JCO INTERVIEWS
Richard P. McLaughlin, DDS, on Facial and Dental Planning
DR. KEIM Dr. McLaughlin, your new book, Facial and Dental Planning for Orthodontists and Oral Surgeons, co-authored with Dr. Bill Arnett,1 focuses on diagnosis and treatment planning. What do you see as the new, unique, and different aspects of the philosophy of diagnosis and treatment planning?
DR. MCLAUGHLIN Emphasis is on three areas of evaluation--the temporomandibular joints, the face, and the dentition--with new and easier-to-use information in each area. In addition to the traditional methods of TMJ evaluation and treatment, there is the challenging area of TMJ remodeling with emphasis on stabilization and medical management. Important contributions are made in the book by Dr. Tom Eggleton (physical therapy), Dr. Richard Gevirtz (biofeedback), and Dr. Steve Milam (medical management and TMJ lavage). Next there are more thorough and objective methods of facial planning. In the past, due to incomplete clinical examination and inadequate information from cephalometric x-rays, more subjective facial planning decisions have been made. While this may produce adequate results, there is a greater chance of error. In my opinion, the above areas are two of Dr. Arnett's great contributions to both orthodontics and oral surgery. Finally, once a decision has been made concerning the angulation and the anteroposterior and vertical position of the incisors from the facial analysis, specific information is provided for calculating the orthodontic movements required for the midlines, cuspids, and molars. This, too, reduces errors in the dental alignment of our cases.
Similar articles from the archive:
DR. KEIM What do you see as the appropriate goals for treatment planning?
DR. MCLAUGHLIN The goals of treatment include:
- Healthy musculature and temporomandibular joints
- Facial balance
- Correct static and functional occlusion
- Periodontal health
- Resolving the patient's chief complaints
- Stability of dental and skeletal changes
- Improved airway
DR. KEIM What are the requirements for a systematized and objective approach to diagnosis and treatment planning?
DR. MCLAUGHLIN It is important that very specific methods and techniques be carried out from the initial contact with the patient to the presentation of the treatment plan. Important steps cannot be eliminated along the way, and checks and balances need to occur as the process proceeds. In addition, objective methods rather than subjective opinions should accompany the process.
DR. KEIM Where is the patient's chief complaint addressed in this protocol?
DR. MCLAUGHLIN After obtaining personal information from the patient, a "Chief Complaint Form", as developed by Dr. Arnett, is completed.2 The original form has been modified into two forms: a basic orthodontic form for routine cases, and a surgical form for more complex cases. Each form is in three sections, asking questions concerning the face, the teeth, and symptoms (the TMJs). This form is reviewed with the patient at the initial examination and once again at the consultation to insure that the patient's concerns are being addressed.
DR. KEIM What are the essential elements of a clinical patient exam?
DR. MCLAUGHLIN The clinical exam consists of three parts: the TMJ exam, the facial exam (frontal view and profile view), and the intraoral exam. A screening TMJ examination is indicated for all patients, whether they do or do not describe symptoms. Two palpation positions (over the condyles externally and using the small fingers in the ear canal) are used during three mandibular movements (opening and closing, left and right lateral, and protrusion). These provide information concerning the patient's range of movement, deviation from normal movements, any pain during movement, and joint sounds. The protocol for the facial examination was published by Dr. Arnett and Dr. Robert Bergman,3 but both the frontal and profile facial exams have been modified slightly since the original publication. Lastly, the intraoral exam is completed, recording necessary information.
DR. KEIM What do you see as the main areas of diagnosis?
DR. MCLAUGHLIN The main areas of diagnosis follow the main areas of the clinical exam. Concerning the temporomandibular joints, it is important to determine if the problem is purely muscular, strictly limited to the joints, or, more commonly, a combination of the two. It is critical to determine the location and extent of TMJ damage--in other words, local or total remodeling of the condyle. A main emphasis of the book is to evaluate the face three-dimensionally and objectively determine and quantify the areas of facial deformity. By doing this, we can be more accurate in determining the best method of treatment as well as alternative options. In the past, this has been an area of subjective estimates, and mistakes are possible with such an approach. Concerning the dentition, accurate determinations need to be made of molar relationships, midlines, occlusal cants, arch widths, arch crowding, and planes of occlusion. This can then be combined with information on ideal incisor positioning from the facial plan. With this information, a more accurate determination can be made concerning tooth movements needed and anchorage requirements.
DR. KEIM How is "facial planning" different from traditional orthodontic treatment planning?
DR. MCLAUGHLIN Facial planning involves two key components that have not been as thoroughly addressed as possible in the past. The first key is a thorough clinical facial examination. This provides us with important soft-tissue, dental, and skeletal information in the frontal (transverse and vertical) dimension and the sagittal (vertical and horizontal) dimension. This information can be developed and objectified by the second key, which is Soft Tissue Cephalometric Analysis (STCA) and Cephalometric Treatment Planning (CTP). These two methods help us to minimize the weaknesses inherent in cranial base references and provide us with significantly greater soft-tissue information.
