JCO Interviews Dr. James McNamara, Jr., on the Frankel Appliance, Part 1: Biological Basis and Appliance Design
DR. GOTTLIEB Jim, give us a little background on how you became involved with the Frankel Appliance.
DR. MCNAMARA After graduation from the University of California orthodontic program in 1968, I came to Michigan for a Ph.D. in anatomy. I sent a copy of my Ph.D. thesis on functional protrusion experiments in monkeys to a number of people whom I knew were interested in formand function. Tom Graber suggested that Professor Rolf Frankel might be interested in myexperimental work. Several months later, Professor Frankel wrote to me stating that he felt that I had shown experimentally what he had been doing clinically for about 15 years. Frankel was interested in the fact that the musculature was being monitored in my experiments, as well as the skeletal and dental aspects. In 1973, I went to the Third International Orthodontic Congress in England, and Frankel was on the program. He cited me twice in his presentation, and we began a professional and personal friendship which has endured to this day. I had a chance to thoroughly discuss Frankel therapy during his visit to the United States in 1974, and shortly thereafter I started using his approach in treating a few patients. In 1975, I was invited by the East German government to participate in a symposium on orthodontics and craniofacial growth, and I had an opportunity to get a first-hand look at his treatment methods.
DR. GOTTLIEB Did you have a chance to visit his clinic and see patients?
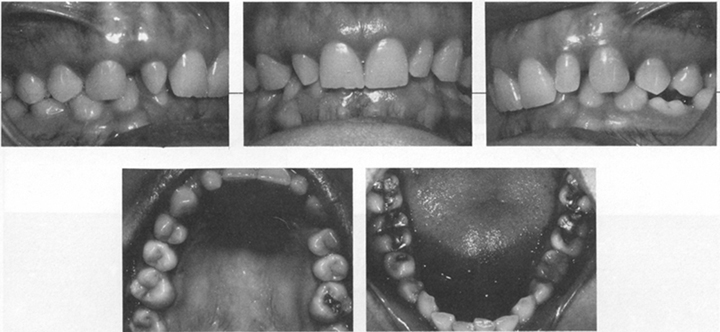
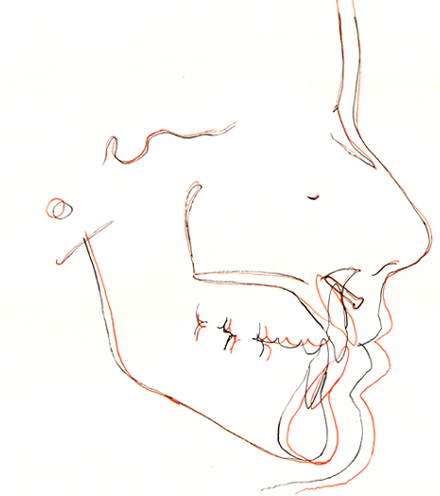
DR. MCNAMARA Yes, during the week before the symposium, I visited Frankel's clinic in Zwickau and saw about 75 patients treated with the functional regulator (Fig. 1). I was amazed at the change in the patients' skeletal and dental development, particularly anteroposteriorly. I saw all the things he had reported in his papers. I also gained an appreciation of how much arch expansion occurs routinely with his functional appliance.
DR. GOTTLIEB Had any of the cases been out of retention for a long period of time?
DR. MCNAMARA Some were five to eight years out of retention, and the stability was excellent.
DR. GOTTLIEB The lower incisors remained stable?
DR. MCNAMARA Yes.
DR. GOTTLIEB Were you looking at the patients or at the records?
DR. MCNAMARA Both.
DR. GOTTLIEB What kind of records were available?
DR. MCNAMARA I think that Frankel had treated some 3,000 patients (mostly Class II division 1 malocclusions) with his appliance, the functional regulator, and his records were as thorough as I have ever seen. He usually has serial radiographs taken on an annual basis and dental casts taken three or four times during and after treatment. The results were something I had never seen or expected to see, because my orthodontic training was in traditional edgewise mechanics and there was no emphasis on affecting facial growth (with the exception perhaps of the use of headgear).
DR. GOTTLIEB And that experience is what motivated you to become involved in Frankel therapy?
DR. MCNAMARA Yes. When I returned home, I was tremendously motivated to start more patients on the Frankel appliance in my practice. I also started a clinical study at the University of Detroit.
DR. GOTTLIEB How many years of experience have you had with the functional regulator?
DR. MCNAMARA I started my first Frankel cases eight years ago. However, those of us using the Frankel appliance in the early years made many errors in adapting his treatment approach to an American orthodontic practice. Many of our innovations turned out to be mistakes rather than improvements of the technique. I only really attained an understanding of the nuances of Frankel therapy a few years ago.
DR. GOTTLIEB Are you implying that you are getting results now that are different from those you were getting in the earlier years?
