Editor's Note: The following article is a response to the Editor's Corner, "Concepts to Live By", by Dr. Fred F. Schudy (JCO, March 1993).
The Editor's Corner contained many statements and concepts presented as convictions for clinical practitioners "to live by". Certain challenges to some of those maxims would seem to be indicated on behalf of present and future generations of orthodontists. The adamant stand taken by the author on some issues particularly needs to be assessed. Responding views are important in light of differing theories held in worldwide movements of current orthodontics.
I will address the seven statements in the editorial one by one.
1. "Molars do not intrude."
It was denied that the muscles of mastication can exert an intruding effect on molars through function. In other words, the author believes the closing jaw muscles are not strong enough to exert an intruding pressure. This statement needs to be challenged from several aspects.
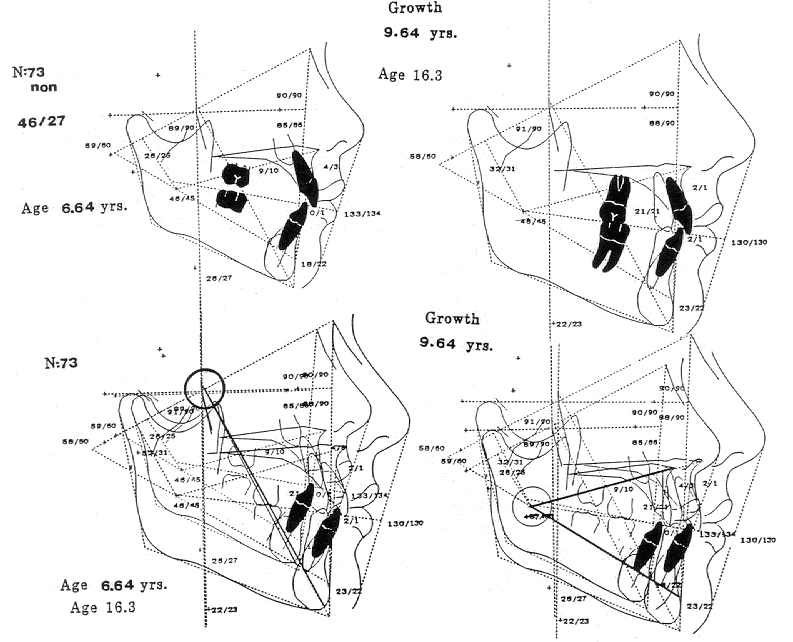
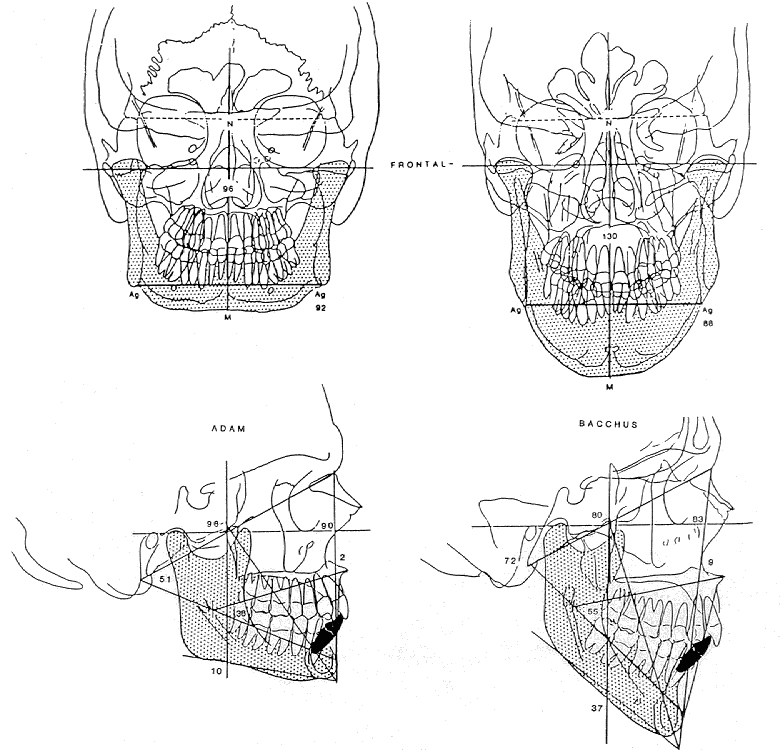
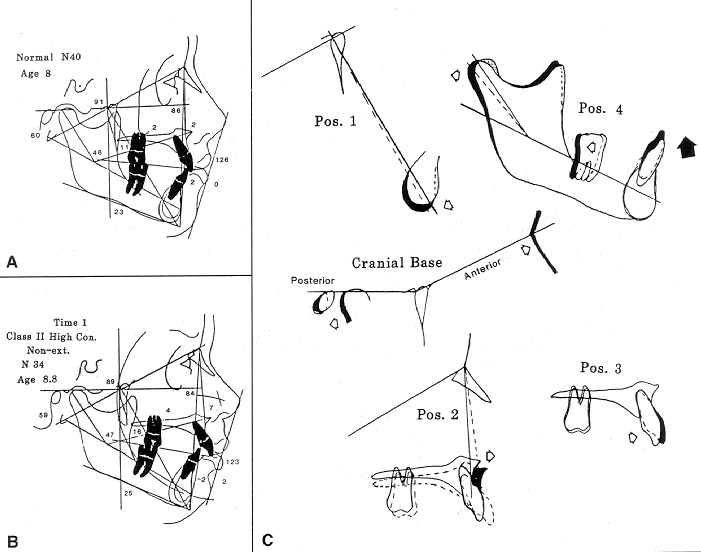
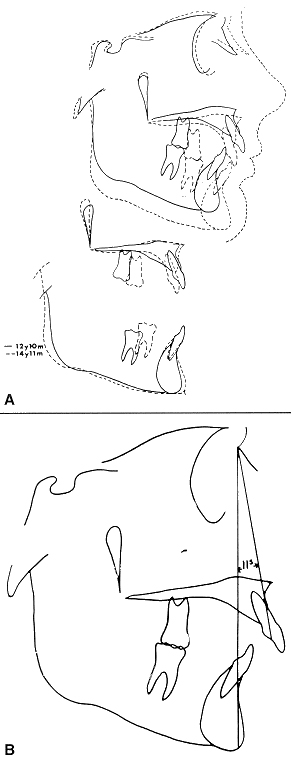