DR. KEIM How does facial planning differ from traditional facial planning based on cranial base measurements?
DR. MCLAUGHLIN Utilizing cranial base landmarks to evaluate difficult cases has always been problematic, since these landmarks vary in position from patient to patient, and are often hard to locate on the head film. Also, traditional cephalometric treatment planning has focused on dentoskeletal factors, with only minimal emphasis on soft tissues. Surgeons in the 1980s (Epker, Wolford, and others) began focusing more on soft tissue by utilizing a line perpendicular to Frankfort horizontal and through subnasale. Such a method provided a greater focus on soft tissue; however, it was still subject to the problems associated with the cranial base landmark, Frankfort horizontal. Studies by various authors in the 1980s and 1990s (for example, Lundstrom and Lundstrom4) suggested that utilizing natural head posture was a more accurate reference than cranial base references. The True Vertical Line is a vertical line through subnasale with the patient in natural head posture. Dr. Arnett used this line to develop his analysis,5 which provides us with thorough information on virtually all of the important dentoskeletal and soft-tissue measurements in the vertical and horizontal planes.
DR. KEIM What kind of standards are used in an objective treatment-planning system?
DR. MCLAUGHLIN We have had objective standards relative to static occlusion, such as Dr. Andrews's six keys, and functional occlusion, such as the goals described by Dr. Roth. Admittedly, we are unable to achieve these goals in every case, and the reasons are multiple. This does not mean that we discard them as irrelevant. They continue to serve as objective references and reasonable goals to achieve whenever possible. In the same way, we can benefit from objective standards relative to facial planning, even though we are unable to achieve such results in each case. More research is needed so that objective standards are established for different ethnic groups. In addition to the Arnett norms (essentially a Caucasian Southern California group), the Japanese are well on the way to completing and publishing their norms. Studies are also ongoing in Korea and India to my knowledge. This is a very exciting project, and the minor differences are enlightening.
DR. KEIM What role does condylar position play in this method of case documentation?
DR. MCLAUGHLIN Consistent condyle positioning is critical in the case documentation process. If this is not done, critical errors can be made in treatment planning. A wax bite with proper condyle positioning is placed when taking facial photographs and cephalometric x-rays and when mounting study models. In this way, there is a consistency of records when evaluating the case.
DR. KEIM Where should the condyle be placed during record taking?
DR. MCLAUGHLIN The condyle needs to be seated superiorly in the fossa in an uncompressed position during record taking. The position may vary slightly from patient to patient and is probably a very small area vs. a pinpoint position. This perspective is not a license to be sloppy during record taking, but a realistic awareness. The importance of the seated condyle position is well documented with extensive literature on condylar sag in surgical cases, relapse with functional appliances, mandibular positional changes with rheumatoid and degenerative arthritis, and generally unstable occlusions associated with unseated condyles. Treating patients to unseated condyle positions has consistently led to treatment failure. We do not need to beat this subject to death any longer. On the other hand, in our zeal to provide a seated condyle position, we have at times placed the condyle in a compressed position. There is a growing body of evidence showing that condylar compression leads to local or even total condylar remodeling. Therefore, the goal is to place the condyle in a seated but uncompressed position. This is not the easiest of tasks.
DR. KEIM How do you assure that the condyles are in this position during record taking?
DR. MCLAUGHLIN For bite registration, the patient is seated in the chair at approximately a 45° angle. The mandible is manipulated with gentle seating pressure, using the thumb on the chin and two fingers under each side of the mandible. Once this has been practiced with the patient, the initial wax bite is taken. The selected wax is a sheet of medium-hardness pink baseplate wax, folded in half and then folded again to 1cm width in the incisor area (open bites need more thickness in the anterior area). The wax is then trimmed to the general shape of the patient's upper arch. With the wax in place, the patient is closed in the seated condyle position to first tooth contact. The wax bite is removed, and a sharp pair of scissors is used to accurately trim just behind the most distal molars, through the upper buccal cusps, and along the edge of the incisors. This avoids soft-tissue distortion during the next two wax-bite checks and when mounting the models. The wax bite is then repositioned onto the maxillary teeth, and the bite is retaken in the same way. The lower incisors must fit precisely into the incisor indentations. If not, the wax bite is discarded and the process is begun again. This repeated wax bite is removed and chilled in cold water. It is then repositioned and taken a third time. Once again, the lower incisors must fit accurately, or the entire process is repeated. If it is not possible to obtain repeated incisor positioning, then the patient is most likely in need of a phase of splint therapy. Also, if the TMJ examination reveals joint or muscle symptoms, then the patient should undergo a phase of splint therapy. Using the above technique has proven to be the best method of avoiding mandibular positioning errors.
DR. KEIM The role of condylar remodeling in the long-term instability of many cases has only recently been fully understood. Could you speak to this issue?