DR. MCNAMARA Yes. We are getting better results now. It would be unfortunate if the appliance were to be judged on the basis of our earlier knowledge. The design, construction, management, and manipulation of the appliance has improved dramatically.
DR. GOTTLIEB I would like you to tell us what those changes are, show what you now consider to-be the correct way to construct and use the appliance, and discuss the pitfalls and problems. But first, I'd like to begin at the beginning and ask you if there is adequate evidence that a change in function will result in a change in form.
DR. MCNAMARA The interaction between form and function is a basic biological axiom. In the craniofacial region, the relationship between form and function has been clearly shown in experiments using various animal species. For example, the work of Petrovic and colleagues (Petrovic, '70, '72; Petrovic et al, '73, '75, '81 ) and our studies (McNamara, '72, '73, '75, '80; McNamara and Carlson, '79) have shown that by experimentally altering mandibular posture, the amount and direction of condylar growth can be altered (Fig. 2).
DR. GOTTLIEB I believe that Petrovic, for example, worked on rats. Is it valid to say what happens in a rat can be expected to happen in a human being?
DR. MCNAMARA The experimental animals primarily used have been rats, rabbits, guinea pigs, and monkeys. The response of the mandible in each of these species has been the same. While the jaw movements of the monkey are more closely akin to the human, if a rat, a rabbit, a guinea pig, and a monkey respond in the same way, it's not illogical to assume that a similar response occurs in humans. In my estimation, you need a strong argument stating why it would not occur.
DR. GOTTLIEB Are the condyles you are dealing with in each of these species the same?
DR. MCNAMARA The basic tissues are the same. Each condyle is characterized by bone and secondary cartilage. The condyles, while varying in shape, are very similar as far as the response in the joint is concerned.
DR. GOTTLIEB How about the muscles?
DR. MCNAMARA The monkey, on which we conducted our muscle experiments, has a muscle orientation similar to man. Most other morphological features are also similar. Obviously it is not possible to do a longitudinal histological study of humans, so we are making a certain leap of faith that the experimental evidence does have some human applicability. But every indication that I have seen, clinically as well as experimentally, tells me that the general tissue responses are the same. There may be differences in the amount, rate, or direction of growth; but in my estimation, there is no question that you can alter growth. You can. The question is, "How much can you alter condylar growth?"
DR. GOTTLIEB The question that I hear everywhere is, "Can you make the mandible grow larger with treatment than it would have grown without treatment?"
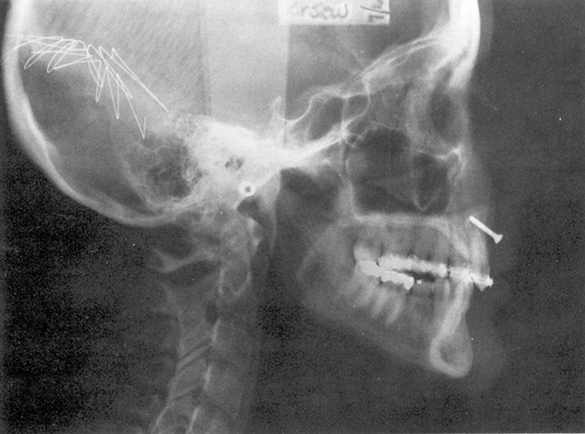
DR. MCNAMARA We have compared the cephalometric findings from 58 Class II patients treated with the Frankel appliance to those of a group of untreated Class II's from The University of Michigan Elementary and Secondary School Growth Study. When considering the effective length of the maxilla (Fig. 3), the Frankel appliance had a slight restrictive effect on maxillary development when compared to untreated Class II's. The effect of Frankel therapy on mandibular growth was greater than on maxillary growth. On the average, mandibular length (as measured from condylion to anatomical gnathion) increased by 3.5mm per year in the treated group, compared to 2.3mm per year in the untreated group (Fig. 4). This is an increase in the rate of mandibular growth of approximately 50% per year, which is similar to the values we have observed in our primate experiments.
DR. GOTTLIEB You're talking about a difference of a little over a millimeter. It's true that it's 50%, but it is still rather small.
DR. MCNAMARA First, these are average values. In many cases much greater increases in mandibular length occur. The most growth I've seen in a year and a half was about 10mm.However, that's unusual. In the untreated sample, 2½mm a year of mandibular growth occurred, while in some Frankel cases, 4 to 5mm a year occurred. The distribution of the individuals in the untreated and treated samples can be seen in Figure 4.
DR. GOTTLIEB Has anyone ever shown that the length of mandible can be increased to a greater extent than that which is "genetically predetermined"?