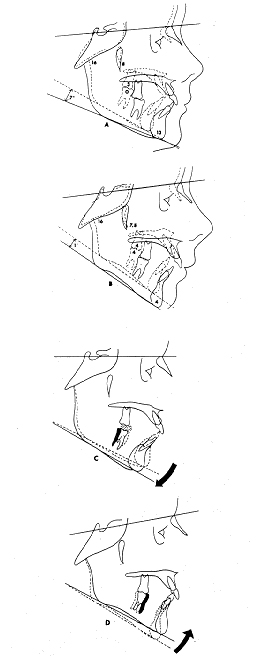
As a background, we must consider the factors of normal eruption, and particularly the most appropriate basis for superpositioning. Certainly, as the growth turgor of the mandible is expressed, and as facial development occurs, greater intermaxillary distance is created. In general, all teeth erupt into the space developed as the jaws grow apart (Fig. 1). Consequently, the molars continue to erupt until growth is completed (unless impeded by the tongue, as observed in posterior open bite).
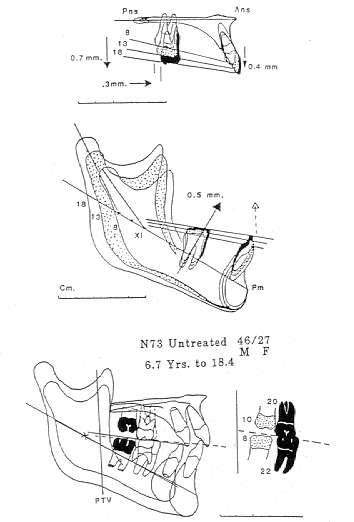
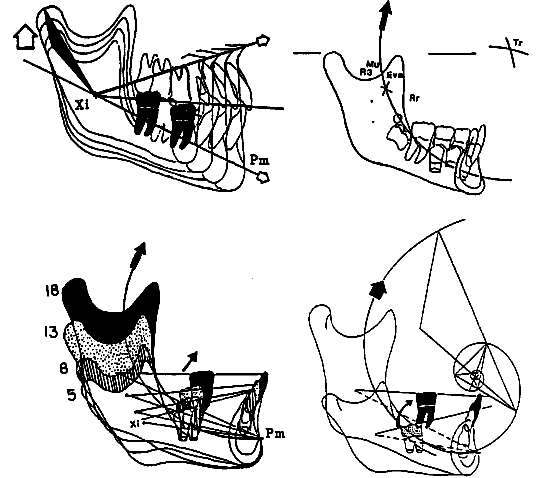
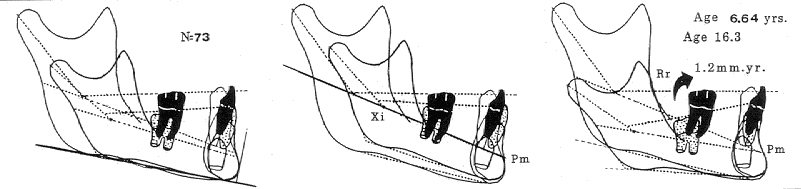
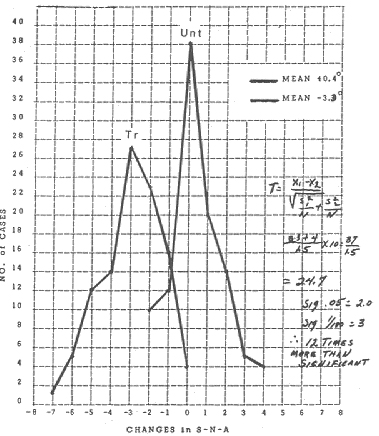
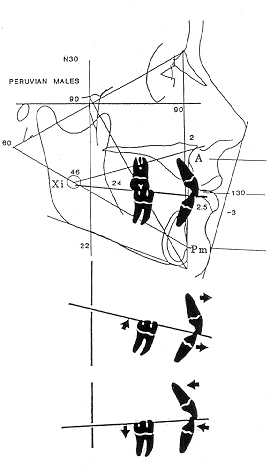
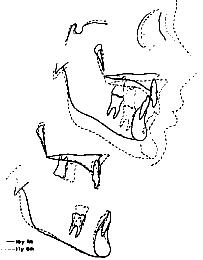
Recent findings indicate that the lower first molar erupts from the corpus axis a mean of nearly .5mm per year. The upper first molar erupts a mean of .7mm per year from the palatal plane (Fig. 2). On the mandibular growth arc, however, the whole arch moves upward and forward. As viewed biologically, the first molar erupts about 1.2mm per year in a vertical direction (Figs. 3 and 4).
