JCO INTERVIEWS
Dr. Rudolf Slavicek on Clinical and Instrumental Functional Analysis for Diagnosis and Treatment Planning, Part 1
DR. GOTTLIEB Rudi, what do you consider to be a complete orthodontic examination?
DR. SLAVICEK We routinely do a thorough clinical examination--including an interview,muscle palpation, and a neurological examination--and an instrumental analysis with mounted casts.
DR. GOTTLIEB How much of your time does the whole examination take?
DR. SLAVICEK For the first appointment, my patients (child or adult) are scheduled for 20 minutes with me for an interview. If you look and listen carefully, you can learn a lot there. Instrumental functional analysis takes a maximum of an additional 30 minutes of my clinical time. That amounts to a total of 50 minutes, perhaps one hour for everything. The rest of the instrumental analysis can be delegated. An hour may be 30 to 45 minutes more than an orthodontist takes who does a less elaborate diagnostic examination, but how long does treatment and retreatment take if you have misdiagnosed a case? One hour is cheap by comparison. In addition, this more thorough examination is the best way to document that you started with a diseased patient. If the joint was clicking at the beginning and you wrote it down and called the patient's attention to it, nobody can say later on that you caused the problem if the patient still clicks. But if you have no documentation at the beginning and the patient is clicking after treatment, you may be accused of causing the symptom. In the medical profession, you have to document and record the patient's condition at the start of treatment and do it in a consistent manner. One hour in a two- or three-year treatment is a small investment for that kind of protection.
DR. GOTTLIEB Can the interview be delegated?
DR. SLAVICEK I do not like to delegate it. I want a feel for what is going on with the patient. But if you have a person who is good with children, he or she can do the job. The person who does it must have the time, and a feeling for young people.
DR. GOTTLIEB Is your clinical examination the same for children and adults?
DR. SLAVICEK There is no basic difference between the functional analysis of the adult and child patient.
DR. GOTTLIEB What are you are looking for with muscle palpation?
DR. SLAVICEK This is my examination of the functional matrix, and we will show this in detail in a future article in this series. I palpate the same structures on both sides at the same time, equally and symmetrically to see if they respond equally. Body posture is also important. For example, if a child has a pelvis problem, the orthodontist may be the first one to recognize it. You have the patient stand upright in front of you, and you look at the shoulders and the pelvis. Everything must be aligned. If there is something askew down below, it is related to something above it and you have an asymmetric development that must be improved.
DR. GOTTLIEB Do you refer such patients for correcting imbalances outside the head and neck area?
DR. SLAVICEK Those cases require interdisciplinary action. I work with my physiotherapist on all dysfunction cases. If he does his job, I have an easier task in my area. This includes child patients.
DR. GOTTLIEB Can imbalances be reflected in the muscle chain upward and downward?
DR. SLAVICEK Absolutely! If you have a patient with an asymmetry in the face and he has to develop some posture change, this posture change affects the whole vertebral chain. Sometimes you have a neck problem caused by an occlusal problem. You may have a problem in your vertebrae caused by imbalance above. Very often in a growing child it may be a posture problem causing asymmetry in the teeth.
DR. GOTTLIEB Are certain muscles more symptomatic in certain cases?
DR. SLAVICEK Although I routinely palpate all the muscles, I take special care in certain muscles in certain cases. In a low-angle Class II, division 2 case, I would examine the medial pterygoid muscle very carefully. In a high-angle case with some posterior rotation of the mandible, I would have a close look at the suprahyoid and infrahyoid muscles and at the position of the hyoid bone. I go through the routine muscle examination, but in some cases I give a high priority to some muscle groups.
DR. GOTTLIEB What do you interpret from the position of the hyoid bone?
DR. SLAVICEK That's very interesting. The hyoid bone and the atlas show a lot about the posture of the patient. The position of the hyoid bone may indicate tension in the anterior region and speech problems. You also have to be aware that suprahyoid and infrahyoid muscles influence the growth pattern. High tension from the hyoid bone rotates the mandible. All your treatment objectives are influenced by the position of the hyoid bone. If you only consider the bone structure of the mandible, you forget the main thing--you forget muscles. You have closing muscles influencing anterior rotation and opening muscles influencing posterior rotation. If you have an imbalance between closing and opening muscles, and your prognosis is based only on the skeletal pattern of the mandible, you are wrong. Therefore, the position of the hyoid bone is very important and will be more important in cephalometric analysis in the future.