DR. MCNAMARA Not in human patients. The only investigators to approach this subject have been Petrovic, Stutzmann, and Gasson in Strasbourg (Petrovic et al, '81). In an experiment in which rats wore a functional protrusion device during their entire growth period (from 20 to 180 days), the overall length of the mandible was 12-15% greater in the experimental group than in the controls when growth had ceased. Generalizing those findings to include monkeys or humans cannot be done directly, although preliminary findings from our ongoing studies of long-term adaptations in rhesus monkeys seem to indicate similar results. If these observations hold true for man, perhaps the extent to which mandibular growth can be affected by functional appliance therapy is in the range of 5 to 15mm in the human patient.
DR. GOTTLIEB If mandibular growth can be in creased, how does the Frankel appliance accomplish this?
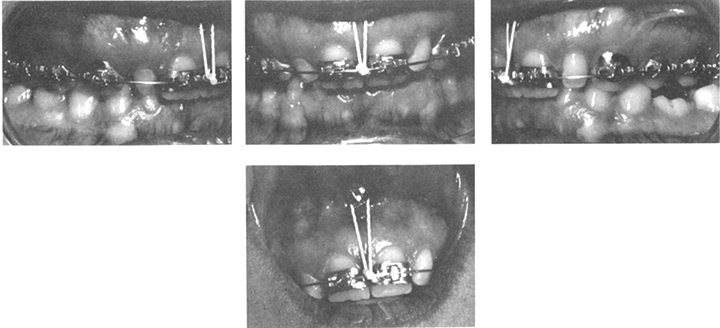
DR. MCNAMARA Here is a drawing (Fig. 5A) of a patient with a Class II division I malocclusion, a rolled lower lip, and a very prominent mental is muscle. Placing an FR-2 in the mouth causes a change in the level of postural activity of the facial and masticatory muscles (Fig. 5B). Anteroposterior correction of the Class II malocclusion is accomplished by repositioning the mandible anteriorly. For this purpose the lower part of the FR-2 appliance (Fig. 1) is equipped with a template consisting of the lower labial pads, which are small acrylic pads which lie in the mental sulcus below the incisors, and the lingual shield, a horseshoe of acrylic which lies lingually below the gingival margin of the lower teeth. Upon closure, the alveolus of the lower jaw engages in this template and stays forward. The appliance also provides a framework which interrupts abnormal function and establishes balanced functional patterns. For example, a patient with a hypoactive orbicularis oris muscle tends to keep his or her lips apart. The mentalis muscle is used as a compensatory muscle to allow lip closure (Delaire, '78). The lower labial pads of the FR-2 act as an inhibitor of the compensatory mentalis muscle activity, and force the retraining of the orbicularis oris musculature to produce lip seal. The lower labial pads do not act as a lip bumper, and are not designed to stretch the orbicularis oris muscle.
Patients who have hyperactive cheek musculature can also be treated with a Frankel appliance. The buccal musculature is retrained by the vestibular shields of the FR-2, and the amount of cheek pressure against the teeth is reduced. This results in a spontaneous increase in arch width, leading to a decrowding of the dentition in many instances (Frankel, '71, '74). Clinical evidence of the effect of the appliance on the buccal musculature is seen in the use of cheek retractors. Often at the beginning of treatment, you can barely use large cheek retractors for intraoral photography. After four or five months of Frankel treatment, you can retract the cheeks quite easily.
DR. GOTTLIEB Is this due to the stretching of the tissues?
DR. MCNAMARA It seems to be the result of a long-term, low-grade stretching of the muscles. The shields may also act on some of the soft tissues that are nonmuscular, such as connective tissue.
DR. GOTTLIEB In treating cases with hypotonic lips, a lip exercising program is necessary in addition to the Frankel appliance, is it not?
DR. MCNAMARA Yes. Frankel has emphasized the importance of adequate lip seal as an integral part of functional therapy. The patient must breathe nasally with lips together, thereby eliminating abnormal muscle activity. This can be accomplished with lip exercises, which are started the very first day the patient comes into the practice. My staff and I are constantly reminding the patient about keeping his or her lips together. This is reinforced with a program of lip seal exercise. Atongue blade or toothpick is held lightly between the lips for at least 30 minutes a day during quiet times such as when the patient is watching television or reading. Frankel has shown someremarkable changes in facial development in patients just by having them do lip seal exercises without an appliance (Frankel, '80).
DR. GOTTLIEB The appliance reduces the hyperactivity of the mentalis muscle by positioning the jaw forward and making it unnecessary to activate the muscle to close the lips?
DR. MCNAMARA Correct. The forward bite produced by the appliance in Class II cases will, by necessity, bring the structural elements of the face into balance and make it easier for the patient to keep the lips together. The appliance also helps eliminate, in part, some of the abnormal muscle function and allows for the development of the jaw structure in a way that would not have occurred without treatment.
DR. GOTTLIEB Do the vestibular shields only keep the hypertonic muscles away from the teeth, thereby increasing the volume of space between teeth and cheeks, or are they also involved in stretching the muscle attachments, which contributes to arch expansion?