Furthermore, it is clear that in longer faces, as greater-than-average vertical development occurs, the teeth compensate by filling in the additional space until they encounter muscle resistance to their eruptive force (Fig. 5).
One can estimate, on the basis of animal studies1 and clinical findings,2 that the pressure of eruption is .2 grams per square millimeter of en-face root surface. This would place the eruptive capacity of each of the first molars, upper and lower, in the range of 20-25g. Theoretically, any continuous magnitude of force in this range would essentially inhibit molar eruption. Any greater continuous pressure would produce an intrusion, as estimated from a starting force of no more than 80g for clinical practice. Such forces are easily within the limits of the muscles of mastication, which is measured in kilograms.
For many years, gnathologists have opened bites by placing overlays on the posterior teeth. In some patients, the vertical height increase was maintained. But many collapsed over a period of time, until nearly the original morphologic face height or vertical dimension was re-established. Because many practitioners did not appreciate the value of oriented headfilms for investigation and clinical monitoring, the relapse was often explained by referring to teeth other than the molars as the basis for intrusive action.
Many practitioners, particularly in the 1970s and 1980s, used overlay posterior splints as advised by prosthodontists. Certain techniques prescribed a splint over the posterior teeth, with or without advancement of the mandible for correction of condylar position. Many of these patients, in the absence of immediate cures, wore such "splints" for more than a year--some as long as three years or more. Careful study of such patients indicated that the posterior teeth were intruded, often together with extrusion of the anterior teeth, thus producing a much worse bite condition than before the splint was worn.
Certain patients have experienced intrusion of the posterior teeth even with full coverage of the lower arch, as in the "biotemplate" technique. This apparently occurs from an attempt to move the condyle away from the postero-superior border of the glenoid fossa (Fig. 6). One such instance would be merely anecdotal, but when this kind of intrusion is observed in many patients, even the most extreme skeptic must take notice.
Additionally, overlay spring plates have been seen to intrude the molars during the treatment of anterior open bite.3,4
Of great importance to this issue is the behavior of the lower molars during cervical traction of the upper molar in the correction of Class II malocclusion. There is, of course, a vertical component to cervical traction that prevents molar tipping. As a result of abuse of this technique, many clinicians became overalarmed. If heavy, continuous forces are exerted on a 20-or-more-hour-a-day basis with cervical traction, the muscles of mastication will often be overcome. This behavior has been described as the "wedge effect".
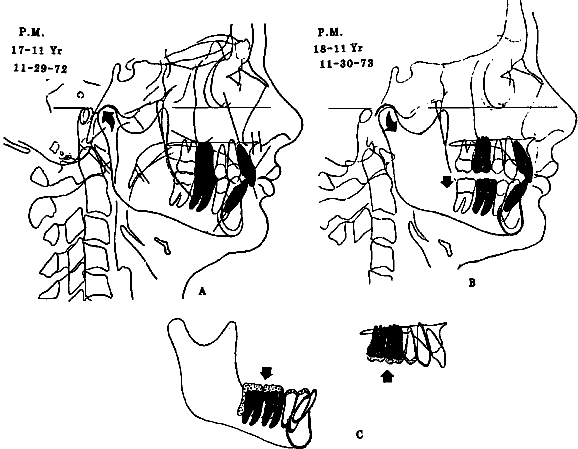
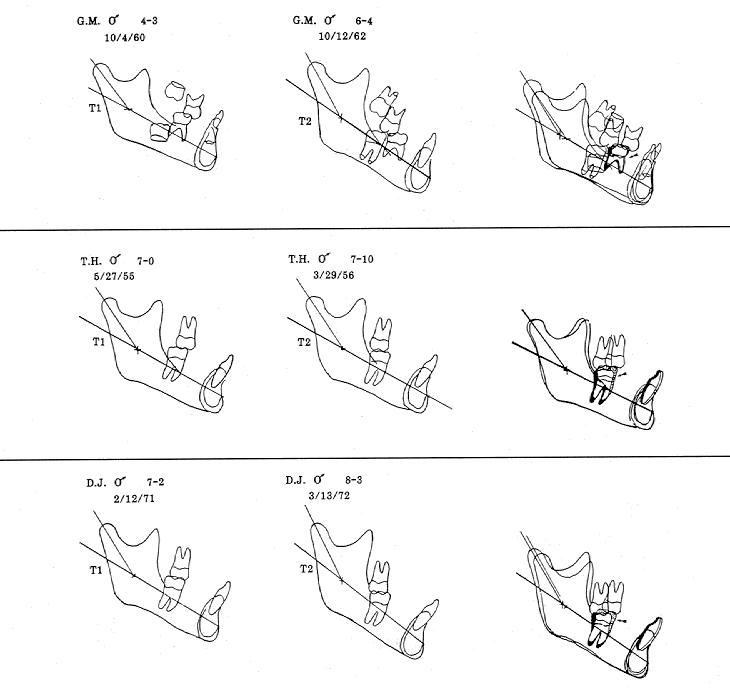
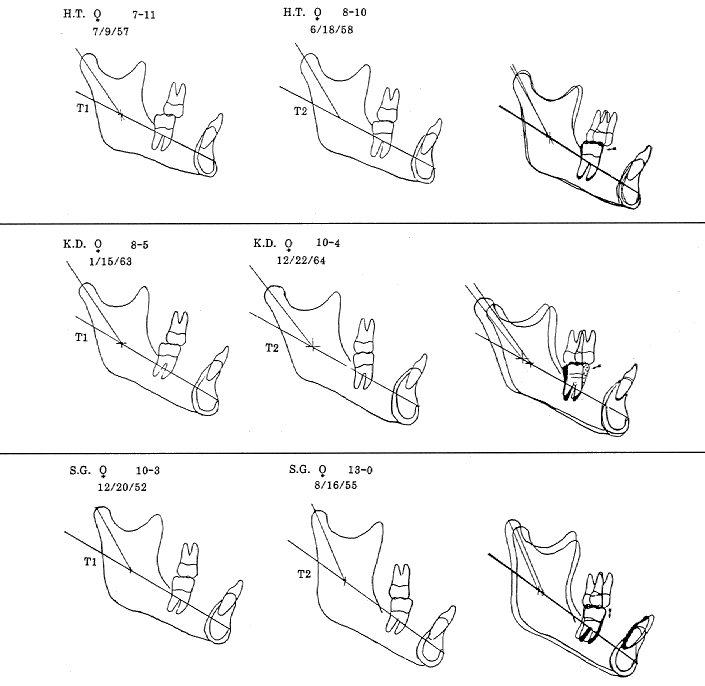
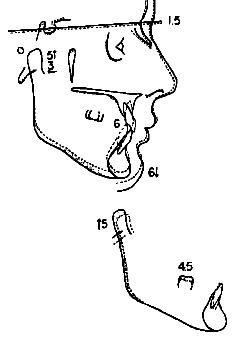
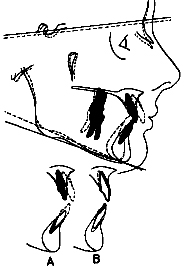