DR. GOTTLIEB How do you define the functional matrix?
DR. SLAVICEK I define the functional matrix as everything related to the function of soft tissues of the face--mimical muscles, tongue, speech, etc. In evaluating mimical muscles, we have to look for activity or passivity. There are lazy faces and very reactive faces. If you have a child with a hyperactive orbicularis/mentalis musculature, you should interfere as early as possible to establish good function. One of the best examples is how Frankel interferes in muscle patterns to influence bone development. I feel that genetics are more related to functional matrix than to bone. People are similar to their parents because they inherited their parents' functional matrix, not their bones. Bone reacts to functional matrix and both determine the form of the face. If you are able to change the functional pattern, you are able to change the face even without doing anything with the teeth.
DR. GOTTLIEB Is it the presence of signs and symptoms that causes you to proceed with the instrumental analysis?
DR. SLAVICEK Without signs or symptoms, I would do a very limited instrumental analysis.
DR. GOTTLIEB Why do you mount all cases on an articulator?
DR. SLAVICEK Hand-held casts provide only one piece of information--how teeth fit together. An articulator mounting with instrumental analysis allows you to know how the temporomandibular joints are functioning in relation to the occlusion. For example, if you have a crossbite, the two arches do not fit together properly and, therefore, the mandible is forced to go to one side. If you do a diagnosis with hand-held casts, you do not know how the system is disoriented by occlusion. So, we use a simple articulator mounting with a facebow and a so-called centric record to mount the casts and see where the system is being misdirected by the teeth. We take two minutes for a facebow procedure and another three minutes for a centric record. We delegate the mounting of the casts on an articulator, and we use this mounting to compare the patient's centric occlusion and centric relation positions, which is very important for documentation and for diagnosing the case. With that approach, you do not just observe the static Angle classification, but you see that the interocclusal relationships are dramatically changed and the orthodontic treatment plan must change. To summarize why I mount cases, it is because the jaw can be deflected by the occlusion and nobody can know the true nature of the deflection. Therefore, the diagnosis and plan of how to develop the occlusion must be based on mounted casts.
DR. GOTTLIEB What determines the jaw position you are looking for?
DR. SLAVICEK In a free movement, the joint moves to a border position. It is not hand-forced, but you do control the position and ask the patient to go forward and backward.
DR. GOTTLIEB How do you define border position?
DR. SLAVICEK Border positions are unstrained positions limited by unstrained ligaments and osseous structures. You have an anterior border position, a posterior border position, and lateral border positions. If the patient moves to a position in which his ligaments and muscles are unstrained and stops there, that is his physiologic border position. We feel that border positions are the diagnostic end positions of the jaw.
DR. GOTTLIEB In your instrumentation, you use a SAM 2 articulator. What is its advantage over other articulators?
DR. SLAVICEK An articulator is a tool for measurement of casts in space. Other articulators can do this, but the SAM 2 has more tools for diagnosis than a normal articulator. It was developed for diagnosis--to evaluate the occlusal plane, the incisal angles, and by adjusting the front table to establish an ideal incisor and canine relationship. With its fully adjustable posterior part we can see how the case is functioning, and it has two important accessories--the Mandibular Position Indicator, or M.P.I., and the Axiograph. These are very necessary tools to analyze the occlusion in space, especially for orthodontists.
DR. GOTTLIEB What does the M.P.I. do?
DR. SLAVICEK In my opinion, the M.P.I. is one of the tools an orthodontist should have to evaluate malposition of the jaw, and to follow jaw position in his treatment sequence and final stage of treatment. There is a three-dimensional change in most cases when the jaw transfers from a physiologic border position to maximum intercuspation. We try to avoid the phrase "retruded border position" because it indicates that force is used in positioning the mandible in a nonphysiologic position. Any manipulation technique must be strictly avoided. With the M.P.I. you can tell if the jaw is moving forward or backward, downward or upward in transferring from border position to maximum intercuspation. With this instrumentation you can see where it goes. This is a very valuable space-oriented diagnosis.
