Survey of Orthodontists' Attitudes and Experiences Regarding Miniscrew Implants
Orthodontic miniscrews are becoming widely used on the basis of their ability to provide skeletal anchorage and to reduce the need for patient compliance.1-7 To date, few clinical studies have assessed implant success rates, the predictability of placement techniques, or the management of risk factors for failure.8 Only two articles have reported directly on miniscrew placement patterns among private orthodontic practices in the United States.9,10
The Department of Orthodontics at the University of Washington at Seattle has established an orthodontist subnetwork within the Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry (PRECEDENT). The following article describes the results of a survey of network orthodontists' attitudes toward miniscrew usage and their experiences with failures and related complications.
Methods
The study was developed under the direction of PRECEDENT and approved by the institutional review board at the University of Washington at Seattle. Orthodontists in Idaho, Montana, Oregon, Utah, and Washington interested in joining the network were certified as investigators by completing a DVD training module and satisfying the HIPAA and Responsible Conduct of Research training requirements of the network.
Similar articles from the archive:
Each certified network orthodontist was e-mailed a secure link to a web-based survey. This recollection- and opinion-based questionnaire was divided into six sections: practice characteristics, treatment planning, practice management, miniscrew placement, miniscrew complications and failures, and miniscrew removal.
Blinded, annotated data were extracted for statistical analysis. Cross-tabulations were performed as appropriate, and the significance of observed differences was assessed by means of the Wilcoxon rank-sum, chi-square, or Fisher exact test as appropriate. A "p" value of .05 or less was considered statistically significant.
Results
Practice Characteristics
In all, 47 of 59 eligible orthodontists completed the survey, for an 80% response rate. Respondents were distributed geographically among all five network states, and the 47 practitioners were graduates of 28 different residency programs. Most respondents (57%) had been in practice more than 10 years; only three had been out of residency for less than two years.
Miniscrew Experience
Forty-three of the doctors (91%) reported treating at least one patient with miniscrews, but only 20 (43%) reported placing the devices personally. Of the 23 who had referred patients for the procedure, all had referred to oral surgeons, 19 to periodontists, and three to general dentists.
Experience levels varied widely among the 20 practitioners who had placed miniscrews themselves. No clinician reported using miniscrews before 2005, and five had begun placing screws as recently as 2009. Only six reported having placed more than 20 miniscrews.
The most common reason cited for not placing miniscrews personally was the need to administer a local anesthetic (58%). Other factors included longer chairtime (25%), the potential need to manage acute pain (20%), and lack of training (20%).
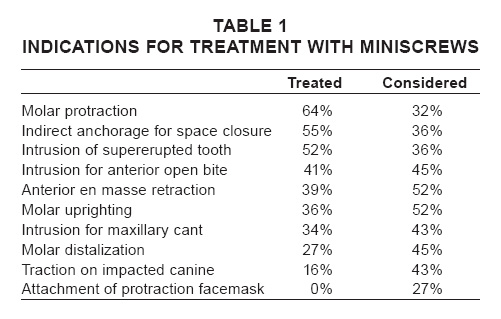
Molar protraction was the most commonly reported treatment indication (64%), followed by indirect anchorage for space closure (55%) and intrusion of supererupted teeth (52%; Table 1). A panoramic radiograph was the most requested or readily available diagnostic tool used to guide miniscrew placement. For pain management, most respondents (69%) reported using a combination of topical and local anesthetics; 38% said they administered only a strong topical agent, while 10% used a full nerve block.
The three preferred miniscrew systems were those manufactured by 3M Unitek*, Dentaurum**, and Ormco***, while 10 other systems were used by far fewer doctors. The 1.4mm- and 1.6mm- diamater miniscrews were most popular, in lengths of 8-10mm. Regardless of the system used, 28 of 29 respondents reported always or frequently loading the implants with force immediately after placement.