However, if forces do not exceed 500g in the mixed dentition (or 350g in the deciduous dentition), and bite plates are not used, and pain has not been overwhelming to the patient, with extrusion of the upper molar the lower molar has been seen to intrude in hundreds of patients. This is not merely an anecdotal finding: six such cases are shown in Figures 7 and 7A. In these patients, the occlusal plane, which originally was located above Xi point, moves downward during treatment to the level of Xi point (or preferably, below it). Measurements from the corpus axis during the period of cervical traction show the lower molar to be decidedly intruded by 2mm or more, when it should have been erupting .5mm per year. This occurs with no appliance on the lower arch. When a utility arch is placed for management of the lower arch, buccal torquing of the roots of the lower molar will produce even further gains in lower molar intrusion or lower molar crown height reduction during cervical traction.
Another technique that was once common with the edgewise appliance was the use of intermaxillary elastics and 2nd-order bends for Class II correction of the upper arch. Some practitioners would withhold engagement of the lower second molars until they were sufficiently erupted, while the lower first molar (and entire lower arch) were used for traction. A common finding was that the upper first molar would move superior to the second molar during treatment. It was often assumed that the second molar had simply supra-erupted, but tracings of such cases show the lower first molar to be occlusally positioned relative to the second molar. The pull of the elastics, which exert a vertical force of about 50g, would normally cause the lower molar to be extruded and the upper molar to be intruded, as measured from the palatal plane. Upper molar intrusion from Class II elastics would, of course, occur primarily in patients who do not yield by lowering of the mandible. Therefore, in these patients the forces of mastication intruded the upper molars.
In conclusion, to build an orthodontic philosophy upon the belief that a molar cannot be intruded by the forces of mastication would be a miscalculation.
2. "Management of the vertical growth of the alveolar processes is the primary function of the orthodontist."
This maxim is followed by the statement, "We are not sure at present whether condylar growth can be stimulated." I wonder who the "we" is and what literature is being referred to. There is little doubt at present--and there are numerous references5-7--that the form of the mandible and the behavior of the condyle can be altered in the short term. In fact, there is some evidence that in the short term (meaning the one-year period of treatment), the vertical growth of the condyle at the ramus can also be affected with cervical traction. This can be seen in a greater increase in ramus height during treatment than would have been expected without treatment (Figs. 7 and 7A). Even more important, high-pull traction to the upper arch can intrude the upper molar, with a resultant loss of vertical support of or even compression of the mandible, which would inhibit some condylar and mandibular growth.8
All of these influences--with the possible exception of treatment-induced condylar compression and damage--seem to have a transitory effect. Within three to five years after treatment, mandibular growth is usually, but not always, restored to its predicted size and general form.
The next statement is, "Vertical growth of the posterior portion of the maxilla cannot be stimulated or inhibited." It is true that it is difficult to get a handle on the body of the maxilla from a purchase on the teeth, which are held in the alveolar process. But it was discovered 40 years ago that the pterygomaxillary fissure could not be used as a reliable longitudinal reference, because it underwent a change in configuration during treatment. This prompted the selection of a pterygoid reference (Pr) at the posterior margin of the pterygopalatine fossa for the construction of a coordinate grid using the Frankfort plane and the pterygoid vertical (Fig. 1).