DR. GOTTLIEB What does the axiograph tell you?
DR. SLAVICEK The axiograph was originally used only to program the articulator, but in the last 10 years we found that this is a very instructive, graphic system to show how the mandible moves. We use it today much as a physician uses an electrocardiogram. It makes it possible for us to identify a normal joint, and muscle and joint problems such as compression, distraction, anterior position, or deformation. We can determine the therapeutic position for splint therapy, and in my opinion this is one of the most instructive ways to show joint movement. We will be showing what it does in detail in a future article in this series.
DR. GOTTLIEB The axiograph is used to identify compression, distraction, and anterior position. Does the M.P.I. give you that information, too?
DR. SLAVICEK Yes. The M.P.I. is the easy way to look for them on the mounted casts. The axiograph is mounted on the patient. If you use an individualized paraocclusal clutch with the axiograph, you have no occlusal interference and you see how the total system works. You have no periodontal ligaments on the stone casts, no give. On the axiograph, when the patient closes you see the reality. In the M.P.I. you see a more static reaction, which is a little bit different in most cases. But the M.P.I. is a very easy way to do it. The axiograph with a functional occlusion clutch is a more difficult way to do it, but a very instructive way. It should be done especially when you are finalizing cases.
DR. GOTTLIEB Do you use the axiograph on children?
DR. SLAVICEK Yes.
DR. GOTTLIEB Can the axiograph give you information that might help you to do something preventive on children?
DR. SLAVICEK Yes, and that is very important. Let's say you have a crossbite in the primary dentition, which is the time the morphology of the joints is being formed. Then the joints must adapt to this crossbite. The axiograph will let you determine if you have asymmetrical joints. This is a very strong indication to start treatment immediately. The axiograph is an early indicator that asymmetries are present during the growing phase of development. Right at the beginning of the development of an asymmetric case you have a high potential to use early treatment to set everything on a path toward normal growth. Therefore, the axiograph in children is not only for a scientific follow-up of development, but it can identify discrepancies early.
DR. GOTTLIEB How does the developing occlusion produce transverse joint problems?
DR. SLAVICEK Differences in development of left and right sides caused by occlusal problems start early. We have recognized asymmetries related to sleep positions and breathing. We also have to detect growth reacting to different occlusal relationships. A patient with a unilateral crossbite in the primary dentition develops a unilateral chewing pattern. A unilateral chewing pattern uses a unlateral neuromuscular system. The patient adapts to this asymmetric system. If you wait until the system develops fully--beyond the 10th year of age--and now you create a symmetrical occlusion, you are inviting a relapse or a dysfunction case later on by introducing a symmetrical occlusion into an asymmetrical system.
DR. GOTTLIEB So you want to see children early?
DR. SLAVICEK Absolutely! In my opinion, a future role of the orthodontist should be to ask to see children every six months after 4 years of age. It has more than one advantage. The child is used to coming in, and you have the chance to see if there is a need for interceptive treatment. A child reacts very well at that age. This is another expansion of the orthodontist's role in the future--to be as preventive as possible. Don't wait until dysgnathia or dysfunction is established. Don't treat the disease if you can prevent it by treating the early signs of the disease. If you see asymmetric problems or if you see sagittal problems such as crossbites, jump in immediately. If there are no problems, let them go.
DR. GOTTLIEB What causes compression?
DR. SLAVICEK If the occlusion does not support the joint, the mandible and condyles move upward and create compression of the joint. When marking the hinge-axis positions for comparison, if the M.P.I. shows a black spot more cranially than the red spot of the reference border position, that indicates compression.
DR. GOTTLIEB Under what circumstances would the occlusion not support the joint?
DR. SLAVICEK If you have no posterior teeth, or if you have intruded teeth posteriorly or overanchored teeth posteriorly. If you use buccal root torque to anchor the first molar against the cortical plate and then let the premolars and anterior teeth settle, you have overanchored the molars so that they will no longer erupt. The premolars are loaded, but the first molars are not in contact. If you also do not have contact on the second molars, you have no posterior support. If you do an M.P.I. in those cases, you will see that the joint is not supported by occlusion posteriorly--only anteriorly. Also, 80% of children are bruxers. They are heavily loaded from a psychic standpoint. With no support posteriorly, you get flattening of the condyles in 20-25% of those cases. Of course, if you are aware of the problem, you de-anchor the molars in the last phase of treatment and let them erupt. If the problem remains and if you load the joint permanently, it results in flattening of the condyle.
