CASE REPORT
Treatment of a Patient with Juvenile Periodontitis
If a Class II division 1 malocclusion results from mandibular retrognathia, or mandibular dentoalveolar retrusion, treatment procedures which retract the maxillary components may be unfavorable. More appropriate treatment may include advancement of the mandibular components through tooth movement, mandibular repositioning, or orthognathic surgery. In a growing patient, mandibular repositioning appliances2 may be the method of choice.
Original Herbst Appliance
The Herbst appliance is designed to reposition the mandible anteriorly. It utilizes a pair of telescoping elements which allow the mouth to open, but limit posterior displacement of the mandible. Unlike many removable functional appliances which are used to reposition the mandible anteriorly, the Herbst appliance does not interfere with speech or eating. Also, since it cannot be removed by the patient, full-time cooperation is more predictable. When indicated, the Herbst appliance can be used in the treatment of Class II malocclusion2.
Although the Herbst technique has many advantages, clinical application of the Herbst design advocated by Pancherz3 and described by Langford4 has been problematic. First, since the lower part of the appliance is attached to mandibular first bicuspid bands, use of the Herbst appliance is limited to those patients with erupted mandibular first bicuspids. This requirement prevents many younger patients in the deciduous or mixed dentition stages from wearing the appliance. Secondly, repeated breakage and loosening of the appliance occurs, especially in the lower bicuspid band area. Langford5 has stated that the placement of stainless steel crowns on the abutment teeth has been helpful in preventing this. Another frequently encountered problem is rapid intrusion of the mandibular first bicuspids. Even though this condition is temporary and the bicuspids reerupt after treatment, their intrusion partially deactivates the appliance. As the bicuspids are driven down, the effective length of the plunger-sleeve combination (which advances the mandible) shortens, so that the mandible is held less far forward. Compensation for this deactivation requires lengthening the upper sleeves, either by placement of shims between the paired telescoping elements, or by replacement of the upper sleeves.
Also, as the bicuspids are depressed the lingual bar, which passes from the lingual of one bicuspid around the lingual of the incisors to the opposite bicuspid, is also depressed. This occasionally results in impingement on the lingual gingiva, causing ulceration and necessitating the interruption of treatment. Lastly, the possiblity of incisor tooth fracture exists once the appliance is attached. Often, as the telescoping elements are engaged and the mandible is brought forward, the posterior teeth disarticulate, leaving only the incisor teeth in occlusion. Without the protection of posterior tooth contact, rapid and forceful closure of the mouth may result in fracture of the incisor teeth.
Bonded Herbst Appliance
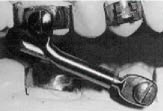
By altering the original Herbst configuration, these limitations may be overcome. Like the original design (Fig. 1), the proposed design includes paired telescoping elements. These elements are attached to the maxillary arch in the manner described by Langford4 (Fig. 2). The principal difference between the original and the proposed appliance designs is that the paired telescoping elements, which had been attached to the lower bicuspid bands, are now attached to the entire lower dental arch by an acrylic bite splint(Fig. 3).
Modifications
1. Short, stiff coil springs (.020" spring wire) 3mm long, with an inside diameter slightly larger than the plunger shaft, can be placed between the upper and lower telescoping elements (Fig. 4).They are designed to provide a dampening effect as the plungers sleeves contact upon closure. This may reduce shock-induced loosening of either the upper bands or the lower splint. These springs can also be used to reactivate the appliance. By placing the springs over the lower plunger shafts, the upper sleeves are displaced distally, effectively lengthening the telescoping mechanisms, and thereby advancing the mandible farther forward. This procedure may be especially helpful for patients with severe mandibular retrognathia, who might benefit from stepwise mandibular advancement.
2. A patient may require palatal expansion to coordinate the dental arches once the lower jaw has been brought forward. If so, a rapid palatal expander can be incorporated into the Herbst design.
3. If the maxillary arch width is adequate, but rotation and displacement of the maxillary posterior teeth are to be minimized, a transpalatal arch bar can be connected between the first permanent molar teeth.
4. A patient displaying vertical hyperplasia of the lower face may benefit from the simultaneous application of a vertical-pull chin cup in order to restrict further vertical development of the lower face. Since the entire maxillary dentition is in contact with the splint, a significant amount of force can be applied using the vertical-pull chin cup.