DR. MCNAMARA Frankel hypothesizes that the vestibular shields have a number of functions, one of which is to keep the cheek musculature away from the teeth, and retrain it to act with a more relaxed level of tonicity. Frankel also maintains that, if the shields are extended superiorly and inferiorly a sufficient amount, there will be increased tension on the periosteum adjacent to the alveolus, which will result in bone deposition along the lateral aspects of the maxilla.
DR. GOTTLIEB Is there any evidence that this happens?
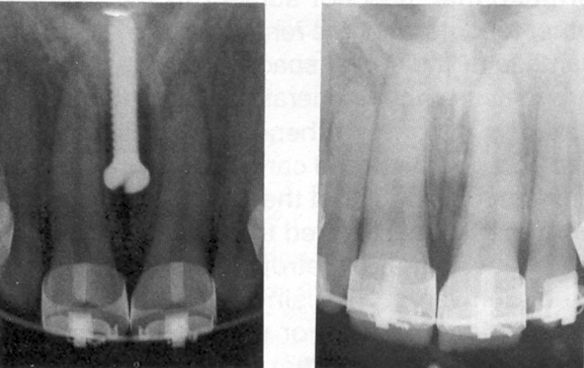
DR. MCNAMARA We have been investigating this phenomenon in a clinical study at the University of Detroit (Brieden, '81). Metallic implants were placed in the maxilla of 12 Frankel patients and the amount of expansion that occurred was monitored, comparing growth at the midpalatal suture to the growth along the lateral aspects of the maxilla. The results of the study indicate that there is only a modest amount of expansion in the suture, and that the majority of the expansion occurs laterally in the alveolar region. This initial study seems to indicate that Frankel hypothesized correctly, but further experimental and clinical studies will have to be done before the relative contributions of sutural growth and alveolar remodeling in maxillary expansion can be clearly delineated.
DR. GOTTLIEB So, the FR-2 differs from other functional appliances because the vestibular shields of the FR-2 keep the cheek muscles away from the teeth, creating space into which the maxillary arch can expand to its full potential. In addition, the stretching action on the cheeks loosens the tissues and causes bone deposition on the lateral aspects of the maxilla by the pull of the periosteum. Is that a fair statement of how the expansion function of the FR-2 works?
DR. MCNAMARA I think so. Another aspect of arch expansion is the role of the tongue. One of the unique advantages of the FR-2 is that lingual volume is not compromised to any great extent. The activator, bionator, and other types of applicances restrict the tongue and decrease the lingual volume (Graber and Neumann, '77). In a Frankel case, the tongue probably plays a role in the expansion of the maxillary arch.
DR. GOTTLIEB How much expansion are we talking about?
DR. MCNAMARA In 1979, Mike Dierkes, Bob Scholz, and I went to East Germany and examined approximately 75 of Frankel's patients and the records on hundreds more. We selected 20 representative cases averaging 4½ years out of retention and measured arch widths. The average expansion was 3.0mm across the upper cuspids, 5.7mm between the upper first bicuspids, and 4.5mm between the upper first molars.
DR. GOTTLIEB It is interesting that the greatest expansion occurred in the upper bicuspid region. If I am not mistaken, that coincides with something Dr. Crozat said a long time ago, and which was a cornerstone of his treatment concept. How do the numbers you just mentioned relate to what would have occurred without treatment?
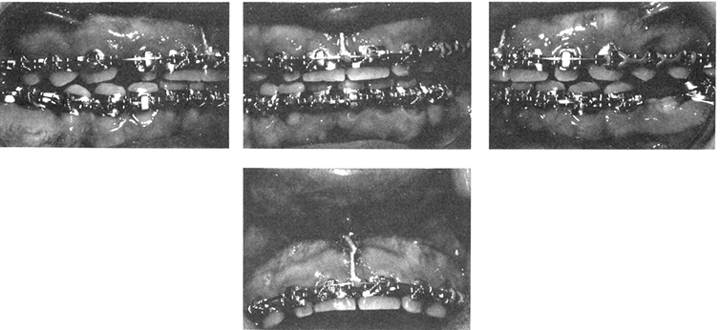
DR. MCNAMARA Paul McDougall, Mike Dierkes, and I (McDougall et al, '82) have recently completed a study of dental arch dimension changes on 60 Frankel cases. We compared the treated cases to 47 untreated Class II's from the University of Michigan Growth Study. Increased arch width was a consistent finding, although the absolute values were slightly less than the amount of expansion reported by Mosch (cited in Frankel, '71) and slightly less than the values we saw in the cases treated in Zwickau. In our American Frankel sample, maxillary width increases averaged 2.1mm to 4.2mm, while the control group averaged between 0 and 1mm.
DR. GOTTLIEB What happened in the mandible?
