MANAGEMENT & MARKETING
Creating the Compliant Patient
Without patient cooperation, few medical or dental therapies will achieve optimum results. The key to success is to discover the actions that will produce the most positive response from the patient. In the June 1996 issue of JCO, Dr. Larry White presented "A New Paradigm of Motivation". In this month's column, four members of the Alexander family discuss the hows and whys of "Creating the Compliant Patient".
The department chairman at Northwestern University during my orthodontic residency, Dr. John R. Thompson, said that "if all we give the young people in our care is the correct bite and an excellent smile, we haven't been truly successful". The Alexanders feel the same way. They describe in detail their approach to turning around a non-compliant patient. If this condition is a cry for help, then we, as caring professionals, should recognize it and respond. We may be the patient's only source of positive reinforcement.
The authors also elaborate on three requirements for creating the compliant patient: belief in one's technique, communication, and motivation. One excellent piece of advice is that the giver and receiver of information should be at the same eye level. Since most orthodontic adjustments are made with the patient in a relatively prone position, instructions are usually given with the doctor or assistant above the patient. Talking down to someone from a position of superiority is not a good way to communicate.
Similar articles from the archive:
Another important factor mentioned by the Alexanders is the office environment. If everyone in the practice is convinced that the service being performed is the best, then a relaxed attitude of warmth, caring, and concern will be conveyed. This atmosphere must be present from the first appointment to the dismissal. In addition, everyone involved in treatment must be open to two-way communication. There is nothing that will discourage a patient more than evading a legitimate query.
The last topic covered in the article is dealing with a persistently non-compliant patient. No matter how much effort we put into convincing patients of the benefits of our treatment, we must all be prepared for this eventuality.
I enthusiastically urge readers to carefully examine the Alexanders' article. Their points are concise, salient, and practical. As their motto says, "Effort equals result".
MELVIN MAYERSON, DDS, MSD
Creating the Compliant Patient
Today's orthodontist seems focused on how to treat the non-compliant patient. Appliances such as the Herbst*, the Pendulum**, nickel titanium coil springs, and magnets can be helpful in certain Class II cases, but using them simply to remove responsibility from the patient could compromise the treatment plan.
Unfortunately, many Americans fail to take responsibility for their actions nowadays. Words like effort, responsibility, and discipline may not be fashionable, but they should be included in the basic patient education program of any orthodontic practice. As clinicians, we have the privilege of letting our patients accept personal accountability, see the results, and succeed.
Goals of Orthodontic Treatment
We all agree that the goal of orthodontic treatment is a high-quality finished result. The reality, however, is that different practitioners have different objectives and different perceptions of quality. What constitutes a balanced profile, the proper position of the lower incisors, and the desirable amount of buccal expansion are all controversial issues about which orthodontists have varying opinions.
The first requirement for creating a compliant patient is that the clinician must believe in his or her technique, whatever it may be. Kenneth Cooper says, Your beliefs are the most powerful motivational tools you have if you can just learn how to use them.1 Keeping treatment simple and executing a step-by-step plan will make explanation and monitoring easier.
Patient Education
The second requirement is that the patient and parents must understand exactly what to do and why it is important (Fig. 1). They need to know the costs and benefits of treatment, in time, money, and effort. This education takes time staff time and doctor time. Although efficiency experts like to talk about saving time, we really can only spend time. The question is how to spend our time most effectively.
Thorough patient education at the beginning of treatment can eliminate many problems down the road. We must inform before we perform (Fig. 2). This means more than a monotone recitation of a set of instructions. We need to enjoy making new friends of patients and parents or at least act as if we enjoy it.
Contemporary orthodontic materials and techniques allow many treatment procedures to be taught and delegated to staff members, freeing up time for the doctor to talk to and educate patients and parents. The words we use and the tone of voice make important sound bites that can inspire and motivate.
Patient Motivation
The third requirement for creating a compliant patient is the ability of the doctor and staff to motivate the patient. In the words of William James (sometimes called the father of American psychology), The most important discovery of the 20th century is that the attitudes of an individual can change.2 He was right.
The lesson to learn from studying motivational techniques3 is that the only truly successful method is self-motivation. Rah-rah speeches usually fall on deaf ears. To be effective, motivation must be internalized. The key, then, is to determine what approach will empower or push the button for each individual.
Every practitioner knows that patients' degree of self-motivation can vary substantially. Those who come from stable families with supportive parents seem to be the same ones who wear their headgears and keep their teeth clean. These patients receive strokes from their parents, friends, teachers, and others. But not all patients are cheerleaders or student council presidents. Our challenge is to relate to the patient with low self-esteem the typical non-compliant patient.
