Clinical Experience with Direct-Bonded Labial Retainers
Direct-bonded retainers are usually placed lingually,1-5 since one of the chief advantages of such retainers is their invisibility. However, we began to experiment with labial bonded retainers several years ago to improve long-term results because of certain retention problems:
1. Short- or long-term inability to prevent some reopening of premolar extraction sites in adults.
2. A tendency for some lingual crown relapse of canines that had been palatally impacted.
3. Difficulty in holding premolars that had been severely rotated.
4. Various types of space reopening in cases where posterior teeth had been moved mesially, in young or adult patients with previously excessive spacing.
Common to these situations was the desirability of adding some support to the premolar areas for one or two years after treatment. It appeared preferable to bond the retainer wires labially, based on earlier experience with bond failures at the enamel-adhesive interface when bonding to the lingual surfaces of premolars.3,4
Another alternative would be to bond the retainer in the occlusal fissure, which is usually successful if there is no contact with antagonists. In most cases, however, a groove has to be prepared with a bur to avoid such contact.5 This amount of enamel removal would not be acceptable in routine situations.
Study Design
The present study was designed to:
1. Evaluate the bonding success rates of different types of bonded labial retainers.
2. Study the effects on the gingival tissues and enamel adjacent to such retainers.
3. Determine whether the labial retainers are effective, particularly in preventing the reopening of premolar extraction sites in adults.
4. Tabulate patient reactions to different types of labial and lingual retainers, compared with removable plates.
Materials and Methods
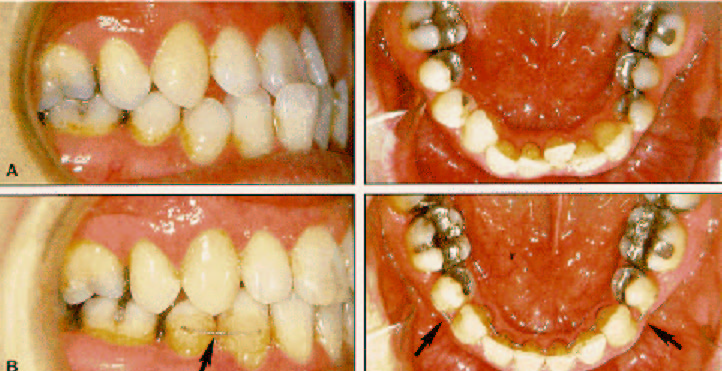
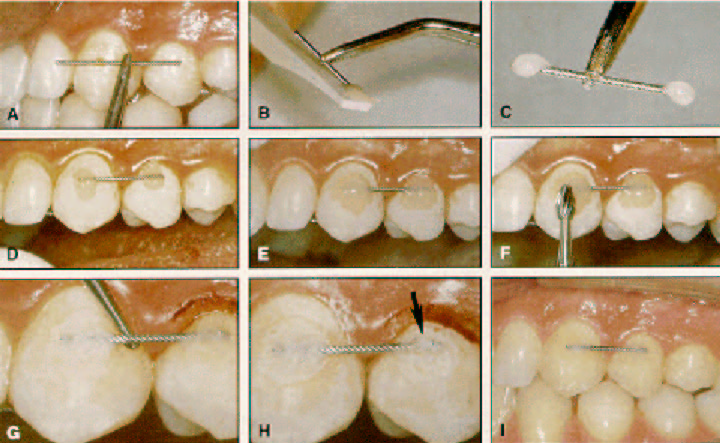
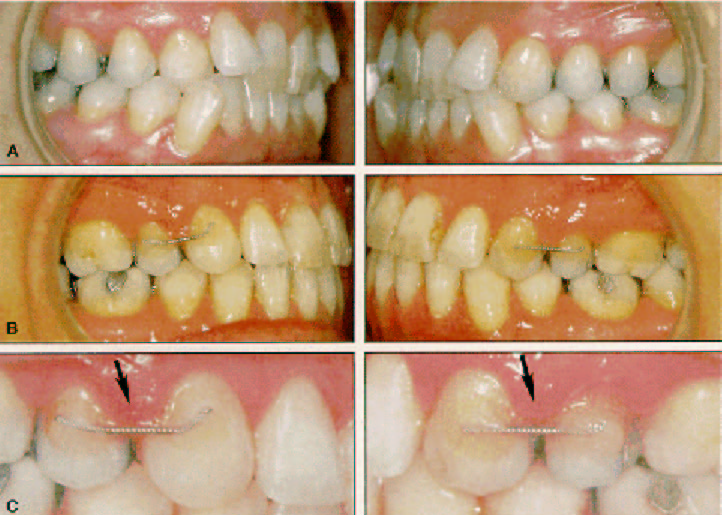
One group of 25 patients had received a total of 47 short (two-unit) labial retainers (Table 1). Most often the retainer was placed over a closed extraction site after removal of the upper or lower first or second premolar (Fig. 1), but retainers were also used in cases of palatally impacted maxillary canines (Fig. 2). The average observation period at the time of the follow-up examination was 2.3 years, and at that time the mean patient age was 34.5 years, with a range from 18 to 53 years.