Although maxillary alteration had already been demonstrated,9 the entire profession was awakened to the possibility of maxillary orthopedic correction with the introduction of the reverse headgear or face mask, especially as combined with maxillary disjunction appliances. Movement of the entire upper jaw complex, including the intermediate bones, has been demonstrated beyond any shadow of a doubt.11,12 Recent 10-year findings suggest that maxillary alteration, contrary to mandibular alteration, can be permanent (Fig. 8).
In conclusion, the assumption that control of the alveolar processes is the sole possibility for vertical orthodontic management of the growing child is consistent with an ideology that will eventually become a relic of the past.
3. "Growth prediction is based on average growth, and average growth needs no prediction."
This is an old, worn-out cliche that has been used for years to suggest that a clinician need not become knowledgeable about growth or about the mechanism by which it can be directly applied for correction of a malocclusion. In fact, without some concept of growth prediction, the orthodontist has no idea whether changes have been accomplished by treatment or by natural growth.
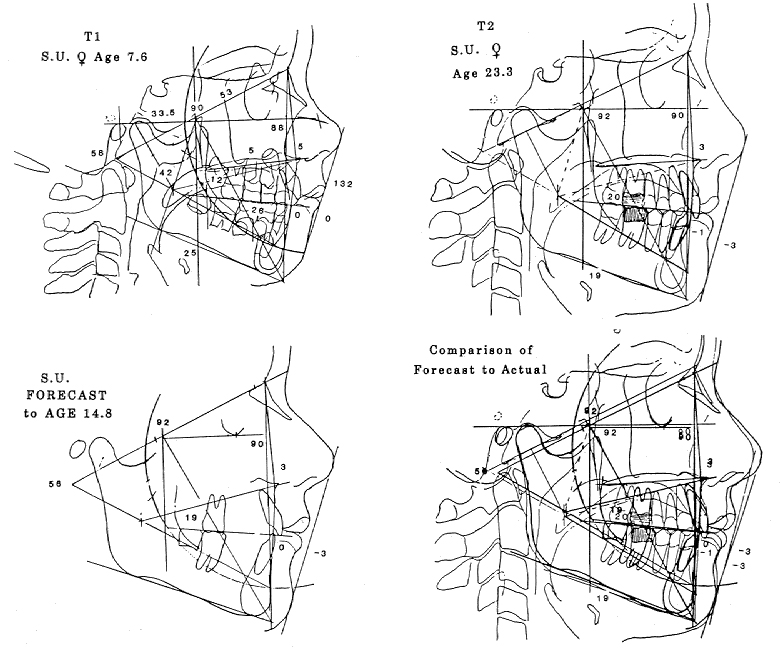
In a recent sample of 73 untreated children followed through 10 years of growth, three patients experienced spontaneous correction of their Class II malocclusions. In all three cases, the skeletal growth pattern was predicted successfully (Fig. 9).
Any seasoned orthodontist has experienced minor Class III malocclusions that have grown into cases requiring surgery. Even treated Class I subjects have been seen to develop Class III conditions with later growth. Proper forecasting techniques can show that these patterns were predictable if the patient later becomes dissatisfied. Other conditions, such as a progressive open bite or an open bite that refused to close, can similarly be attributed to a growth pattern as opposed to iatrogenic results of orthodontic treatment.
The short-range forecast, based on a projection through the joint, was developed in 1950. The first test of the so-called Visualized Treatment Objective (VTO) was run in 1955. In that study, the growth and behavior of the mandible were forecast within clinically desirable limits in 52 of the 55 patients--a 96% accuracy.13 The maxilla was missed because of its alteration with treatment. Had orthopedic action on the maxilla been known at the time, the forecast would have been equally successful with the maxilla, because the forecast included both the treatment objective and the possibilities of specific modalities.
In 1971, following a six-year computer study, the mandibular arc of growth was first reported14 (Fig. 3). Mean values were suggested only as a starting matrix for use of this arc in forecasting. Allowances could then be made for sex and individual morphologic characteristics within the mandible. Consequently, the development of the mandible could for the first time be reliably predicted in the long term (to maturity). The next step was to fit the forecast to an adult face.
Continuous improvements were made in building the cranial base and the midface around a predicted mandible. Adjustments were made in the forecasts for the skull base. The results were quite spectacular: not all, but the great majority, were within clinical limits for treatment designs.
In 1990, an extensive study was made of 133 patients from childhood to maturity. Growth predictions in that study were far more accurate than the intellectual climate in orthodontics was willing to accept. The reason was that the predictions were not based on averages, but on typical behavior when certain characteristics in the mandibular and structural morphology were already present. They were corrected for age and sex as well. Have detractors of the forecasting principle given this technique a try, or even opened their minds to the possibility of its benefits?
Cephalometrics itself lacks absolute certainty, and its proper use takes sophistication. If a VTO or VTG (Visualized Treatment Goal to maturity) is constructed, the idea of "beginning with the end in mind" will easily demonstrate whether "increments of growth" are attributable to the condyle, the mandible, the body of the maxilla, the maxillary alveolar process, or the mandibular alveolar process, as the author of the editorial desired. It should also be pointed out that "metapositioning" after treatment in the long term is not limited to relapse of the treatment itself; many changes can be favorable.
In 1990, 57 uses of the long-range forecast were listed in five categories: communication, growth and orthopedic attention, growth contribution-orthopedic correction, basis for detailed planning of mechanics, and prognosis of retention problems. I would suggest that orthodontists investigate further the biology of growth, rather than think of orthodontics as adjusting sticks on a platter. It is unfathomable why anyone would make the statement that "average growth needs no prediction", when what is average is not what would be expected of any particular individual. Such a statement leads to utter confusion. Why would our institutions research or teach growth if it were not to be applied or had no value?