DR. MCLAUGHLIN The work of Dr. Arnett, Dr. Milam, and others has been very helpful in this area. They often refer to condylar remodeling as the "last frontier" in the TMJ management issue. The book presents an up-to-date discussion of this subject. In summary, condylar remodeling can be local (confined to smaller areas on the head of the condyle) or total (involving the entire head of the condyle). Local remodeling is also being referred to as "functional" remodeling, since it is observed in nearly everyone as a result of normal functioning. With this type of remodeling, ramus height is not affected and the occlusion remains stable. Total remodeling, which fortunately occurs in a small number of patients, is referred to as "dysfunctional remodeling". This is the orthodontist's and surgeon's nightmare, since the ramus height is affected and the bite is unstable. It is also significant for the orthodontist, since it can disturb normal growth and development. Joint stabilization with splint therapy is important for these patients. Also, protocols for medical management of the joint are being developed, and, hopefully, this will allow us to begin improving our ability to help these patients.
DR. KEIM You define three groups of cases: Group 1 is non-surgical, Group 3 is surgical, and Group 2 is borderline cases that could be treated surgically or non-surgically. Where do you draw the line between a Group 2 and a Group 3 case, one that definitely requires surgery?
DR. MCLAUGHLIN It is impossible to draw a clear line between surgical and non-surgical cases. This is due to cultural differences, personal patient preferences, the orthodontist's biases and preferences, financial factors, and availability of surgical treatment. Having said this, the more we can objectively evaluate our cases, the better our decision making will be. The Arnett STCA and CTP protocol allows us to do this. In addition, computerized access to these programs allows us to quickly evaluate cases as orthodontic and/or surgical. Also, options can be presented to the patient in a clear and concise manner, allowing them to participate more fully in these important decisions.
DR. KEIM What do you mean by "double assessment" of the difficult borderline surgical cases?
DR. MCLAUGHLIN Group 1 cases are evaluated only for orthodontic treatment, as they do not present with skeletal disharmonies that require a surgical assessment. Group 3 cases present with such severe skeletal disharmonies that it is readily apparent that an acceptable result cannot be achieved non-surgically. Therefore, these cases are evaluated for surgical-orthodontic treatment. Group 2 borderline cases, which can make up a fairly large group in the orthodontic practice, can benefit from a "double assessment". That is, they can be evaluated for orthodontic treatment only and also for surgical-orthodontic treatment. In the past, this has been a tedious process, and has not been fully completed for most cases. However, the computerized STCA and CTP allow the clinician to do it quickly and accurately.
DR. KEIM Do you handle a Group 2 borderline case that opts for non-surgical treatment differently from a Group 1 non-surgical case?
DR. MCLAUGHLIN These patients are frequently our most difficult cases to manage orthodontically. It is often necessary to move teeth long distances, with added anchorage, periodontal, and instability concerns. Long-term retention is often required. These factors should be carefully explained to the patient, who may alternatively reconsider the surgical option.
DR. KEIM What is the role of the doctor's subjective artistic and clinical judgment in such a system?
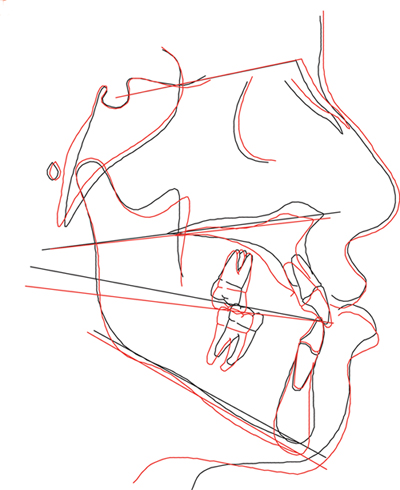
DR. MCLAUGHLIN Clinical judgment comes into play with each part of the clinical examination: the TMJs, the face three-dimensionally, and the condition of the dentition in its entirety. This judgment is also critical in the analysis of all of the records, and is essential in treatment planning of all aspects of the case. Objective norms serve as points of reference to improve our clinical judgment. Also, the doctor's subjective artistic judgment can be coordinated with the patient's concerns to fine-tune and guide the case to a satisfactory completion. The two patients shown on the following pages are examples of how we used facial and dental planning in borderline cases--one Class II and one Class III.