How often do doctors and staff members react negatively when such a patient enters the operatory? "Here comes Tommy. Let's get him in and out as quickly as possible." The reaction should be exactly the opposite! Here is a young person who really needs our help. He could be from a broken family, always getting into trouble at school, mixed up with the wrong crowd, perhaps wearing strange clothes and a funky hairstyle. He probably has poor oral hygiene, hasn't worn his appliance, and expects to be reprimanded as soon as someone looks into his mouth. It is difficult to be non-judgmental in such a situation, but we do have a choice.
Fig. 1 Patient education booklets, used to reinforce instructions throughout treatment, are written in positive tone to encourage and motivate patients.
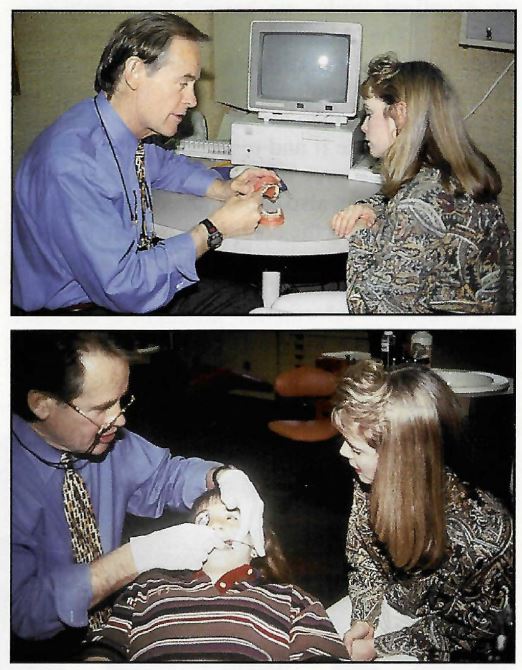
Fig. 2 Procedures and appliances explained to patient by Dr. Wick Alexander before treatment.
Stephen Covey describes the "space" between stimulus and response.4 In this space, he says, lies our freedom to choose how we respond. For example, when a car cuts in front of us (stimulus), our instantaneous thought or attitude (space) will determine our action (response). The stimulus cannot be changed, but our attitude can change. It takes practice and forethought to anticipate how to fill that space. In defensive driving, we are taught how to "watch out for the other guy". The same process occurs with the non-compliant patient.
The orthodontic office may be one of the few positive influences on this child's life. If he can receive positive strokes from the doctor and staff while learning to accept individual responsibility, his attitude might be altered. Picture the patient with a sign around his neck that says "Make me feel important". This approach is self-serving in that a better attitude will help the patient follow instructions and presumably lead to a better treatment result. If successful, however, it could give him a foundation on which to build other positive experiences.
Office Environment
Every office reflects the personality of the orthodontist. If you want to find out how your office "personality" is perceived, ask a sales representative who visits periodically. The key is to create a positive environment that fits within your personal comfort zone. In our practices, the goal is to maintain a friendly, relaxed, warm, caring, professional atmosphere in which patients know that they will receive the highest-quality treatment and that we also expect the best from them. Thus, we are building offices full of achievers.
A good office environment helps create the compliant patient through non-verbal motivation. Motivational signs can be seen throughout our offices. On the wall next to the entrance is a sign with our motto: "Effort Equals Result". This theme, taken from James Allen's quotation, "In all human affairs, there are efforts and there are results, and the strength of the effort is the measure of the result",5 is carried throughout the office for staff members as well as patients.
In keeping with our desire to create a friendly environment, a "hi-bye" policy is in effect. Patients' names are written in large letters on their charts so that everyone can greet them by name when saying "hello" and "goodbye". The most beautiful sound in the world is the sound of a person's own name.
Communication Techniques
Most patients open their mouths as soon as the orthodontist sits down at the chair. An effective communication technique is to look in their eyes before you look in their mouths (Fig. 3). This simple act helps us remember that we are dealing with human beings, not typodonts. You must have patients' well-being in mind to be able to motivate them.
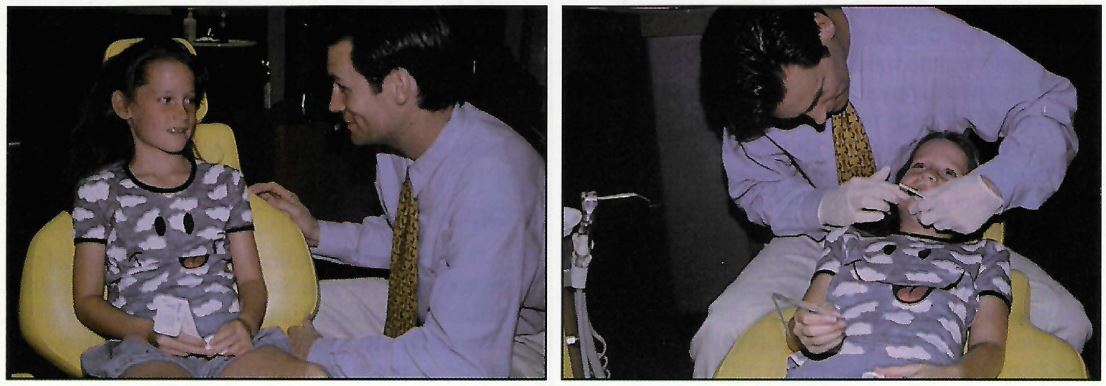
Fig. 3 "Horizontal communication": Dr. J. Moody Alexander looking in patient's eyes before looking in the mouth.