4. "Lower incisors should not be intruded to level the arch in growing patients."
The logic of such a statement lacks any precision whatsoever. This is an issue that has been debated for at least 30 years. At first, many in the field adamantly contended that intrusion of the lower incisor--or of any tooth--was an impossibility. After it was demonstrated with utility arches and other appliances that lower incisors could be intruded, the theme turned to "even though you could, you shouldn't".
When composites are compared to controls of normals (corrected for age, size, and sex), it is easily observed that in most deep bites, the lower incisor is in supraversion. In deep-bite Class II conditions with high convexity, the lower molar is near normal and all the other teeth are in abnormal positions (Fig. 10). The question could be asked: If the lower incisor segment is in an extruded position, why intentionally elevate the premolars to such abnormal positions? But of even greater concern, an increased elevation of the premolar tends to rotate the mandible backward, which worsens the Class II condition (Fig. 11). Such rotation, theoretically at least, could even compress the condyle and inhibit growth. The prohibition of lower incisor intrusion, therefore, lacks sophistication in light of present knowledge.
The lower incisor can be successfully intruded. When proper upper incisor position and interincisal angles are restored, and when normal function is established, the relationship will hold. Cases with lower incisor intrusion were demonstrated to be stable 30 years ago. The utility arch was developed in 1960, and many other modalities are currently used for management of the lower incisor.
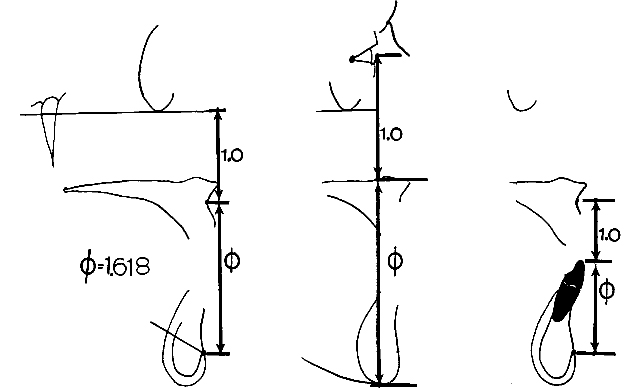
Proper height of the lower incisor can be established as a starting reference. Patient after patient and sample after sample of normal occlusions are almost uniformly observed to have the incisal edge of the lower incisor in a divine proportion to Points A and Pm: 1.0 to 1.618 (Fig. 12). Since both Point A and Point Pm can be altered with treatment, the whole question of where to go with treatment involves a prediction. The anticipation of the location of Points A and Pm is made prior to the orientation of the lower incisor in a treatment plan by sophisticated orthodontists.
It is true the lower incisor may be difficult to manage properly with round wires. For best long-term stability, best control of the mandible, and best utilization of growth during treatment, my practice in deep-bite cases for 30 years has been to treat to the level of the lower first premolar rather than extruding. This provides the least disturbance to the facial pattern, and ensures the least likelihood of post-treatment adjustment by preventing any increase in lower face height, which increases lip tension.
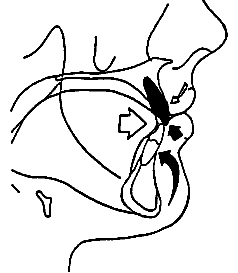
In fact, it is obvious that the lower incisor, when intruded into a wider portion of the mandibular symphysis, can be brought forward satisfactorily and safely. Such a practice will avoid the flat mouth and the flat face. Quite frequently, this is the method of choice when all the alternatives are considered.15 Another factor not often understood is that intrusion of the lower molar (or inhibition of eruption) is a significant factor in holding the lower incisor upright as it is finished with the ideal arch (Fig. 13).
In Class II, division 2 cases, both the upper and lower incisors are at fault. In these deep bites, intrusion of both the upper and lower anterior segments is required to prevent excessive mandibular rotation.
The level of the upper incisor is an esthetic consideration related to lip length. Many practitioners have been fooled into thinking that short lips, particularly in young male patients, would remain short for the life of the patient. Again, the divine proportion is a standard in the relationship of the upper incisor to the lower. It should be borne in mind that the whole palate can be tipped, taking the lip and nose with it. The smile line, or the margin of the upper lip in the passive smile, should be approximately at the level of the gingival crest of the upper incisor segment. Complementary nasolabial angles should also be a goal. All these factors must be taken into account in establishing techniques for the management of the lower incisor.
In short, it is time to put into mothballs another age-worn cliche--that the lower incisors should never be intruded.
5. "There are good reasons for extracting second bicuspids rather than first bicuspids."
Form and strength of the first premolar is a factor, but there are other reasons for upper second premolar extraction, such as sustaining space closure distal to the canine and management of the upper canines, which fit in the bifurcation of the roots of the upper first premolars. In 1993, many orthodontists consider a patient who once would have been a four-second-premolar extraction candidate now to be a nonextraction candidate. Slippage of anchorage is often required for second premolar extraction. Additionally, a choice can be made between premolar extraction and early removal of the third molars.
Extraction of the lower second premolar makes it necessary to contact the lower first premolar with the lower first molar, and the contact at the distal of the first premolar is rather narrow. The form of the first premolar is such that it frequently does not make good lingual contact with the upper premolar. Therefore, the best choice is to extract upper second and lower first premolars and modify the mesiobuccal angle of the second toward the anatomy of the first premolar.