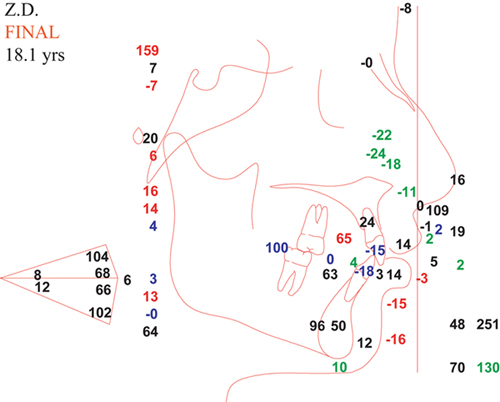
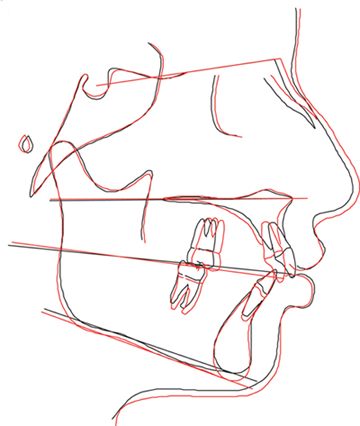
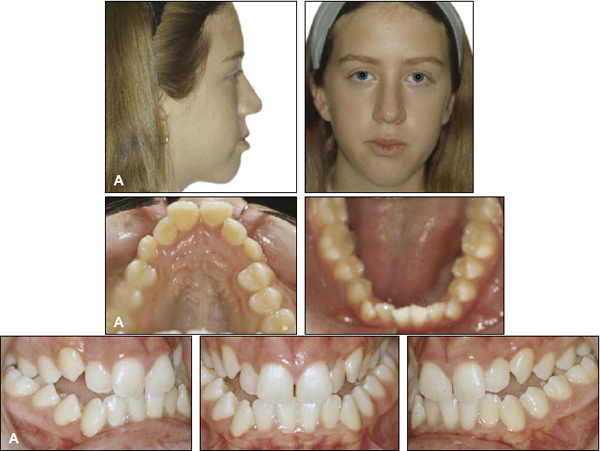
Patient Z.D.
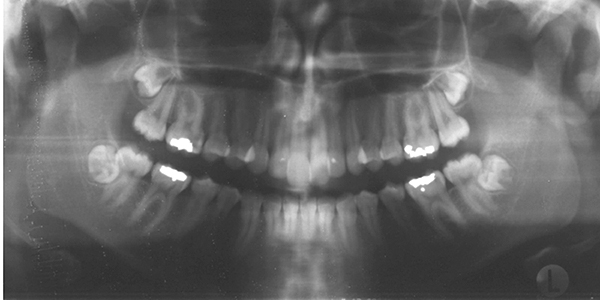
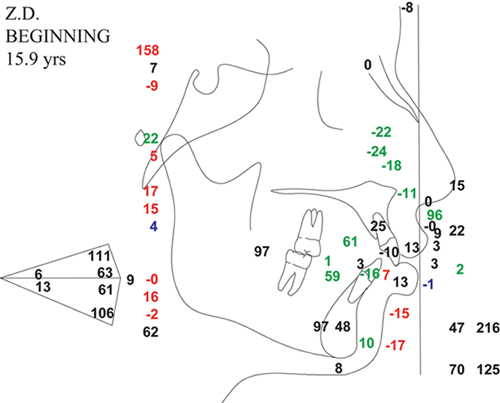
A. 15-year-old female patient with Class II skeletal and dental pattern. Maxillary molars were 6mm Class II on each side. Lower midline was symmetrical, with upper midline 1.5mm left. Lower arch showed minimal crowding, but upper anterior segment was moderately crowded. Panoramic radiograph showed all four third molars impacted. Evaluation indicated that patient could benefit from "double assessment" for surgical-orthodontic treatment and orthodontics only.
B. Arnett Analysis indicated maxilla in normal horizontal and vertical position, upper lip normal in thickness and length, and upper incisors in normal vertical and anteroposterior position, but slightly undertorqued. Mandible was severely retrusive, and lower incisors were proclined.