DR. MCNAMARA In Frankel's cases, there was an average width increase of 2.1 mm in the lower cuspid region, 4.4mm in the lower bicuspid region, and approximately 3mm in the lower molar region. In the American Frankel sample, there was an average of 1mm of width increase across the cuspids (although the maximum increase was 3.7mm), 3 to 4mm between the bicuspids, and 2.7mmbetween the first molars. In contrast, the control group actually showed a 0.4mm loss in the lower cuspid region and 1mm to 1.5mm increase between the lower first molars.
DR. GOTTLIEB Are these width increases permanent?
DR.MCNAMARA Evaluating long-term stability was one of our primary concerns in looking at Frankel's cases in Zwickau in 1979. We were able to document that, on the average, there was very minimal change in the amount of arch width 4½ years postappliance.
DR. GOTTLIEB Do the post-treatment arch forms bear any resemblance to anything that we'd think of as treatment goals in the United States?
DR. MCNAMARA Frankel's post-treatment arch forms bear some resemblance to the Brader arch form. They tend to be very broad in the bicuspid region and are quite different from the typical, ideal arch form that I was exposed to in my orthodontic training. It should be emphasized that the placement of an archwire to achieve a broad arch form is not analogous to the passive development of the same arch form which results when a Frankel appliance is used. In the first case, the archwire actively determines the placement of the teeth through the force generated by the archwire. In contrast, the arch form typically found in Frankel patients presumably results from a change in the balance of muscular forces in the oral region (e.g., cheek, lips, tongue). The long-term stability of the arch form seen in Frankel patients probably is a result of the retraining of the musculature, which does not occur when traditional fixed appliance therapy is used.
DR. GOTTLIEB We have been speaking about the FR-2 appliance. For what kinds of cases is it used, and what are the other Frankel appliances?
DR. MCNAMARA About 90% of the Frankel appliances in use in the United States are FR-2s. They have been used in Class II division 1 and division 2 cases, and some open bite cases. The FR-3 has been used in Class III cases, and the FR-4 in open bite cases. The FR-1 has fallen by the wayside, but it is so similar to FR-2 that it could be used interchangeably in most instances.
DR. GOTTLIEB Why has the FR-1 been discarded?
DR. MCNAMARA One reason that the FR-1 (Frankel, '74) is no longer used lies in the nature of the cuspid clasps. In the FR-1, the cuspid clasp goes interproximally between the canine and first deciduous molar (or first premolar), and then recurves anteriorly on the labial surface of the upper cuspid. When I began using Frankel appliances, I used the FR-1, but I found that during the transition of the dentition, the erupting permanent cuspid often became trapped by the cuspid clasp, which then actually inhibited the eruption of the upper cuspid rather then helping it. I now recognize that this was appliance mismanagement, but I found it easier in this respect to use the FR-2. Also, the incisors are more easily stabilized with the upper lingual wire, which is present on the FR-2 (Fig. 1) but not on the FR-1.
DR. GOTTLIEB I believe that Frankel used the FR-2 on Class II division 2 cases because he used the lingual wire for tooth movement to correct the angulation of the upper incisors. Since American orthodontists would more often use fixed appliances for this purpose, what does the lingual wire do now?
DR. MCNAMARA I've talked with Frankel about that, because I have heard the idea you just expressed many times. According to Frankel, until about three or four years ago he did not have access to fixed appliances. In a Class II division 2 case he usually found it more practical to use some kind of removable palatal plate with finger springs to move the upper incisors outward. So, what was called the "protrusion bow" of the FR-2 (which we now call the upper lingual wire) has really not been used for protruding incisors. I think that the FR-2 is a better appliance for the Class II patient, because the lingual and labial wires provide stabilization labiolingually and very little incisor movement occurs.
DR. GOTTLIEB Are there many cases that you would treat entirely with a Frankel appliance?
DR. MCNAMARA Only a very small percentage of cases can be treated with the Frankel appliance alone. Fixed appliances are almost always used after the Frankel phase of treatment, and about half of our patients are undergoing a sequence of fixed appliance therapy before Frankels are used.
DR. GOTTLIEB How much do you try to accomplish with fixed appliances before beginning Frankel therapy?
DR. MCNAMARA Preparation of a case for the Frankel appliance is similar to the preparation for a surgical case. The dentition is prepared in the anteroposterior, vertical, and transverse dimensions so that it is possible to achieve the proper skeletal changes. Tooth movement is accomplished with fixed appliances before Frankel therapy; and a jaw movement, including skeletal and muscular changes, is accomplished with the functional orthopedic appliance.
DR. GOTTLIEB Are you trying to create with the fixed appliance two good arch forms with relation to their respective jaws, and with the Frankel a width that would fit properly in a Class I molar relationship?