DR. GOTTLIEB Does the same thing happen with functional appliances?
DR. SLAVICEK If you position the mandible forward with an activator and grind away your posterior support totally in a hyperactive case, the mandible is forced upward toward the eminentia. You can see flattening on the condyles superior-anteriorly in those cases, and some bony changes in the eminentia. It can also cause pain.
DR. GOTTLIEB What causes distraction?
DR. SLAVICEK If you have uncontrolled posterior prematurities, especially in cases where you have a very strong functional matrix anteriorly, you have posterior fulcruming, and this causes a problem of distraction with the condyles being pulled back and down. This causes ligamentous problems in some cases. You do not have a centered joint functioning in a physiologic reference position.
DR. GOTTLIEB When we do rapid palatal expansion, we might have a period of six months in which we are creating distraction?
DR. SLAVICEK Prematurities caused by jumping the bite are not so important, because the muscles are moving and pacifying these prematurities.
DR. GOTTLIEB How about the wearing of an appliance that has a thick posterior platform?
DR. SLAVICEK It is now thought if you have only posterior support you are causing therapeutic distraction and it may cause a change in the form of the condyle by elongation of the ramus vertically in the growing child--not in the adult. If you only use it as an exercise tool for somehours in the day, then it's fine.
DR. GOTTLIEB Sometimes it is done with the idea of intruding molars.
DR. SLAVICEK I think it is much easier to distract the joint than to intrude molars, and some of the successes may be an illusion.
DR. GOTTLIEB Do platforms encourage bruxing?
DR. SLAVICEK I think so. At first they are pacifying the masseter and are not encouraging bruxing. If they are kept in longer, the masseter will try to force them away.
DR. GOTTLIEB What causes anterior positioning?
DR. SLAVICEK Anterior positioning is normal in a juvenile individual. The joint in a growing child is never placed posteriorly. If it is placed posteriorly, it is pathologic. The normal position in the child's joint is half a millimeter to one millimeter anterior to his border position, and he tries to avoid going back. Anterior positioning in an adult patient may be a compensating mechanism for a skeletal discrepancy. Anterior positioning in a Class II, division 1 is an example of this compensation.
DR. GOTTLIEB What is Bennett movement?
DR. SLAVICEK Bennett movement is side movement in a unilateral motion of the jaw. If you chew to one side, the mandible rotates and moves transversely to that side to bring the teeth into function. The medial and lateral pterygoids contract and rotate the jaw to the working side. Then the mandible moves bodily to the working side in function. Bennett movement is a necessary physiologic action of the mandible to make chewing efficient, but this Bennett movement is completely different from the Bennett movement that occurs during bruxism. During bruxism, especially if you have a bad posture because of a pillow and you are supporting the mandible and bruxing to one side, this induced Bennett movement is a pathologic ligamentous loaded position.
DR. GOTTLIEB How can you have negative Bennett movement?
DR. SLAVICEK That's a very interesting finding. You ask the patient to make a movement to the left side and you are expecting Bennett movement to the left side; but if the patient has a pathologic pattern, the condyle goes to the right side at the start of the movement. This unexpected behavior of Bennett may be caused by muscle problems or by a medially displaced disc that is medially and anteriorly rotated. It's an early detection of disc problems before the joint starts to click.
DR. GOTTLIEB Is immediate side shift a Bennett movement?
DR. SLAVICEK In our opinion immediate side shift is a pathologic Bennett movement in bruxism. Immediate side shift shows that before you start any work-related development, the mandible shifts sideways. This immediate side shift can only happen with a pathologically displaced joint or in a pathologic flat joint with a remodeled bony structure.
DR. GOTTLIEB Is clicking related to side shift?
DR. SLAVICEK Clicking is associated with some type of side shift for the reorientation of the condyle in the disc, but reduction in the joint is three-dimensional. A lot of reduction in the joint causes some transverse movements, but it is not primarily a side shift.