In addition to the short labial retainer on one or both sides, these patients also received removable maxillary plates and/or standard lingual retainers bonded to the maxillary or mandibular incisors (Figs. 1,2,7).
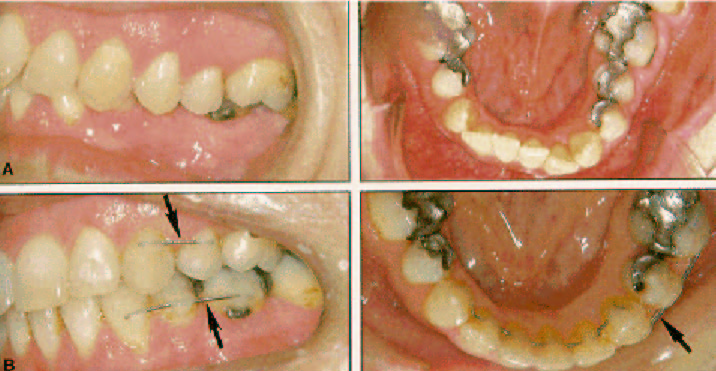
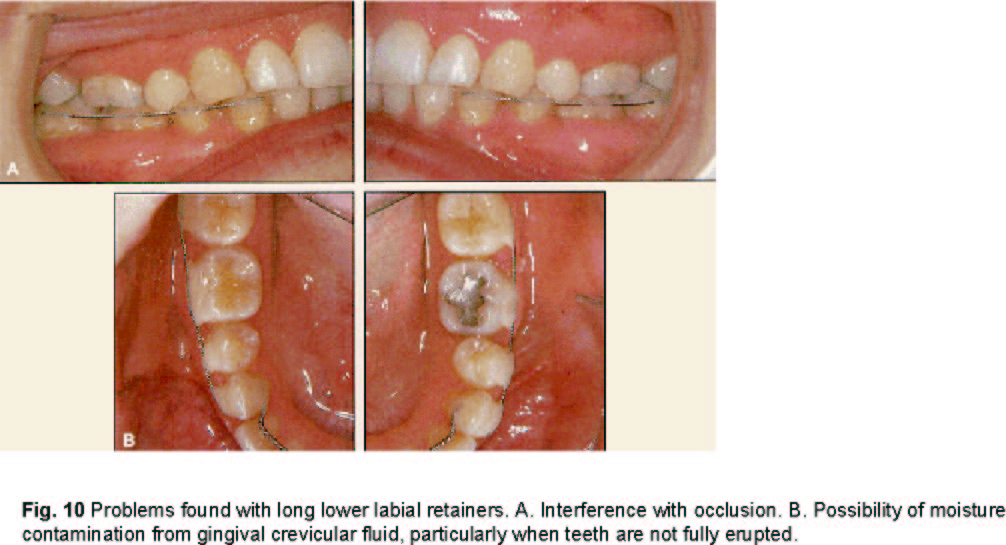
Another group of 10 patients had received a total of 14 long (three- or four-unit) labial retainers (Fig. 3). These retainers were used particularly in minimum anchorage situations involving mesial movement of entire posterior segments, where the lower second premolars were congenitally missing (Fig. 10). They were also placed in first-molar extraction cases (Fig. 4). The average observation time was 2.5 years, with a mean patient age of 35.7 years at follow-up.