6. "Differential anchorage is nature's way of harmonizing the temporomandibular joint and the teeth."
First, what is meant by "differential anchorage"? The statement was made that in natural growth, the lower molars seldom move forward appreciably in relation to the symphysis. Such an interpretation of growth and eruption of the lower molar, as mentioned above, is entirely dependent upon the method of superpositioning. If the lower border of the mandible is used for reference, the impression is gained that the lower arch does sometimes move distally (Fig. 1). As observed with implants, however, in normal development the lower border of the mandible is resorbed as the angle drifts on an arc upward and backward (Fig. 4). This shows that when the lower border of the mandible is employed as a reference, an erroneous impression might be gained with regard to mandibular development as well as to the eruption of the teeth. Two other references are much better for the display of lower arch development: the corpus axis and the arc method.
The beauty of the corpus axis is that it is based on Xi point and Pm and thus shows a remarkable tendency to stay level with the occlusal plane, which tends to move with Xi point. It is the best method I have found for accurately predicting occlusal plane behavior. Studies have shown that the lower molar tends to move at a right angle to the original corpus axis, upward and forward at about .5mm per year (Fig. 2).
In truth, however, as shown with the discovery of the mandibular arc, the entire lower arch continues to move upward and forward as space is made posteriorly for the second and third molars by the forward drift and eruption of the lower arch. The lower molars offer more limited resistance to forward movement unless the roots are torqued buccally and the arch is slightly expanded in an attempt to lock them underneath the buccal cortical plate. The upper molars move forward more easily, particularly because the main resistance is toward the palatal root.
I agree that the upper and lower incisors should remain out of occlusion almost throughout the course of treatment. I would pay attention to both incisors, however, depending on the individual diagnosis and prognosis.
7. "The most important part of orthodontic treatment is the management of the six upper anterior teeth."
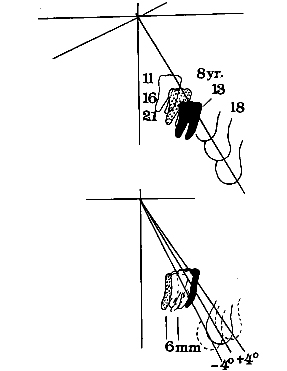
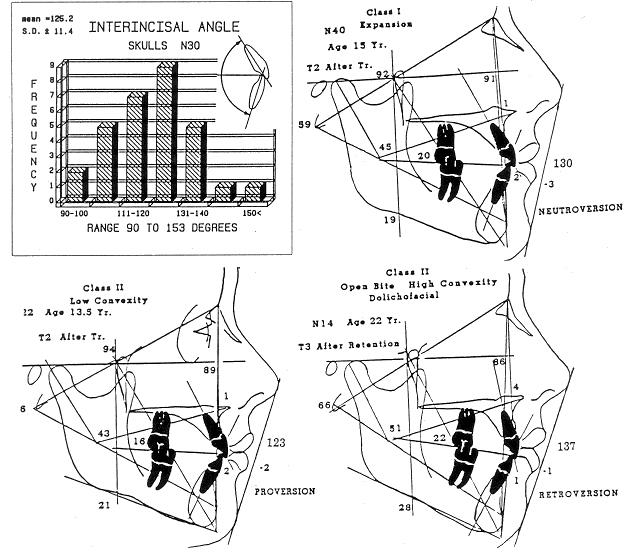
The author mentions that proper angulation and torquing are difficult to achieve without numerous archwire changes. I have prescribed three different bracket formulas, called a "trimorphic formulation", that account for the original malocclusion, the facial type, and the growth pattern (Fig. 14).
Patients with interincisal angles of 120°-125°, with a tendency for uprighting, are treated as the "proversion" type. Those with interincisal angles of around 130° use the "neutroversion" formula. The "retroversion" formula is for long faces and Class III conditions, with interincisal angles in the range of 135°.
With these formulations, frequently only two or three archwires are needed. In a Class II, division 2 case with retruded upper incisors, an upside-down loop is placed mesial to the canine so that in retraction, the action will be dispersed among the roots rather than expressed in lingual tipping of the crowns.
One aspect not often recognized is the function of the axial inclination of the upper incisor to support the lower lip (Fig. 15). Perhaps still greater sophistication is needed for full appraisal and management of the upper anterior segment.
Dr. Schudy replies:
Those who know me know that I would never knowingly misrepresent any information. They also know that I have always shown objective evidence to support any principle that I recommend. We all have great concern for students and young orthodontists who have not yet formulated their philosophy of clinical practice. When two persons of many years' experience come up with diametrically opposite views about important issue, it can produce great confusion in the minds of these young people.
A book written by Dr. George Schudy and myself 16 contains much objective evidence to support all the concepts, principles, and precepts that we recommend. The reason we have been so specific is that someone with a lifetime of concentrated study needs to nail down some important treatment principles. In this short space, I will present only a few highlights of the evidence I have accumulated. Of course, one can find exceptions to any rule.
In discussing the intrusion of molars, the respondent goes to great pains to explain what theoretically should happen, but never shows what actually does happen. He speaks of the jaws growing apart. The posterior portion of the jaws does grow apart, but the anterior portion merely adapts to the interfacing contact of the posterior teeth (Fig. 16).