DR. GOTTLIEB What causes the noise in clicking?
DR. SLAVICEK The noise is related to the force of the joint returning to the disc in a reduction of the joint--a return to its normal position. In a luxated joint, there may be a click going out of the joint. Most authors think this is more of a ligamentous click. The reduction click is the sound of the head of the joint landing in the disc in the fossa.
DR. GOTTLIEB Is clicking a reason to treat?
DR. SLAVICEK No. Clicking is a symptom. If there is no evidence of progression or of pain or of any dysfunction, there is no reason to treat a click.
DR. GOTTLIEB Do you get anything out of joint x-rays?
DR. SLAVICEK I do, but there is no need to take joint x-rays in all cases. I do not like to be too invasive to my patients, and we have other ways to evaluate what is going on. If I take a joint x-ray, I am seeking to determine if there is strong deviation from normal shape.
DR. GOTTLIEB Pathology, in other words.
DR. SLAVICEK Pathology in the joint. Is it a completed pathology or is it still progressing? There is a difference between an arthritic joint that is making some noise and no longer has pain and an arthritic joint that is showing pain and progression. So number one is joint pathology. Number two, tumors. If I am not really sure, I must do a sophisticated joint examination.
DR. GOTTLIEB Do you ever use arthrograms?
DR. SLAVICEK My rule is not to perform invasive techniques unless there is a good reason. I do arthrograms at most on only 1% of my patients. Arthrograms are only necessary in a very delicate differential diagnosis situation.
DR. GOTTLIEB Do you ever use an x-ray for joint position?
DR. SLAVICEK No. there is no way to determine a three-dimensional joint position from a two-dimensional x-ray.
DR. GOTTLIEB Are loose ligaments in the joint an inherited situation?
DR. SLAVICEK It may be, depending on what type of patient you are discussing. If you have a patient with loose ligaments in other joints--for example, cheerleaders who do splits--and the TMJ has the same looseness, this is not a very dangerous situation if those patients are not overforced in their movements. If you have loose ligaments only in the TMJ, this is a dangerous indication. There is some evidence that these ligaments are stretched in relation to some occlusal problem.
DR. GOTTLIEB Is there any healing in the joint?
DR. SLAVICEK Yes, I think we have healing. We know that ligaments are very slow to heal, but there is some repair if you bring everything to the right position. Also, if everything in the neuromuscular aspect of the system is repaired, a lot of posture problems of the mandible are taken over by muscles. The ligaments are unloaded during function and they are only stretched by very poor muscle or occlusal patterns. There is also some tendency after causative factors are corrected for the shape of the disc to change due to normal function. A deformed disc may reform with normal function.
DR. GOTTLIEB When the disc escapes is it generally due to thinning of the rim of the disc?
DR. SLAVICEK The disc is the functional fossa of the joint, and there are reasons for a disorientation of the system mainly caused by occlusal and muscle problems. I don't think that it's primarily flattening of part of the perimeter of the disc.
DR. GOTTLIEB So you can recapture a disc with a reasonable expectation that it will stay recaptured?
DR. SLAVICEK Yes, but try to avoid the word "recapture". This is semantics, but I think we should say that we have rotary luxation or reduction of the joint. Reduction means we are again in the functional fossa.
DR. GOTTLIEB If the slipping of the disc is caused by a thinning of the rim, the slipping will recur, will it not?
DR. SLAVICEK If you have no reason for it to recur it will not, but if you have a thinned anterior or posterior band you have a risk patient. However, if the only symptom is that the disc slips out a little bit, that is not a reason to be overly concerned. You have to take care that the joint is not pathologically loaded. A joint not acting in the disc assembly is in more trouble if you have pathologic loading. If you are not able to have a permanent reduction of the joint, the occlusion must be very good. I do not like to have a compression situation in a physiologic disc assembly, but the more you are luxated out of the disc assembly the more dangerous a compression situation is. The structure of the joint is not designed for that. Therefore, the occlusion must support the joint very carefully in these cases.
DR. GOTTLIEB Is it ever indicated to treat loose ligaments by compression?