5. A patient with hyperactive mentalis muscle may benefit from the attachment of Frankel-like labial pads in order to inhibit mentalis muscle activity. By incorporating a buccal tube in each side of the mandibular splint, removable labial pads can be worn with the Herbst appliance.
6. Also, if a distal component of force is desired, a mandibular lip bumper can be inserted into similar buccal tubes in the lower splint6.
7. Further modifications of the splint design are under evaluation. These modifications include bonding procedures for both the upper and lower halves of the Herbst appliance, as well as adaptations which allow simultaneous application of the Herbst mechanism with full bands.
8. To facilitate removal of the bonded Herbst appliance, we drill holes in the splint corresponding to the middle of the occlusal surfaces of the lower posterior teeth to accommodate the resting leg of
a posterior band-removing plier.
Fabrication and Clinical Application
First Patient Visit
1. Bands are fitted to the maxillary first molars and first bicuspids.
2. An impression is taken of the lower arch and of the upper teeth, with the bands in place.
3. A protrusive wax bite is obtained, registering the desired anterior repositioning of the lower jaw.
4. The maxillary bands are removed and replaced in the impression. Laboratory Preparation
1. The impressions are poured and the models are mounted on a simple articulator, using the advanced wax bite.
2. The maxillary Herbst is constructed as described by Langford4.
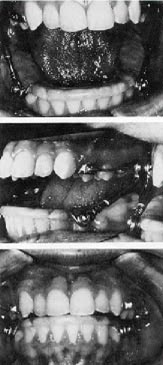
3. An acrylic bite splint is fabricated on the lower model. The splint is constructed, using a circumferential wire framework, which supports the lower Herbst axles. The entire framework is embedded in an acrylic splint, which extends from the last available molar tooth on one side, around the arch, to the last molar tooth on the opposite side. The acrylic coverage begins at the free gingival margin on the buccal of the posterior teeth and runs over the occlusal surface of the teeth, ending at the free gingival margin on the lingual. In the anterior region the splint is reduced from the cervical, so that only the occlusal one-third of the incisor and cuspid crowns is covered with acrylic (Fig. 5). The splint contains the lower pivots, which are positioned in the area of the mandibular first bicuspids or deciduous first molars.
4. The length of the sleeve and plunger are determined by the wax bite registration, and cut to fit. Second Patient Visit
1. The maxillary appliance is cemented.
2. The lower splint is bonded to all lower teeth including the incisors, using a conventional etching and bonding technique.
3. The paired telescoping elements are positioned onto their respective axles, the screws are replaced, and the appliance is now operational (Fig. 6).
4. Instructions are given to the patient and parents.
Patients are instructed to restrict sugar intake, brush carefully, and use a fluoride mouth-rinse. It is imperative that patients follow these instructions, in order to avoid decalcification of the teeth.
Some discomfort may be expected during the first few days. However, once this has passed, patients have been surprisingly comfortable. As Langford4 points out, the appliance may separate upon wide opening, but the patient quickly learns to replace the lower plunger into the upper sleeves. Special care must be taken not to extend the lower plunger out the top of the upper sleeve during appliance construction (Fig. 7). If the plunger is left too long, an acute ulceration and infection of the cheek can result.
Advantages of the Splint Design
The bonded mandibular splint was designed by the author to solve several problems. First, it allows attachment to the entire mandibular dental arch without the use of orthodontic bands on the mandibular first bicuspid teeth. Therefore, patients at any stage of dental development can be fitted with the bonded Herbst. This modification may make the Herbst suitable for large numbers of young orthodontic patients who might not be able to wear the appliance as originally designed. Secondly, tooth movement--especially the intrusion of the mandibular bicuspids--is minimized, since the lower arch is stabilized as a single unit. This may also reduce the likelihood of mesial migration of the lower anterior teeth. While this hypothesis has not been tested, early observation suggests it as a possible effect. Thirdly, tissue impingement of the lower lingual wire-which had been a problem in the original appliance-is prevented since it is replace by the acrylic splint-which covers the occlusal and incisal surfaces-offers a degree of protection from incisor fracture, since the posterior teeth contact the splint upon closure. Finally, the incidence of failure of the appliance due to breakage has been greatly reduced.