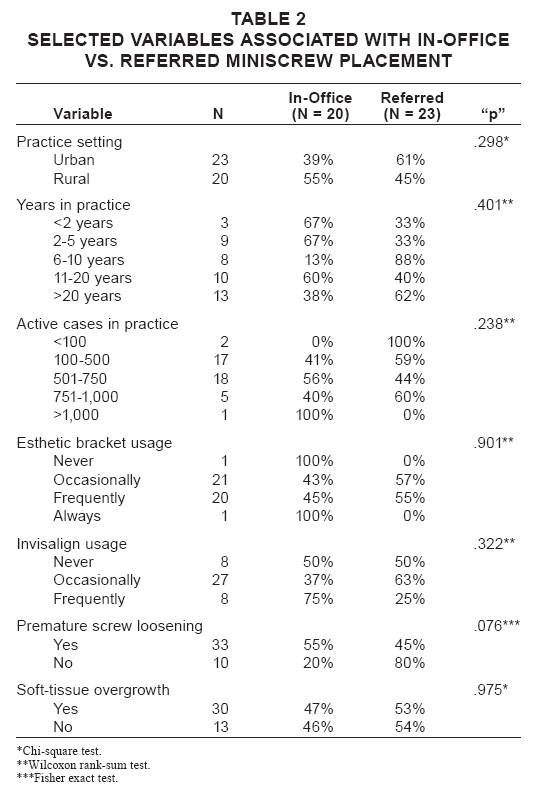
A cross-tabulation of practice variables with miniscrew placement experience (in-office vs. referred) is shows in Table 2. No variables tested were statistically significant.
Miniscrew Complications
The most commonly reported biological, mechanical, or iatrogenic complications of miniscrew treatment (Fig. 1) were screw loosening (76%), soft-tissue overgrowth/irritation (69%), and irritation caused by auxiliary springs(67%). There were no reported cases of tooth ankylosis, sinus perforation, or subcutaneous emphysema.
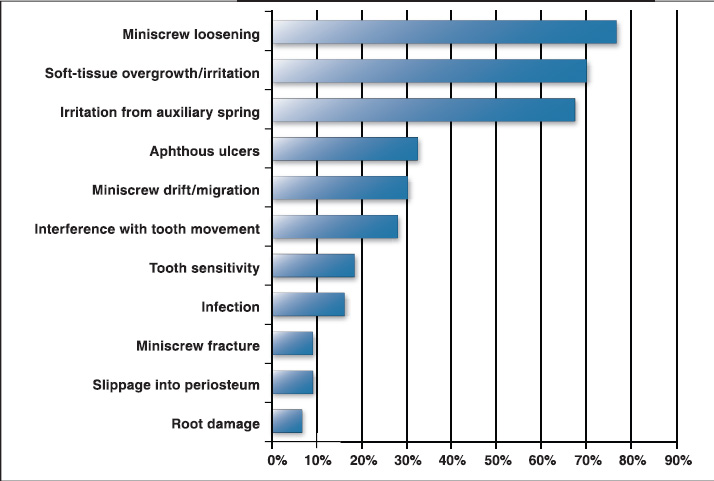
Fig. 1 Percentages of orthodontists reporting various biological or mechanical complications of miniscrew implants.
The most commonly cited side effect of miniscrew usage was excessive torquing/tipping of teeth, with 32% of the respondents reporting at least one occurrence. Much less commonly reported side effects were excessive extrusion/intrusion of teeth (7%) and root resorption (7%).
Most respondents (82%) were satisfied with the performance of miniscrews in their practices. Only one respondent who had personally placed miniscrews reported being dissatisfied enough to stop using the devices. Of the 23 practitioners who had referred miniscrew placement, six were dissatisfied. Reasons cited for dissatisfaction were that the procedure was not well tolerated by patients and that tooth movement was not as effective as hoped.
Discussion
Although miniscrew usage has been less common within the United States than in other parts of the world,10orthodontists practicing in the five Northwest PRECEDENT states appear to be adopting this technique rapidly.
Results of our study are comparable with those of two larger-scale published surveys of orthodontists' experiences with miniscrews.9,10 Our study had a higher response rate, but the potential number of participants was limited, whereas JCO invited all orthodontists in the United States9 and the AAO surveyed all its U.S. and international members.10 The proportion of respondents placing miniscrews personally in our study (43%) was identical to that reported in the JCO survey9 and somewhat lower than that in the AAO member survey (55%).10 Referral to oral surgeons over periodontists was preferred consistently across all three studies.