DR. MCNAMARA Not always. I would try to establish the proper anteroposterior and vertical positioning of the teeth before using the Frankel. I like to have the upper incisors a little bit too far forward and the lower incisors a little bit too far backward, in order to maximize skeletal change. I also determine whether the vertical dimension will be proper when the incisors are ultimately brought into an end-to-end position, either initially in a mild Class II or in steps in a severe Class II. Usually, I like to see the tip of the upper incisor 2 to 3mm below the lip at rest. If the upper incisor is extruded, I will intrude it to the desired level.
DR. GOTTLIEB Is the positioning of the incisor related to lip function?
DR. MCNAMARA Yes, if a patient has hypoactive lips, the orthodontist must be careful not to intrude the upper incisors too much. When the lips become more competent, you may actually bring the lip line down to a certain extent. So, there is a certain amount of clinical judgment involved in this area.
DR. GOTTLIEB What are the considerations in setting up the lower arch for Frankel therapy?
DR. MCNAMARA In the lower arch, the orthodontist must determine whether or not to intrude the lower incisor before beginning with Frankel therapy. This is an extremely important point. Determining whether or not the lower incisors should be intruded is based not as much on the functional occlusal plane as it is on the pretreatment anterior facial height and the anterior facial height that will be achieved when the mandible is positioned ultimately in an end-to-end incisor position. Patients who have normal or even excessive anterior facial height at the beginning of treatment may require intrusion of the lower incisors. If the patient has a deficient anterior facial height but overerupted lower incisors, the last thing the clinician wants to do is to intrude these teeth. It would be better to position the incisors edge-to-edge with the Frankel, and allow the posterior teeth to erupt during the Frankel phase of treatment.
DR. GOTTLIEB Does using fixed appliances and leveling the curve of Spee before using the Frankel appliance make American Frankel treatment more effective?
DR. MCNAMARA I think so. American orthodontics now has reached the point at which, by first setting up the case properly, the Frankel can be used as a true orthopedic appliance.
DR. GOTTLIEB You mentioned the anteroposterior and vertical dimensions as considerations in planning the initial fixed appliance phase. What about the transverse dimension?
DR. MCNAMARA If a crossbite is the only problem to be corrected, I probably would not correct it with fixed appliances, unless it was very severe, because the Frankel routinely will allow 3 to 5mm or more of increased arch width. As a practical matter, if I am going to intrude incisors or make other corrections, I usually use a quadhelix appliance or a rapid palatal expansion appliance to correct the crossbite, if for no other reason than to lessen treatment time.
DR. GOTTLIEB What is the relationship of early expansion with a quadhelix or rapid palatal expansion appliance to later expansion with a Frankel?
DR. MCNAMARA I don't know. I expect that it might result in less additional expansion later on.
DR. GOTTLIEB The quadhelix and rapid palatal expansion appliances mainly affect the suture, while the Frankel mainly affects the lateral borders of the maxilla. Maybe you get the best of all possible worlds.
DR. MCNAMARA That might be the case.
DR. GOTTLIEB Does Frankel still use the FR-1 a lot?
DR. MCNAMARA From my recent correspondence with him, I think that he does.
DR. GOTTLIEB Doesn't he have the same problem with the cuspid clasp that you mentioned before?
DR. MCNAMARA The cuspid clasp does go interproximally between the C and D, as I said, but it does not touch the cuspid. It is usually 2 to 3mm away. The problem is that it may inhibit eruption of the permanent cuspid, if not enough attention is paid to it.
DR. GOTTLIEB If it doesn't touch the cuspid, what is the purpose of the cuspid wire?
DR. MCNAMARA Cuspid clasps in both FR-1 and FR-2 are more or less extensions of the vestibular shield, and they act to keep the soft tissue away from the cuspid. In East Germany, the cuspid clasp in the FR-1 is used to guide the eruption of the cuspid; in the FR-2, it is strictly an extension of the vestibular shield.
DR. GOTTLIEB But you would not use the cuspid clasp as a tooth mover?
DR. MCNAMARA In certain instances, if the cuspid is labially positioned and the orthodontist didn't want to use fixed appliances at that point, he or she might use it as is or with a finger spring to tuck in the cuspid. However, I would usually use fixed appliances to do it.
DR. GOTTLIEB Do you ever use the labial wire of the FR-2 as a tooth mover?
DR. MCNAMARA One of our biggest sources of error when we began using the Frankel appliance was the labial wire. We could obtain dramatic changes in the incisor overbite and overjet by tipping them with the labial wire. However, we very rapidly discovered that this was not a good thing to do, because the excessive lingual tipping was compromising the achievement of a change in skeletal relationship. We tried for a while to have the labial wire lie slightly away from the incisors, but now we have it lie passively against the teeth.
DR. GOTTLIEB That is just for stabilization?
DR. MCNAMARA The labial and lingual wires together act as a guide for closure. The labial and lingual wires and the interproximal wires that lie between the canine and first deciduous molar (or first bicuspid) and between the second deciduous molar (or second bicuspid) and first permanent molar, form a positive lock on the maxilla and allow for the maximum amount of forward mandibular growth. In addition, these wires act as occlusal rests, as well as an anteroposterior lock.