DR. SLAVICEK In loose ligament cases, we try to be as cranially oriented to the disc as possible, in order to unload ligaments. Distraction would cause more harm in these cases. Loose ligaments should not be distracted more, because they have a tendency to loosen up more.
DR. GOTTLIEB What do you call internal derangement?
DR. SLAVICEK Internal derangement is limited to one very clear symptom--a condyle that is sometimes reduced and sometimes luxated. This in-and-out situation causes what we call reciprocal click. The classical way to describe it is if you are posteriorly positioned in your occlusion, you are luxated. When you go forward or open, you are reduced. Going backward and forward alternately luxates and reduces the condyle. This reciprocal click is a classic syndrome. In some cases, the internal derangement is permanent--this means that in a posterior position you are luxated due to ligamentous or bony problems. You are not able to reduce. This may be a loose or tightly locked joint. There is another derangement that is very often overlooked where you have a normal joint position, but right at the end of forward movement you are able to luxate. Take it a little bit back, and it reduces. Another situation that is often overlooked is where the disc may be dislocated anteriorly.
DR. GOTTLIEB Do you recognize the term "TMJ syndrome"?
DR. SLAVICEK I do not like to isolate the TMJ. It is never only a TMJ problem. Therefore, I try to avoid the term "TMJ syndrome".
DR. GOTTLIEB How about "MPD syndrome"?
DR. SLAVICEK The P is the important part of that term--pain. If you say there is a syndrome related to severe pain in the skull and you have a lot of related symptoms, MPD is a shortcut term. The source of the pain is the main concern. It may be from the TMJ, from the muscles, or from dysfunction of some system. I don't like this term either, but the main thing is that there is evidence of facial pain related to some dysfunction problem.
DR. GOTTLIEB Is there such a thing as a child growing out of a condition that is presenting signs or symptoms?
DR. SLAVICEK Yes, but a child who is seated in a physiologic manner in his joint has a much greater chance to adapt than a child who is not. For example, a patient who had one joint severely distracted and laterally displaced by the occlusion developed a completely different joint pathway on that side. One side was very steep and the other very flat, which caused a lot of problems. He developed an asymmetry. You have to realize the joint grows asymmetrically in a case like that in trying to achieve a seated position. Later on you have a totally asymmetric mandible caused by growth and adaptation. Now you arrange the occlusion in a symmetrical way and it may not work. Every orthodontist knows that some cases respond very well on one side--you correct half a Class II within four or five months--and the other side of the same patient does not respond. Why? You have a joint problem. One joint is seated and one joint is not seated. You are dealing with two different halves of the patient. Joints that are not centered do not act the same as joints that are centered during growth and treatment.
DR. GOTTLIEB How should the orthodontist proceed in a case like that?
DR. SLAVICEK He must treat it immediately to reorient the joint, and then make the diagnosis. For example, if you have a midline discrepancy let's say of 2mm, if the asymmetry is in the alveolar process you have to make the correction orthodontically. But if the problem is related to an incorrect joint position, treating it as if it were an alveolar problem would be a mistake. You are better off using a diagnostic splint for two weeks on such cases before doing other diagnostic procedures. This is how we start all of our asymmetric cases. I think orthodontists in the future will have to pay special attention to them, because these are the really difficult cases.
DR. GOTTLIEB There are a lot of asymmetric cases.
DR. SLAVICEK Absolutely! And an asymmetric diagnosis is the real art of the profession. If you start early enough on a skeletally asymmetric case, you have the opportunity to make a symmetrical case out of it. If you start late, or if the patient comes in late, then you have to be aware that your occlusal treatment must be asymmetric. The left and the right TMJ complexes of the patient are different. They are not the same case.
DR. GOTTLIEB Unless it is obvious by looking at the occlusion or the face, how do you determine that the patient is asymmetric?
DR. SLAVICEK A lot of the cases look asymmetric. In some it is more subtle and you have to look at airway space and the nasal openings to see if left and right are different, and you have to look to the midlines. The patient with a midline discrepancy is always suspect. Some asymmetries show up in the cephalometric x-ray if the ear plugs are not aligned, or if you see a lot of ramus height difference and oblique occlusal planes. Then in some cases you see asymmetries as a difference in left and right measurements on the frontal x-ray. It is necessary to be aware of asymmetry, especially asymmetry in joint movement. We do a complete instrumental functional diagnosis for all our asymmetric cases, especially those with severe asymmetries. We will be showing all this in detail later in this series.