The patients had all undergone full, routine orthodontic treatment for a variety of malocclusions. Together they represented all the bonded labial retainers placed in Dr. Zachrisson's office before May 1989. Five of the patients moved and could not be located for the follow-up examination.
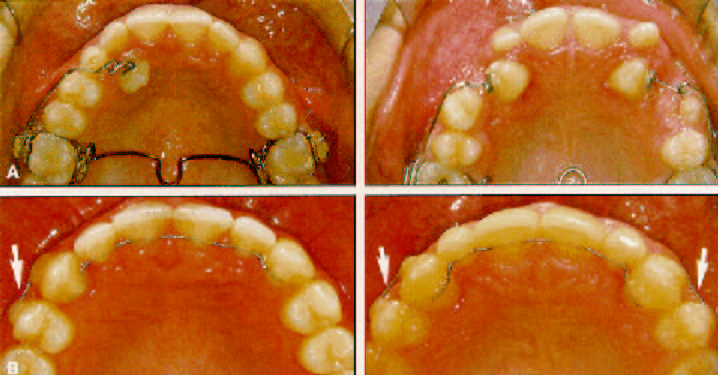
Each retainer was made of .0215" five-stranded spiral wire (Penta-One, Fig. 5A). After the labial surface was etched with 37% phosphoric acid for 30-60 seconds, the retainer was tacked in place on each end with a small amount of fast-setting composite6 (Concise). Slippage was avoided by dipping both ends of the wire into the composite mixture on the plastic spatula (Fig. 5B,C) and then placing the wire in position (Fig. 5D).
No sealant was added after etching. After setting, the bulk of the composite was added with a plastic instrument, thus ensuring totally undisturbed setting of the bulk of the composite. Contour trimming of the composite was done with tungsten carbide burs No. 7006 and 7408 (Fig. 5F), and interdental trimming with small round burs No. 1 and 2 (Fig. 5G). Care was taken to avoid contact between the composite and the gingival margin at the bonding sites (Fig. 5H), and between the interdental papillae and the retainer wire.
Every patient was instructed in maintenance of oral hygiene with toothbrushes and floss threaders. Daily rinsing with a .05% neutral sodium fluoride solution was prescribed throughout retention.
At the follow-up appointment, impressions for study models were made, intraoral photographs were taken, and the retainers were checked. The number of teeth included in each retainer and any occurrences of loosening or wire fracture were recorded from the patient's records. By comparing the follow-up study models with the post-treatment models, notations could be made of any tooth movements within the retained segments and of spaces that had opened adjacent to the retained segments.
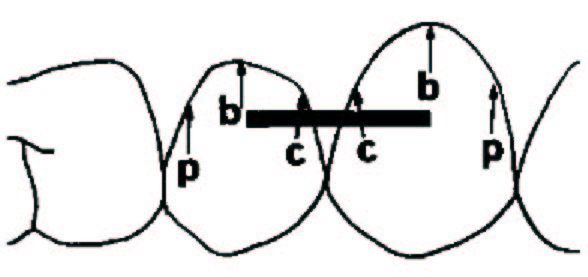
To reduce examiner bias, all scoring was done by an orthodontist (Dr. Axelsson) who had not seen any of the patients. Standard techniques were used to score plaque accumulation,7 gingival inflammation7 and recession,8 and demineralization.9,10 Pocket depths were probed along the retainer wire and gingival margin, as well as on all interdental surfaces of the teeth included in the retainer. For each rating, the average of two separate scores was used at each of three sites--peripheral, mid-buccal, and central--for each labial retainer (Fig. 6). Disclosing solution was not used.