DR. GOTTLIEB What is the purpose of the lower lingual springs (Figs. 1E,F)?
DR. MCNAMARA In the past the lower lingual springs were used to produce slight tooth movement, but since we are often now banding cases prior to placement of a Frankel appliance, the lingual springs are used mostly to stabilize the lower incisors, both horizontally and vertically. The springs pass along the lingual surface of the incisors at the level of the cingulum and stabilize the incisors against distal movement, and, in certain instances, prevent further eruption of these teeth. In many cases the lower lingual springs are not needed.
DR. GOTTLIEB Is the position of the lower lingual shield (Figs. 1E,F) important?
DR. MCNAMARA Yes. It is extremely important, when fabricating the appliance, to make sure that the lower lingual shield does not touch the margin of the lingual gingiva, and that the lower labial pads do not touch the margin of the labial gingiva, or stripping of the gingiva may occur.
DR. GOTTLIEB What is the importance of the lower labial pads (Figs. 1A,B)?
DR. MCNAMARA The lower labial pads have proven to be the most difficult part of the appliance to manage clinically. They should be teardrop in shape, not rectangular, in the sagittal dimension (Fig. 6). The teardrop shape allows proper positioning of the pads in the labial sulcus, and prevents gingival stripping when the appliance moves and the jaw opens and closes. This shape also allows for a more comfortable fit for the patient, by allowing the pad to tuck into the undercut below the incisors. The orthodontist must also make sure that there is enough space between the lower labial pads and the vestibular shields to allow room for the attachment of the lateral frenum. Otherwise, sore spots may occur.
DR. GOTTLIEB What wires are present posteriorly?
DR. MCNAMARA The occlusal rest-palatal wire (Fig. 1C and 1D) begins as an occlusal rest on the upper first molar, extends superiorly and anteriorly, and then recurves through the interproximal space between the upper first molar and the upper deciduous second molar, crosses over the palate, and travels a similar path on the opposite side. The occlusal rest prevents superior displacement of the appliance and inhibits the eruption of the first molar. The interproximal portion of the wire usually inhibits the eruption of the second deciduous molar, and helps provide an anteroposterior lock.
DR. GOTTLIEB You mentioned that the occlusal rest-palatal wire recurves interproximally to form an anteroposterior lock. How does it fit interproximally?
DR. MCNAMARA The lingual wire and the occlusal rest-palatal wire form the anteroposterior lock. To lodge them interproximally, it is necessary to prepare the teeth when the appliance is delivered. This is done in my office with a diamond cylinder bur in a high speed handpiece. Placing the bur in the interproximal space between the upper cuspid and first deciduous molar, a groove is made in the deciduous teeth at least 2mm or more down from the occlusal surface to the gingiva. The same is done on the distal surface of the deciduous second molar.
DR. GOTTLIEB Is the same instrument used to notch the teeth on the model?
DR. MCNAMARA No. Usually the teeth on the model will be notched with a knife or a file by the laboratory technician. When the appliance is returned from the lab, it is the clinician's job to duplicate in the mouth the notches on the teeth on the model.
DR. GOTTLIEB The clinician does not notch the teeth before taking the impression?
DR. MCNAMARA No. If that is done, the spaces often close by the time the appliance is returned from the lab. I find it is convenient to notch the teeth at the time of appliance delivery.
DR. GOTTLIEB But you would not notch permanent teeth, would you? How do you handle cases in the permanent dentition?
DR. MCNAMARA When a Frankel appliance is going to be used in a permanent dentition case, the permanent teeth obviously are not notched. Separators are used in the appropriate areas, or a transpalatal (Goshgarian) arch is attached to the molars to provide some space through molar rotation. However, it should be noted that when the appliance is fabricated, the permanent teeth on the working model are notched, so that the appliance gradually seats itself as it is being worn.
DR. GOTTLIEB Is the purpose of the notching to create the interproximal anteroposterior lock to bind the upper arch together, or to stabilize the appliance, or both?
DR. MCNAMARA Frankel has said that the purpose of the anteroposterior lock is to prevent the maxillary teeth from tipping lingually. At one time in this country we stopped doing the notching. We weren't too keen on using a handpiece in the mouth, and we decided among ourselves that it didn't make any difference. In looking at the treatment results of the cases which were not notched, it became very apparent to me that many of the major changes occurred in the maxilla and not in the mandible, and that the reason for this was that the appliance was being displaced posteriorly on the maxilla and tipping the upper incisors lingually. So, maxillary change and dentoalveolar change was produced before mandibular change. Since I have resumed notching, I have seen much less lingual tipping of incisors, and the skeletal growth results are far more gratifying.
DR. GOTTLIEB I imagine that you must have a good relationship with a laboratory in order to get the Frankel appliances constructed properly.