DR. GOTTLIEB In addition to considerations we have been discussing, tooth anatomy dictates what relationships are needed for a good functioning occlusion. Is there a spot on the lingual surface of the upper central incisors for optimal occlusion or is it an area?
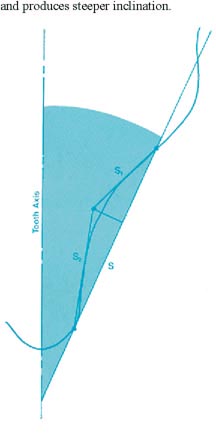
DR. SLAVICEK It's an area. The front teeth have a lingual concavity that has a flat area of about 2.5mm from the cingulum to the change point in the curve. We call that S1 (Fig. 1). We found in our research that the concavity is not circular--S1 is the flat part, S2 is the steep part. Nature is very tolerant so long as you position the lower incisors somewhere within S1. Nature will make the final adaptation. If you are too far forward and S2 is a steep incline, the alveolar process has to react. In most such cases, if the upper front teeth are well aligned, the lower anterior arch collapses and causes a problem; there is even more danger, because this is a very sensitive guidance area.
DR. GOTTLIEB What is the importance of anterior guidance?
DR. SLAVICEK The proprioception of the front teeth activates an avoidance mechanism in the neuromuscular system. The patient doesn't like to hit his front teeth. Therefore, he functions farther back. This may cause a problem for the joint. The more the muscles act in that position, the greater the strain. The front teeth, mandible, neuromuscular system, eminence--everything is designed to function forward. Everything that locks the system back is violating this design. If you create a neuromuscular avoidance mechanism, you strain suprahyoid muscle action and maybe you are causing a vertical problem. Sometimes you see an open bite develop, because everything is trying to avoid S2, growth takes place, and the patient rotates open. We believe today that the area you have to deal with is in the flat part of the lingual curvature or S1. I like to occlude in this area away from the change point, within a range of about a half a millimeter.
DR. GOTTLIEB What is the significance of losing anterior guidance in an anterior open bite?
DR. SLAVICEK The anterior teeth are like tentacles that feel where the mandible is moving. Number one, if they are out of contact, a lot of proprioceptive protective information is lost. Number two, in bruxism you have a very poor situation because all your guidance mechanisms are loaded posteriorly by the heavy muscles. You have inclined planes posteriorly that act as a guidance system during bruxism, but they are not designed to take that loading. Number three is esthetics, of course; and number four, the more you open the bite toward the posterior, the fewer tooth surfaces you have to chew with. I agree with Ricketts that there are not so many genetically caused open bites; there are a lot of open bite cases caused by TMJ resorptions in the early stages.
DR. GOTTLIEB How do you orient the lingual anatomy of upper incisor in your analysis?
DR. SLAVICEK The surface is oriented exactly to the coordinate system of the x-ray and related to hinge point and orbital point. You will see this when we demonstrate the computer system.
DR. GOTTLIEB Then do you relate the lower teeth to this surface?
DR. SLAVICEK Yes. We relate the long axis of lower incisor perpendicular to the line connecting hinge-axis and the tip of the lower incisors, and we relate it to the lingual surface of the upper incisor. Then we establish the occlusal plane and arrange the occlusion.
DR. GOTTLIEB Do you position the lower anterior teeth first?
DR. SLAVICEK Absolutely!
DR. GOTTLIEB In what position?
DR. SLAVICEK We collected a sample of untreated patients with no signs or symptoms. Wefound that the position of the incisal edge of the lower front teeth was closely related to the APg plane, independent of skeletal pattern. Nature arranges teeth with respect to skeletal pattern with inclination, not with position. We found it also is around 90° to the closing axis of the mandible with a little variation. Class II is a little bit more anteriorly inclined, Class III is reclined a little bit more posteriorly.
DR. GOTTLIEB Angulation adjusts for position?