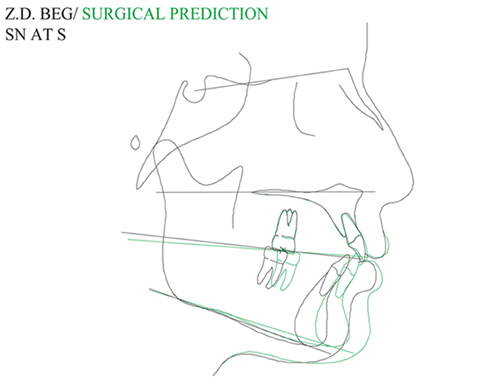
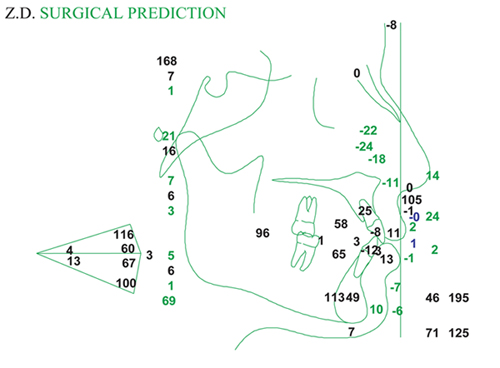
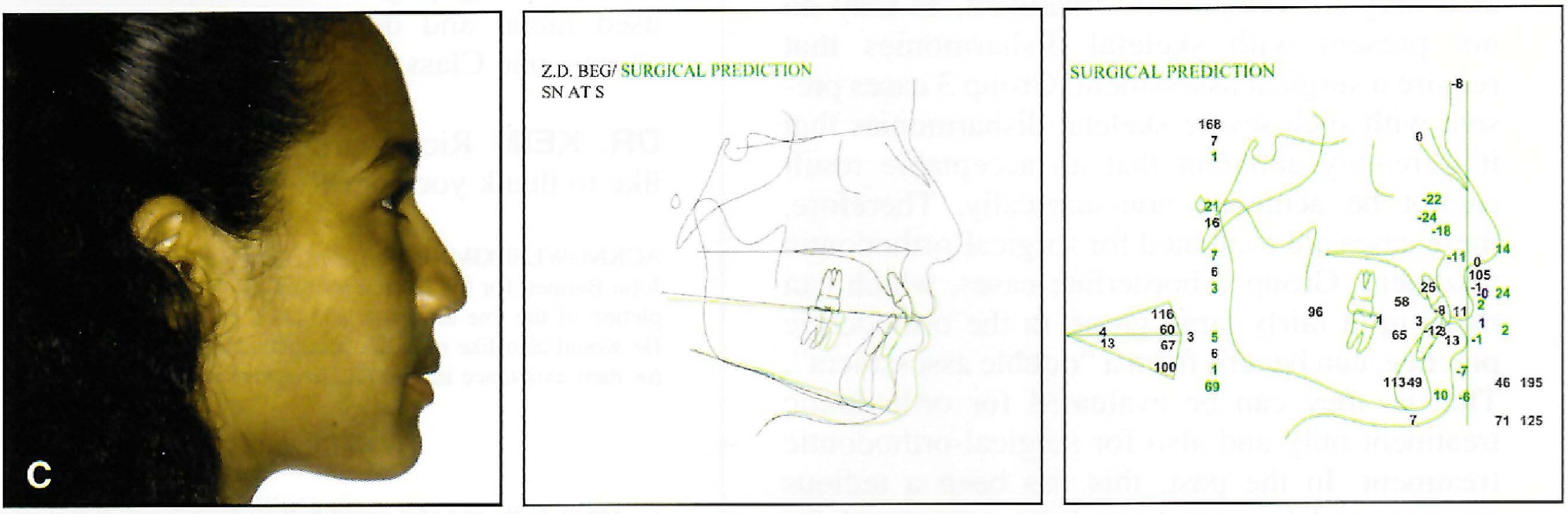
C. Surgical-orthodontic analysis. Both arches could be aligned without extractions using interproximal reduction. Upper incisors could be slightly advanced, and lower incisors uprighted. After orthodontic preparation, mandible could be surgically advanced approximately 6mm. (Surgical prediction SN at S; Surgical prediction, analysis)
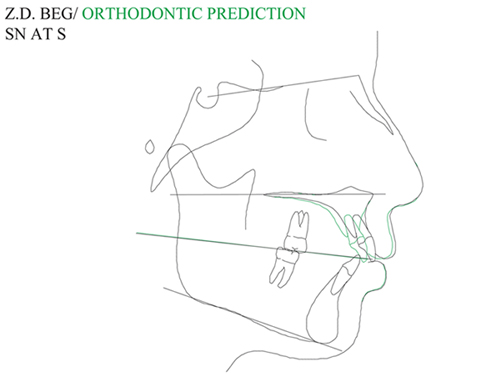
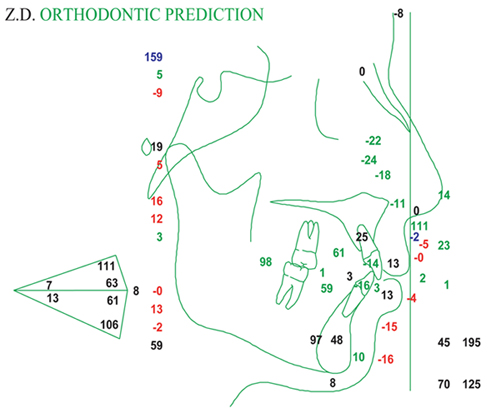
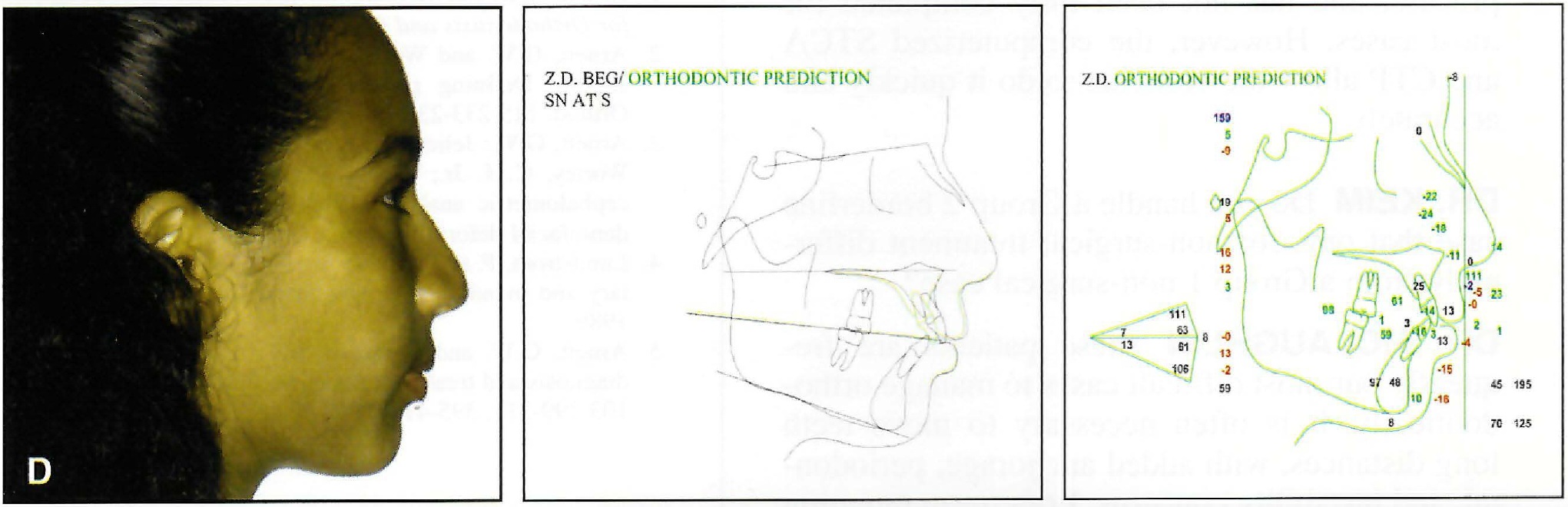
D. Orthodontic analysis. Lower incisors could be left in original positions to contact lower anterior teeth, leaving molars in Class II relationship. This would result in some flattening of upper lip, but with average lip thickness, effect would be minimal. Patient elected orthodontic treatment only, following extraction of upper first bicuspids. (Orthodontic prediction SN at S; Orthodontic prediction, analysis)