Always keep the conversation on a personal note: school, sports, music, or whatever activities the patient is involved in. Assume that every patient is a star; find out where he or she shines, and write it on the chart. Try to get an idea of what is going on in the patient's personal life. Is it a single-parent family? Is alcohol or abuse involved? How can we really help this person?
It is critical to communicate horizontally rather than vertically. Avoid situations in which your eye level is above that of the patient.
Good communication should be honest as well as two-way. The orthodontist should be "askable". After explaining a procedure, always ask, "Do you have any questions?" Then listen! Active listening is not easy. Look the patient in the eye, nod agreement, repeat key phrases, and be willing to change your mind depending on what the patient says.
Monitoring Progress
Each patient's progress must be monitored constantly to maintain motivation and compliance throughout treatment. Achievable short-term goals, such as a reduction in overjet, are essential. When improvement is seen, praise the patient and share the achievement with the parent. We award an Eisenhower silver dollar when a patient receives three "plus" grades for excellent oral hygiene.
Some patients will inevitably fall behind in treatment. If it is not the patient's fault, as with slow eruption of the permanent teeth, this should be explained and treatment continued as usual.
If slow progress is due to non-compliance, it is crucial that the patient and parents be informed as early as possible in a "mini-consultation". Both parents should be present for this appointment if possible. At the consultation, set goals that are clear and attainable. It might be necessary to compromise to achieve some form of success--"if you wear elastics full-time, you can stop the headgear". Try every motivational technique you know, take accurate notes, and follow up with a letter to the parents.
A few patients will fail to respond despite all our efforts. If compliance problems persist, schedule another meeting six months before the estimated end of treatment, again with both parents on hand if possible. Present four options:
- The patient gives ultimate effort with headgear and elastics to achieve the treatment goals.
- The headgear is tied in, or the patient is switched to a "non-compliant" appliance such a Herbst or coil springs.
- Treatment is continued and appliances are removed as originally scheduled, after the parents sign a release letter.
- Treatment is continued past the scheduled point, with an additional monthly fee, until a successful result is achieved.
Since the parents have already invested a considerable sum, it is not fair to expect them to pay more. Many patients choose to put some of their own money into completing treatment. This option is provided in our Individual Responsibility Agreement, which is signed by every patient in front of the parents at the initial consultation. Most patients, however, elect to put more effort into completing treatment on time.
Conclusion
Creating the compliant patient begins with the attitude of the orthodontist. We are in the "people" business. Our goals will be achieved if we believe in our delivery system, properly educate our patients, and learn how to motivate them to follow instructions. This kind of communication takes time, but the results are well worth it.
"Non-compliant" appliances have their place in the orthodontic armamentarium, but they should not be viewed as a means to solve all our problems. If they were, there would be no need for patients to maintain good oral hygiene, take care of their appliances, keep appointments, and do all the other "little" things that make treatment successful.
John Naisbitt summed it up with this statement: "In our minds, at least, technology is always on the verge of liberating us from personal discipline and responsibility. Only it never does and never will."6 Patients must still cooperate in all areas if we expect to produce consistent high-quality results. The law of cause and effect hasn't changed--effort still equals result.
Editor's Note: We would like to thank the Center for Human Growth and Development at the University of Michigan for allowing us to publish this slightly condensed version of the authors' material in advance of the Craniofacial Growth Series monograph on the 1996 Moyers Symposium.
FOOTNOTES
- *Registered trademark of Dentaurum, Inc., 10 Pheasant Run, Newtown, PA 18940.
- **Ormco, 1717 W. Collins Ave., Orange, CA 92667.
REFERENCES
- 1. Cooper, K.: It's Better To Believe, Thomas Nelson, Inc., Nashville, TN, 1995.
- 2. Peale, N.V.: Words I have lived by, in My Favorite Quotations, C.R. Gibson Co., Norwalk, CT, 1990, pp. 5-6.
- 3. Waitley, D.: The Psychology of Human Motivation, cassette tapes, Nightingale Conant, Niles, IL, 1991.
- 4. Covey, S.R.: First Things First, Simon and Schuster, New York, 1994.
- 5. Allen, J.: As a Man Thinketh, Hallmark Cards, Inc., Kansas City, MO, 1968, p. 57.
- 6. Naisbitt, J.: Megatrends: Ten New Directions Transforming Our Lives, Warner Books, Inc., New York, 1982, p. 53.