In discussing opening of the bite by placing overlays on the posterior teeth, the respondent states, "Careful study of such patients indicated that the posterior teeth were intruded". This is the type of intrusion of molars that we insist does not happen. Many orthodontists have said they have seen intrusion of molars and have promised to send me films, but to date I have never received any. I have only received films showing extreme intrusion of molars due to pathologic, continued spasm of the closing muscles.
It is also stated that "when this kind of intrusion is observed in many patients, even the most extreme skeptic must take notice". Figure 6 looks like bona fide molar intrusion-- the kind we say does not happen. But first the illustration has to be better explained. Facial height, facial depth, anterior dental height, and posterior dental height are almost identical before and after treatment. Most of the skeletal measurements are exactly the same. The only difference is the teeth. The increase in the vertical dimension due to the posterior overlay is not shown; the recovery from the overlay was extremely rapid and complete, with hardly a millimeter of change in any dimension of the skeleton. All this is puzzling to me. If I am wrong I want to know, and I want the reader to know. But if I am right we will have truly established a truth in orthodontics (Fig. 17 and Fig. 18).
I thank the respondent for showing the instances of intrusion in Figure 7. The lower molars obviously did intrude, but this is not what I would call natural, normal function. He also mentioned the high-pull facebow and the protractive or reverse headgear. Both of these devices were first used in our office--the high-pull facebow in 1963 and the reverse headgear in 1965.
The respondent was certainly justified in objecting to my statements that the posterior nasal spine is not affected by treatment and that we are not sure that we can affect condylar growth. These intities are small, indefinite, and undependable, and they have only minor effects on clinical practice. I have been aware for many years of the possibility of orthopedic effects on the maxilla and have done my share of such procedures. I am aware that backward-rotating condyles can be changed to forward-rotating condyles with the right treatment procedures. So I thank the respondent for calling attention to these issues.
Figure 9 shows considerable leeway between the mesiodistal dimension of the deciduous molars and that of the premolars. The first molars simply occupied this extra space. Also, the forecast was done at age 14.8-- after growth has ceased in many girls. I would like to have seen the original film on which the forecast was done.
"The prohibition of lower incisor intrusion . . . lacks sophistication in light of present knowledge." Again, we need more than an opinion. We need evidence. The respondent states that "in most deep bites, the lower incisor is in supraversion" . Not so ! The molars and bicuspids are in infraversion.
Another statement is that "increased elevation of the premolar tends to rotate the mandible backward, which worsens the Class II condition". The respondent doesn't understand that the mandible does not rotate backward if vertical condylar growth equals or exceeds the combined vertical growth increments (Fig. 18 and Fig. 19). The cause of the backward rotation shown in Figure 11 was no growth of the condyles.
"The lower incisor can be successfully intruded.... Cases with lower incisor intrusion were demonstrated to be stable 30 years ago. The utility arch was developed in 1960". We used a utility arch in 1948, but not to intrude lower incisors. We used it to upright mandibular molars with the aid of extraoral anchorage and Class III elastics at night.
Regarding "successful intrusion", I refer to a study of 30 treated deep-bite cases from the respondent's office and 30 treated deep-bite cases from my office. The study was conducted in the mid-1970s, but was not formally reported until 1989.17 The criteria called for an average of 3mm of lower incisor intrusion in the respondent's sample, but there was actually an average intrusion of only 1.2mm. Our sample was to have no intrusion, and in fact the average was .3mm. Thus, the study was tilted in his favor.
Results of the study: "Both techniques were successful in overbite correction, producing only minimal increases in mandibular plane angle and anterior facial height. Mandibular incisors in the Ricketts group demonstrated more flaring and anterior bodily movement during treatment, with a greater amount of post-treatment uprighting and overbite relapse than the Schudy group."
In another study of 30 treated deep-bite cases, the author found a high correlation between intrusion of lower incisors and relapse of overbite.18 He also found a high correlation between occlusal movement of molars and stability of overbite. These findings are extremely important and relevant to our treatment of malocclusion. They mean, of course, that when we avoid intrusion of incisors, overbite is stable; when we intrude them, overbite is unstable. When we move molars occlusally, overbite is even more stable.
The respondent asks, "Why would our institutions research or teach growth if it were not to be applied or had no value?" I am not against the study of growth. I have done a considerable amount of it. However, no growth studies by individuals or institutions, as far as I know, have discussed specific increments and measured them in millimeters. If we do not measure the actual increments, then we are only studying the effects of growth increments. We are putting the cart before the horse.
It is the relationship of vertical and horizontal increments that controls the behavior of the chin. Given the vertical and horizontal increments, including the horizontal component of condylar growth, we can plot how much the chin will move forward and how much it will move downward. With this knowledge, we can begin to learn cause and effect (Fig. 20).
We have been discussing the mechanism of jaw growth for the past 33 years. Creekmore published an article in 1967 in which he discussed growth increments.19 Isaacson has comprehensively covered growth increments, how they are interrelated, and how they contribute to anatomical change.20 He has not reported measuring the actual increments.
The reason many orthodontists have rejected the prediction of growth is that it has been based on averages. Many orthodontists have, after the fact, sent films of unusual cases to the laboratory for growth predictions. When the reports came back, they were so grossly incorrect as to be almost ludicrous. If growth prediction has now been improved to the point that abnormal growth can be predicted, I welcome the improvement. But the profession needs more solid proof than it now has before endorsing such a notion.