E. Patient after 28 months of treatment; note small spaces remaining in upper extraction sites due to small upper lateral incisors and second bicuspids. (Final analysis; Superimposition; Final panoramic radiograph)


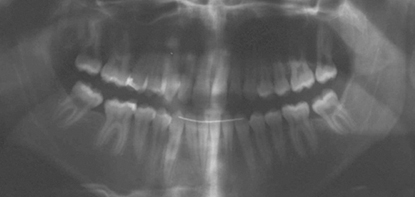
Patient R.C.
A. 14-year-old female patient with Class III skeletal and dental pattern. Posterior segments were about 4mm Class III on each side. Patient had narrow maxilla and bilateral crossbite. Lower anterior segment showed 7mm of crowding. Only lower third molars were present. Evaluation indicated that patient could benefit from "double assessment" for surgical-orthodontic treatment and orthodontics only. (Initial panoramic radiograph)
B. Arnett Analysis indicated slight midface deficiency and slight mandibular prominence. Maxillary occlusal plane was steep, and lower incisors were extremely upright.

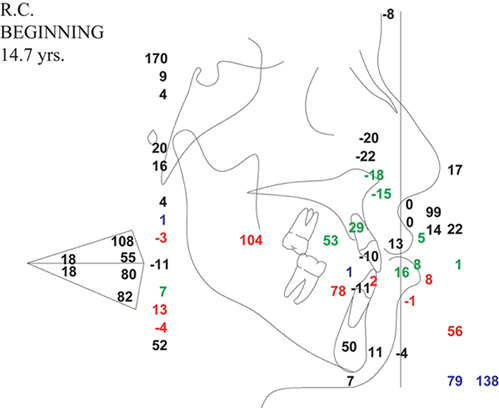