Each patient anonymously answered a 16-point questionnaire at the follow-up examination. The first seven questions dealt directly with the labial retainers, including any embarrassment suffered when talking and smiling. Emphasis was placed on comparing the labial retainers to the lingual retainers and removable plates. The other nine questions were related to the overall orthodontic treatment experience, including the relationship between expectations and results, the value of the results compared to the time and money spent and the cooperation and oral hygiene required, the degree of esthetic concern about visible appliances, and the most positive and negative aspects of treatment. A copy of the complete questionnaire is available from the authors upon request.
Results
Only two of the 47 short labial retainers came loose during the observation period (Table 2). The failure rate for the long retainers was significantly higher, with all the loosenings occurring in the mandibular arch.
In most cases, the treatment result was well maintained. Of the 28 short upper labial retainers, two had spaces reopen distal to the retainer (Fig. 7) and two within the retained segment. Of the 19 short lower labial retainers, two had spaces reopen distal to the retainer, four within the retained segment, and one mesial to the retainer. The space was generally about .5mm, and was greater than 1mm in only one case.
No caries or white spot lesions were noted with the short retainers; two patients with long retainers showed surface demineralization. The plaque index scores were all either 0 or 1 on a scale from 0 to 3 (Table 3). Gingival index scores were all 0 or 1 at the mid-buccal locations, but occasionally 2 (bleeding upon probing) at the interdental sites (Table 4, Figs. 8,9).
The pocket depths were all measured at 1-2mm buccally, but in about half the cases they exceeded 2mm interdentally (Table 5, Fig. 9). The plaque and gingival scores and pocket depths were significantly greater (p less than .01) for the central sites than for the peripheral sites.
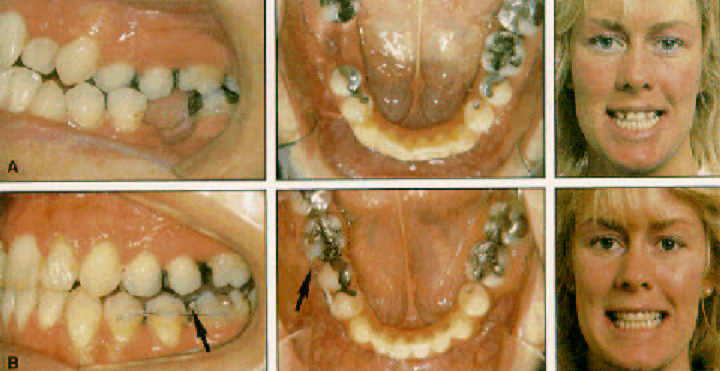
Patient satisfaction with the labial retainers was surprisingly high. Only 31% of the patients said they were "not much affected" or "somewhat affected" by the visibility of the retainers when talking or smiling, and 69% said they were "not affected at all". When patients with both labial and lingual retainers were asked which one they would prefer to keep for another year, only 59% preferred the lingual retainer. Given a choice between the labial retainer and the removable plate worn at night, 49% of the patients said they preferred to wear the labial retainer, 28% preferred the plate, and 23% were undecided.
Of the 35 patients who responded, only one was "somewhat dissatisfied" with the overall treatment result as compared to expectations on a five-point scale. Five were "very satisfied", and 29 were "completely satisfied". Nearly all the patients also felt the treatment was worth their time, money, cooperation, hygiene efforts, and esthetic appearance (Table 6).
Discussion
The results of this study show that labially bonded .0215" wires can be a useful supplement to conventional retention in certain situations, including adult premolar extraction cases (Figs. 1,3,7,9,11) and cases involving orthodontic correction of impacted canines (Figs. 2,5,8). More than 95% of the short labial retainers remained intact over the two-year observation period, and patient acceptance was much better than we expected.
The longer retainers, on the other hand, were considerably less successful. A combination of factors such as the patient's age, occlusal interference, and moisture contamination may have been responsible. As shown in Figure 10, it was often difficult to place the long mandibular retainers out of occlusion, particularly in young patients with short clinical crowns. When bonding close to the gingival margin, there is an increased risk of seepage of gingival crevicular fluid, which would be detrimental to bond strength.