Our network respondents and the AAO respondents10 agreed regarding the use of diagnostic tools, anesthesia protocols, and the timing of force loading. A panoramic radiograph was the primary placement guide in both surveys, and near-equal percentages reported using a combination of topical and local anesthetics rather than topical agents alone. Immediate loading within two weeks after miniscrew placement was performed by about 80% of both samples, in agreement with the 2007 Cochrane Review's recommendations on the appropriateness of early loading.8 These results suggest an evolving consensus regarding certain aspects of miniscrew treatment--a trend noted by Baumgaertel and colleagues.11
The most common miniscrew treatment indications differed slightly among our network members, AAO members, and JCO survey respondents. Although space closure and bodily movement were the most commonly reported indications in both the PRECEDENT and AAO groups,10 respondents to the JCO survey were more likely to use miniscrews for molar intrusion9--an application that has been linked to higher failure rates in two studies.3,12 By comparison, the most common indication for miniscrew placement in previous studies has been maxillary anterior retraction, followed by molar protraction and posterior intrusion, with other types of treatment in a clear minority.3,4,13,14
Two recent systematic reviews have suggested that implant diameters of less than 1.3mm or greater than 2mm, as well as lengths of less than 8mm, are more susceptible to failure.15,16 Our network respondents' preferred miniscrew diameters of 1.4mm or 1.6mm and lengths of 8-10mm agreed with these guidelines.
Assuming that premature screw loosening constitutes a failure rather than a complication, the two complications reported most often by network orthodontists were soft-tissue overgrowth/irritation and irritation from a spring or attachment. The high percentage of orthodontists reporting softtissue complications, whether the procedure had been performed in-office or after referral, correlates with growing concerns about inflammation and tissue hypertrophy. A recent systematic review highlighted the lack of published information on the character and duration of inflammation surrounding miniscrews.16 Two studies have found soft-tissue overgrowth and inflammation to be significant risk factors for implant failure17,18; another noted an increased failure risk with placement in nonkeratinized tissue.19 In a recent survival analysis from Thailand, inflammatory hypertrophy entered the model as a significant risk factor, with the application of orthodontic force, irritation from stainless steel ligatures, and plaque accumulation postulated as etiologic factors.18 Combined with our findings, these data suggest that orthodontists need to be aware of the potential for soft-tissue complications and that this area needs further investigation.
Network orthodontists reported a higher incidence of premature screw loosening when they had placed the miniscrews themselves rather than referring the patients to a periodontist or surgeon for placement (90% vs. 65%, respectively). The association between these variables approaches statistical significance (p = .076), and examination of this phenomenon in a larger sample would help clarify its implications.
Our study reflects the challenges inherent in practice-based research.20 These include difficulty in recruiting younger practitioners, who may not be motivated to participate in research, and potential self-selection by orthodontists who are eager to participate--both of which can lead to biased findings. Other possible limitations are the small number of participants and an overrepresentation of orthodontists from the greater Seattle metropolitan area (45% of the respondents). This survey also lacks a temporal component, in that respondents were asked to report instances of complications and other events in current and past cases, not their incidence over time. In addition, the survey depended on recollection instead of chart review, which may affect its reliability. Future PRECEDENT studies aim to continue using this new orthodontic subnetwork with improved study designs and outcomes assessments.
ACKNOWLEDGMENTS: Northwest PRECEDENT is supported by grants U01DE016750 and U01DE16752 from the National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD.
FOOTNOTES
- *3M Unitek, 2724 S. Peck Road, Monrovia, CA 91016; www.3Munitek.com.
- **Dentaurum USA, 10 Pheasant Run, Newtown, PA 18940; www.dentaurum.com.
- ***Ormco Corp., 1717 W. Collins Ave., Orange, CA 92867; www.ormco.com.
REFERENCES
- 1. Papadopoulos, M.A. and Tarawneh, F.: The use of miniscrew implants for temporary skeletal anchorage in orthodontics: A comprehensive review, Oral Surg. Oral Med. Oral Path. Oral Radiol. Endod. 103:e6-e15, 2007.
- 2. Tracey, S.: The nuts and bolts of miniscrews, Orthod. Prod., February 2006, pp. 22-28.