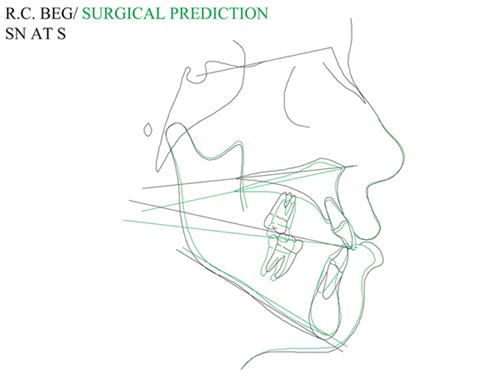
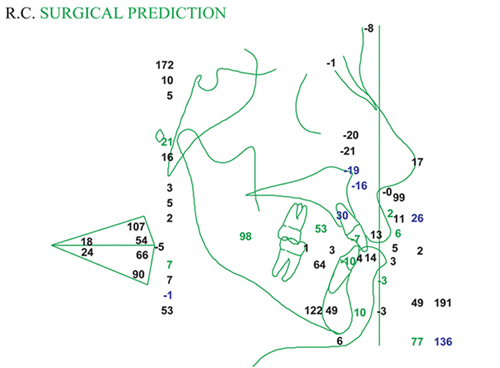
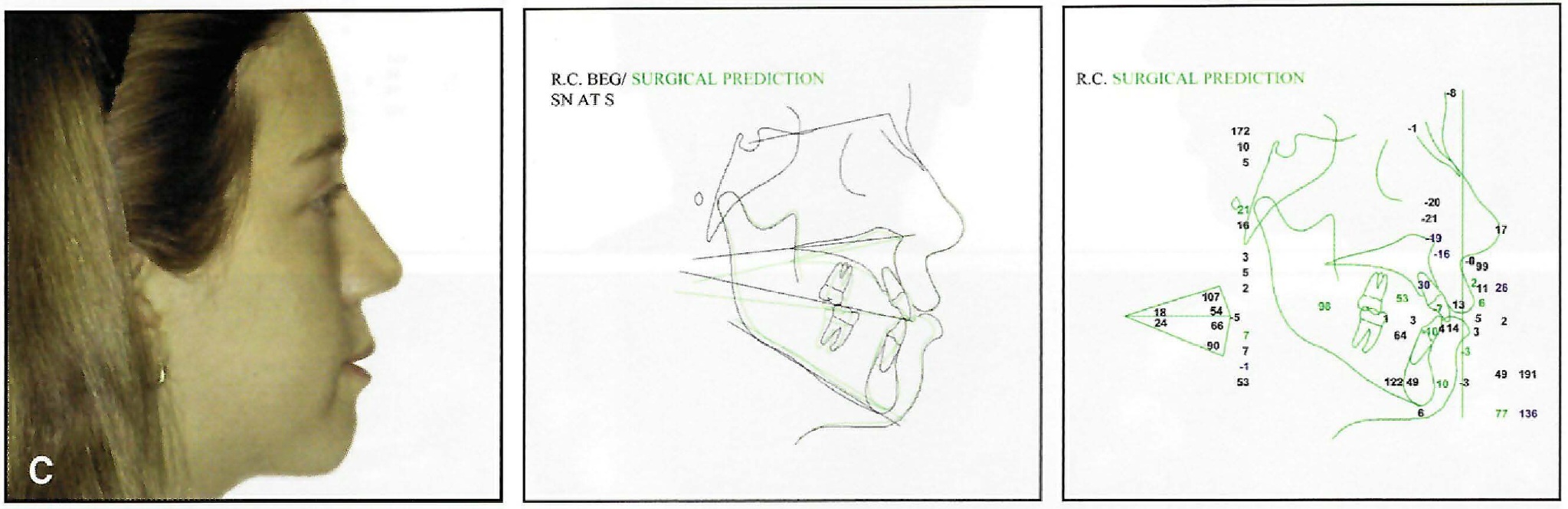
C. Surgical-orthodontic analysis. Presurgical orthodontics would consist of rapid palatal expansion, followed by arch alignment without extractions, along with advancement of lower incisors and some interproximal reduction in lower anterior segment. When patient's growth was complete, two-jaw surgery would be performed with slight maxillary advancement, flattening of maxillary occlusal plane, and mandibular setback. (Surgical prediction SN at S; Surgical prediction, analysis)
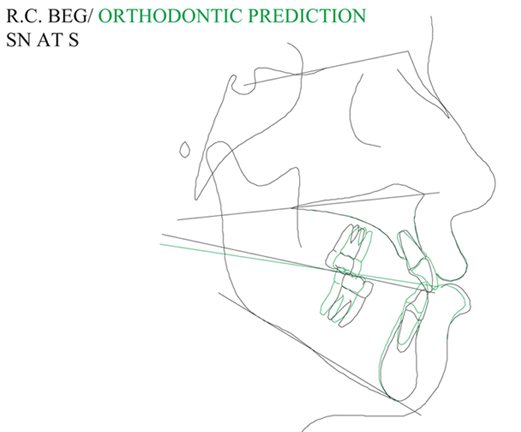
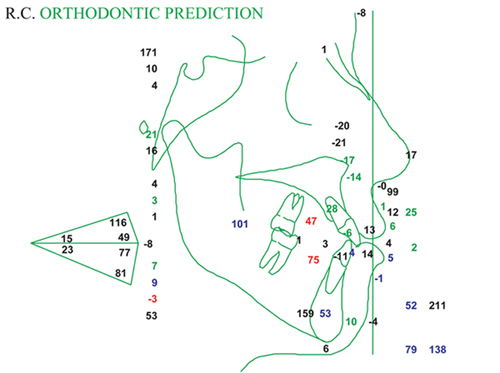
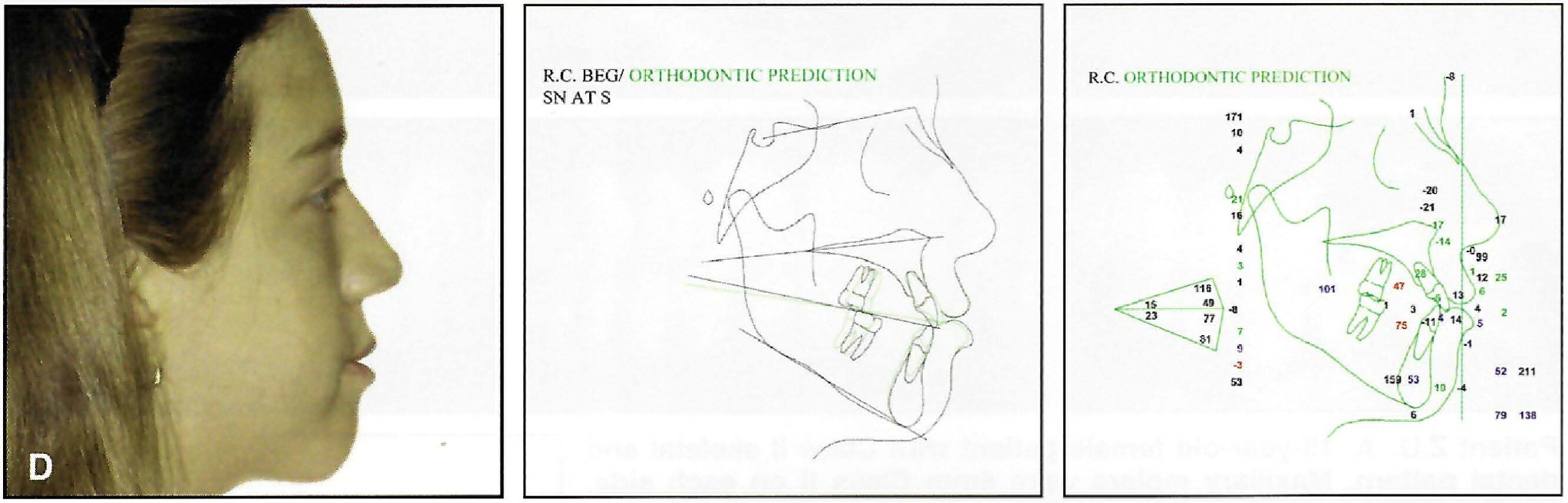
D. Orthodontic analysis. Maxillary arch would be expanded and upper incisors advanced, allowing alignment without extractions. Mandibular crowding and lack of overbite created greatest challenge. Nonextraction treatment would result in lower incisor