DR. SLAVICEK Yes. Inclination corrects position. The closing axis is mechanically oriented. It determines the inclination of the teeth. The roots develop in the direction of the closing axis throughout the whole mandible including the molars, which is very important.
DR. GOTTLIEB Does leveling the curve of Spee violate the principle?
DR. SLAVICEK Elimination of the curve of Spee is completely against the biomechanics of the system.
DR. GOTTLIEB Of course, some of it returns when we let go.
DR. SLAVICEK I feel that what we call relapse is often what nature does to correct orthodontic treatment. The system is designed with an individual curve of Spee to coordinate with tooth morphology. Teeth do not fit together in a straight line. If you look at the anatomy of a set of natural teeth, it requires some curve of Spee. If you straighten the curve of Spee and put the molars in Class I, you always land in an edge-to-edge position. If the front teeth are in good alignment, you land half a cusp behind with the posterior teeth. If you eliminate the curve of Spee you will be lacking space of half a premolar on each side in the lower arch, or one premolar width for the whole lower arch. If you eliminate the curve of Spee in the upper arch, you are creating space. The mistaken thinking is that if you eliminate the curve in occlusion, you are straightening upper and lower equally. That is not true! You are narrowing the upper cuspid-cuspid width and you are widening the lower, because you are bending along the contact points. The roots are coming together, but the cusps are going out. In the upper, you have the reverse mechanism.
DR. GOTTLIEB Are you saying that orthodontists ought to be maintaining the curve of Spee during treatment?
DR. SLAVICEK They have to diagnose the curve of Spee. There are curves of Spee that are far too accentuated. They may have to alter them, but we have the means today to determine what the appropriate curve of Spee is for the individual patient.
DR. GOTTLIEB How do you do that?
DR. SLAVICEK We measure the perpendicular distance from hinge point to the plane of occlusion. By varying the distance to the plane of occlusion, you vary the curvature of the curve of Spee. The more the occlusal plane is inclined upward, the more the curve of Spee will be flattened. The more the occusal plane is inclined downward, the more accentuated the curve of Spee. In orthodontics today, we are often inclining occlusal plane downward and flattening the curve of Spee, which is the wrong way. If you are inclining upward, you have to flatten the curve some. The curve of Spee must be individualized. If you look at development, it makes sense. In a newborn baby, you have no distance from the hinge-axis to the plane of occlusion. The hinge lies on the plane of occlusion. There is no articular eminence and there is no curve of Spee at this stage of development. As the teeth come in there is a little more distance between hinge-axis and occlusal plane, and the articular eminence and the curve of Spee compensate for this distance. The closer you get to the final stage of development, the more eminence develops and the more curvature. You see an individual curve of Spee based on the distance from hinge point to occlusal plane perpendicularly. It is predictable, and we can also use the computer for this purpose.
DR. GOTTLIEB Is overbite an important consideration?
DR. SLAVICEK Vertical overbite is necessary as a guidance system for the total stomatognathic system, but we don't want the over bite to limit anterior movement. If you have anterior freedom, then it is a wonderful guidance system. Studies have shown that natural systems have different overbites and overjets, and that teeth are oriented to allow anterior movement of the mandible. These studies also showed that the incisal edges of the upper teeth are always more anterior than in most of the orthodontic philosophies.
DR. GOTTLIEB Does that happen because the interincisal angle is decreased as overbite increases?
DR. SLAVICEK More than one factor is involved. The difference in anterior tooth size is one, and the lingual anatomy of the teeth is different from individual to individual. The functional surface palatally is not highly correlated to long axis of the tooth. That means that interincisal angle is not a very valid measurement. Also, we feel that the upper front teeth react to the position of the lower front teeth in inclination more than in position, and their position is more anterior than we believe in orthodontics. In a mesiofacial case, we have had about 4.5mm overjet, but in Class II cases we are on the average 5-6mm anterior; and the overbite is between 3 and 3.5mm between upper and lower incisors, which is a lot.
ACKNOWLEDGMENT: Dr. Slavicek and JCO would like to thank Mr. William Missert of William Missert, Inc., Orthodontic Laboratory, Rochester, NY, for his help in producing this series.
(TO BE CONTINUED)