- 3. Kuroda, S.; Sugawara, Y.; Deguchi, T.; Kyung, H.M.; and Takano-Yamamoto, T.: Clinical use of miniscrew implants as orthodontic anchorage: Success rates and postoperative discomfort, Am. J. Orthod. 131:9-15, 2007.
- 4. Chen, Y.J.; Chang, H.H.; Huang, C.Y.; Hung, H.C.; Lai, E.H.; and Yao, C.J.: A retrospective analysis of the failure rate of three different orthodontic skeletal anchorage systems, Clin. Oral Impl. Res. 18:768-775, 2007.
- 5. Moon, C.H.; Lee, D.G.; Lee, H.S.; Im, J.S.; and Baek, S.H.: Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal region, Angle Orthod. 78:101-106, 2008.
- 6. Kuroda, S.; Yamada, K.; Deguchi, T.; Hashimoto, T.; Kyung, H.M.; and Takano-Yamamoto, T.: Root proximity is a major factor for screw failure in orthodontic anchorage, Am. J. Orthod. 131(4 suppl):S68-S73, 2007.
- 7. Miyawaki, S.; Koyama, I.; Inoue, M.; Mishima, K.; Sugahara, T.; and Takano-Yamamoto, T.: Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage, Am. J. Orthod. 124:373-378, 2003.
- 8. Skeggs, R.M.; Benson, P.E.; and Dyer, F.: Reinforcement of anchorage during orthodontic brace treatment with implants or other surgical methods, Cochrane Database Syst. Rev. 3:CD005098, 2007.
- 9. Keim, R.G.; Gottlieb, E.L.; Nelson, A.H.; and Vogels, D.S. III: 2008 JCO Study of Orthodontic Diagnosis and Treatment Procedures, Part 1: Results and trends, J. Clin. Orthod. 42:625-640, 2008.
- 10. Buschang, P.H.; Carrillo, R.; Ozenbaugh, B.; and Rossouw, P.E.: 2008 survey of AAO members on miniscrew usage, J. Clin. Orthod. 42:415-418, 2008.
- 11. Baumgaertel, S.; Razavi, M.R.; and Hans, M.G.: Mini-implant anchorage for the orthodontic practitioner, Am. J. Orthod. 133:621-627, 2008.
- 12. Antoszewska, J.; Papadopoulos, M.A.; Park, H.S.; and Ludwig, B.: Five-year experience with orthodontic miniscrew implants: A retrospective investigation of factors influencing success rates, Am. J. Orthod. 136:158.e1-158.e10, 2009.
- 13. Wiechmann, D.; Meyer, U.; and Buchter, A.: Success rate of mini- and micro-implants used for orthodontic anchorage: A prospective clinical study, Clin. Oral Impl. Res. 18:263-267, 2007.
- 14. Berens, A.; Wiechmann, D.; and Rudiger, J.: Skeletal anchorage in orthodontics with mini and microscrews, Int. Orthod. 3:235-243, 2005.
- 15. Chen, Y.; Kyung, H.M.; Zhao, W.T.; and Yu, W.J.: Critical factors for the success of orthodontic mini-implants: A systematic review, Am. J. Orthod. 135:284-291, 2009.
- 16. Reynders, R.; Ronchi, L.; and Bipat, S.: Mini-implants in orthodontics: A systematic review of the literature, Am. J. Orthod. 135:564.e1-564.e19, 2009.
- 17. Park, H.S.; Lee, S.K.; and Kwon, O.W.: Group distal movement of teeth using microscrew implant anchorage, Angle Orthod. 75:602-609, 2005.
- 18. Viwattanatipa, N.; Thanakitcharu, S.; Uttraravichien, A.; and Pitiphat, W.: Survival analyses of surgical miniscrews as orthodontic anchorage, Am. J. Orthod. 136:29-36, 2009.
- 19. Cheng, S.J.; Tseng, I.Y.; Lee, J.J.; and Kok, S.H.: A prospective study of the risk factors associated with failure of miniimplants used for orthodontic anchorage, Int. J. Oral Maxillofac. Impl. 19:100-106, 2004.
- 20. Harrison, L.: Practitioners face challenges with office-based research, DrBicuspid.com News, April 1, 2009, www. drbicuspid.com/index.aspx?sec=nws&sub=rad&pag=dis&ItemId=301674, accessed October 1, 2009.