advancement and unacceptable overbite and overjet. Extraction of lower bicuspids was considered, but would create 14mm of space to offset 7mm of crowding, limiting need for Class III elastics. Decision was made to extract second molars, allowing Class III elastics to be used to retract lower dentition and extrude lower incisors. (Orthodontic prediction SN at S; Orthodontic prediction, analysis)
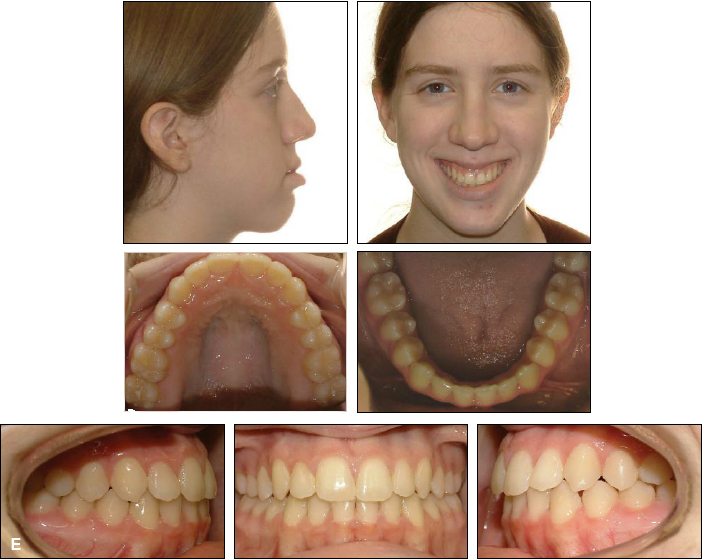
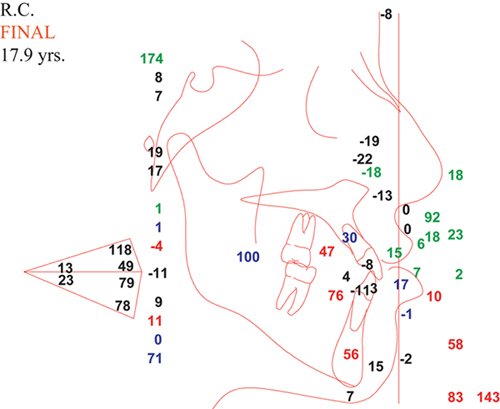
E. Patient after 38 months of treatment. (Final analysis; Superimposition; Final panoramic radiograph)
DR. KEIM Rick, on behalf of our readers, I'd like to thank you for this discussion.
ACKNOWLEDGMENTS: Dr. McLaughlin would like to thank Dr. John Bennett for his help in writing the book, as well as his completion of the line drawings and coordination with the publishers. He would also like to thank Michaele Carnahan and Patty Knecht for their assistance in his and Dr. Arnett's office.