Several studies have presented methods of preventing relapse in extraction cases.11-14 It is generally agreed that stabilization of orthodontic results is more difficult to achieve in adults than in children, and that special precautions and prolonged retention may be indicated in adults.15,16 This is at least partially due to changes in the metabolic status of bone, collagen, cells (fibroblasts), and blood flow or vascularity that occur with increasing age.15
The retainer wire used in our investigation was .0215" Penta-One five-stranded wire, which was shown in an earlier study of direct-bonded lingual retainers to have optimal properties for stabilizing segments of teeth splinted together, while allowing physiological mobility of the individual units.5 The most notable side effect was the opening of small spaces distal to the retainer wires in a few patients. In these cases, it is likely that tooth-size discrepancies played a role during settling of the occlusions (Fig. 7).
The question of when to remove the bonded retainers is easier to answer for the labial version than for the lingual.5 The labial retainers were intended only to gain an extension of the stabilization and remodeling process during the first year after orthodontic treatment. Therefore, they may be removed on an individual basis, depending on the retention problem and the patient's age, motivation, and hygiene. In our sample, retention with conventional removable plates continued when the labial wires were removed one to two years after treatment.
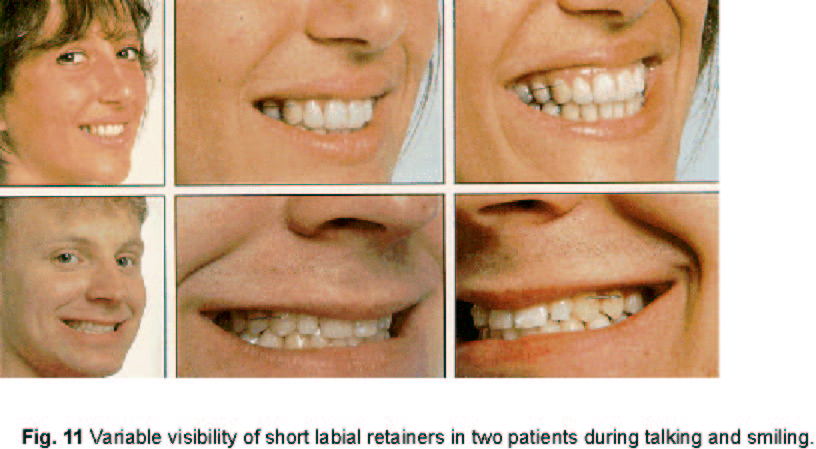
The visibility of the retainer wire varied among the patients because of variations in personality and smiles (Fig. 11). Still, for nearly all of them the short retainer caused little esthetic concern. Tooth-colored wires could be used in short labial retainers, but at present we do not believe they are necessary. Even more visible labial wires are routinely used in removable retainers that are worn day and night during the initial period after fixed-appliance removal.
It should be emphasized that although our sample was small, it represented a consecutive series of adult patients who had undergone full orthodontic treatment and a specific form of retention.
Few unbiased studies of such samples have been published. That nearly all of them were satisfied with the results and their efforts is in accordance with the experience of other clinicians,18-20 who have found that adult patients are relatively easy to satisfy. It is somewhat surprising, however, that more than 90% of the patients believed the time needed for correction was worthwhile, since most of them seemed to become more eager to have appliances removed as they approached the end of active treatment.
Conclusion
Bonding success rates and patient acceptance appear to be excellent for labial retainers bonded to two adjacent teeth. Such retainers may therefore be recommended for improved stabilization of extraction sites in adults, and for added retention of palatally impacted canines.
On the other hand, the results obtained with three- or four-unit bonded labial retainers were unsatisfactory, particularly in the mandibular arches of young patients. Further technical improvements will be required before these retainers can be routinely used on long buccal spans.
ACKNOWLEDGMENT: The authors gratefully acknowledge the word processing by Ms. Marit Sulander of the Norwegian Police Data Processing Service.