with more serious resorption require four-week appointment intervals to ensure appropriate monitoring. A patient with clinically relevant root resorption may need a two-to-three-month resting period; when treatment is resumed, the interval between appointments should not exceed four weeks.
9. Schedule considerations. Parents who must take time off from work or children with heavily scheduled after-school activities may go as long as eight weeks between appointments, unless considerations such as poor hygiene, impactions, asymmetry, or the use of non-sliding space-closure mechanics dictate otherwise.
Whatever the appointment interval, the financially responsible party must be made to understand that the payment schedule is not connected to the number or length of appointments during treatment, the procedures performed, or the time interval between visits. The fee schedule is simply a plan to conveniently budget payments for services rendered. This should be clearly stated on the truth-in-lending statement signed by the financially responsible party.26
FOOTNOTES
- *Registered trademark of Dentaurum GmbH & Co., Turnstrasse 31, 75228 Ispringen, Germany; www.dentaurum.de.
REFERENCES
- 1. Gottlieb, E.L.: The Editor's Corner, J. Clin. Orthod. 29:679-680, 1995.
- 2. Alger, D.W.: Appointment frequency versus treatment time, Am. J. Orthod. 94:436-439, 1988.
- 3. Sheridan, J.J.: The Readers' Corner, J. Clin. Orthod. 39:535-537, 2005.
- 4. 2008 AAO Patient and Member Census Study, American Association of Orthodontists, St. Louis, 2009.
- 5. Sayers, M.S. and Newton, J.T.: Patients' expectations of orthodontic treatment, Part 1: Development of a questionnaire, J. Orthod. 33:258-269, 2006.
- 6. Lindauer, S.J.; Powell, J.A.; Leypoldt, B.C.; Tufekci, E.; and Shroff, B.: Influence of patient financial account status on orthodontic appointment attendance, Angle Orthod. 79:755-758, 2009.
- 7. Sondhi, A.: Sondhi signature treatment system: Doing the right things right, Orthod. Persp., January 2001.
- 8. Proffit, W.R.: The biologic basis of orthodontic therapy, in Contemporary Orthodontics, 4th ed., ed. W.R. Proffit, H.W. Fields, and D.M. Sarver, C.V. Mosby Co., St. Louis, 2007, pp. 331-358.
- 9. Ong, M.M. and Wang, H.L.: Periodontic and orthodontic treatment in adults, Am. J. Orthod. 122:420-428, 2002.
- 10. Bollen, A.M.; Cunha-Cruz, J.; Bakko, D.W.; Huang, G.J.; and Hojoel, P.P.: The effects of orthodontic therapy on periodontal health:Â A systematic review of controlled evidence, J. Am. Dent. Assoc. 139:413-422, 2008.
- 11. Lopatiene, K. and Dumbravaite, A.: Risk factors of root resorption after orthodontic treatment, Stomatologija 10:89-95, 2008.
- 12. Makedonas, D.; Odman, A.; and Hansen, K.: Management of root resorption in a large orthodontic clinic, Swed. Dent. J. 33:173-180, 2009.
- 13. Damon, D.: The Damon low-friction bracket: A biologically compatible straight-wire system, J. Clin. Orthod. 32:670-680, 1998.
- 14. Gorelick, L.; Geiger, A.M.; and Gwinnett, A.J.: Incidence of white spot formation after bonding and banding, Am. J. Orthod. 81:93-98, 1982.
- 15. Glatz, E.G.M. and Featherstone, J.D.B.: Demineralization related to orthodontic bands and brackets--a clinical study, Am. J. Orthod. 87:87, 1985.
- 16. Ogaard, B.; Rolla, G.; and Arends, J.: Orthodontic appliances and enamel demineralization, Part 1: Lesion development, Am. J. Orthod. 94:68-73, 1988.
- 17. Ogaard, B.; Rolla, G.; Arends, J.; and ten Cate, J.M.: Orthodontic appliances and enamel demineralization, Part 2: Prevention and treatment of lesions, Am. J. Orthod. 94:123-128, 1988.
- 18. Gorton, J. and Featherstone, J.: In vivo inhibition of demineralization around orthodontic brackets, Am. J. Orthod. 123:10-14, 2003.
- 19. Hurst, C.L.; Duncanson, M.G. Jr.; Nanda, R.S.; and Angolkar, P.V.: An evaluation of the shape-memory phenomenon of nickel-titanium orthodontic wires, Am. J. Orthod. 98:72-76, 1990.
- 20. Miura, F.: Reflections on my involvement in orthodontic research, Am. J. Orthod. 104:531-538, 1993.
- 21. Viazis, A.D.: Bioefficient therapy, J. Clin. Orthod. 29:552-568, 1995.
- 22. Santoro, M.; Nicolay, O.F.; and Cangialosi, T.J.: Pseudoelasticity and thermoelasticity of nickel-titanium alloys: A clinically oriented review, Part II: Deactivation forces, Am. J. Orthod. 119:594-603, 2001.
- 23. Nightingale, C. and Jones, S.P.: A clinical investigation of force delivery systems for orthodontic space closure, J. Orthod. 30:229-236, 2003.
- 24. Chen, S.S.; Greenlee, G.M.; Kim, J.E.; Smith, C.L.; and Huang, G.J.: Systematic review of self-ligating brackets, Am. J. Orthod. 137:726.e1-726.e18, 2010.
- 25. Fleming, P.S. and Johal, A.: Self-ligating brackets in orthodontics: A systematic review, Angle Orthod. 80:575-584, 2010.
- 26. Jerrold, L.: The truth and nothing but the truth: Using a truthin-lending statement in clinical orthodontic practice, Orthod. Prod., July/August 1999.