DR. MCNAMARA In the beginning, there were very few places to get the laboratory work done, and the laboratories were struggling, as we were, with the design and fabrication of the appliance. More recently, the construction of the FR-2 has been worked out, and it is now available in published form (McNamara and Huge, '81) and on a videotape sequence. A number of competent laboratory technicians are now able to fabricate an acceptable FR-2. When giving instructions to the laboratory, we usually specify a standard design.
DR. GOTTLIEB Is it feasible to do this in your own laboratory?
DR. MCNAMARA I think it is possible, but I would suggest that a novice deal with a major laboratory for a while.
DR. GOTTLIEB Have there been any significant design changes?
DR. MCNAMARA Most of the current changes in appliance design in reality have been a return to Frankel's original design of the appliance. During Frankel's last visit to the United States in 1980, he was critical of our vertical placement of the labial lip pads, saying that they were too close to the gingival margin and not placed deeply enough in the sulcus. Frankel has said that the support wires of the lower labial pad should be 7mm below the gingival margin. I now use a slightly different guideline - that the bottom of the pad should be 12 to 14mm below the gingival margin at the level of the lateral incisor. Also, I went through that period during which I was not notching the teeth and not carving the work models. Because of that, I was not getting sufficient extension of the vestibular shields. All three of these errors have now been corrected.
DR. GOTTLIEB Did you find that those design errors affected your treatment results significantly?
DR. MCNAMARA Yes. Many of the cases treated when I was not making the labial pads low enough still had obvious mentalis hyperactivity at the end of the treatment. In addition, I discovered that although I got a very substantial amount of expansion posteriorly (3.5mm to 4.5mm), it was somewhat less than I had observed in the cases we measured in Frankel's clinic in East Germany.So, now models are carved to maximize the tissue extension from the vestibular shields.
DR. GOTTLIEB What do you mean by "carving the models"?
DR. MCNAMARA The impression area is extended by carving the sulcus areas deeper on the model. We are still trying to develop new impression trays and impression techniques to minimize the amount of carving, but I am still carving the models to some extent on every Frankel case.
DR. GOTTLIEB In making the bite registration for the FR-2, do you position the lower jaw forward all the way to an end-to-end relationship?
DR. MCNAMARA If the patient is a severe Class II, the mandible should be brought forward in steps. In fact, Frankel believes that several advances of the appliances in small increments is the best possible way of achieving the physiologic response. He recommends that the bite only be brought forward 2 or 3mm every four or five months. I have almost always advanced the appliance 4 to 6mm at any one time, and I've found that patient tolerance and cooperation have been excellent. However, the exact amount of advancement is still open to question. No definitive studies have been published on the subject of how much the bite should be advanced at one time. In any case, most Frankel practitioners agree that a bite registration of more than 6mm forward is not well tolerated by most patients. Thus, in severe cases the bite should be advanced in steps.
DR. GOTTLIEB Does that require a remake of the appliance?
DR. MCNAMARA Not necessarily. The labial and lingual pads can be brought forward as a unit, by cutting the vestibular shield between the extension of the crossover wire and the upper lingual wire with a crosscut fissure bur (Fig. 7). The cut is extended downward, so that the acrylic is freed, but the extension of the crossover wire is still embedded in the buccal shield. The lower anterior part of the appliance can then be slid forward, with the .051" crossover extension as the guide wire. The anterior assembly is advanced the desired amount, the space between the acrylic parts is refilled with cold-cure acrylic, and the shields are re contoured. This is called "advancing the Frankel".
DR. GOTTLIEB I believe that the alignment of the two jaws is on the skeletal midline rather than the dental midline. What happens with the teeth? Do they somehow align themselves?
DR. MCNAMARA You are correct that the alignment of the bite is on the skeletal midline. Sometimes, when the skeletal midlines are lined up, the dental midline problem will straighten itself out, at least in part. However, dental midline problems can be solved most easily with fixed appliances, either before or after Frankel treatment. In any event, under no circumstances should an attempt be made to correct an asymmetrical dental midline with the Frankel appliance, because the end result will be an asymmetrical face. Similarly, if the mandible is symmetrical, and the maxilla is asymmetrical, a Frankel should not be used to correct the asymmetry.
DR. GOTTLIEB What about the unilateral Class II's?
DR. MCNAMARA Many unilateral Class II's that I have seen have been cases in which there was premature loss of an upper second deciduous molar, and the adjacent first permanent molar has rotated forward on one side. Most of these should be corrected in the pre-Frankel orthodontic stage, with a transpalatal arch or a similar appliance. In the pre-Frankel stage, I make extensive use of the utility arch for incisor intrusion, and the transpalatal arch for correcting molar rotations. In doing so, space often opens between the first molar and second deciduous molar, which allows the palatal wire of the FR-2 to be seated in that area.
DR. GOTTLIEB I think we ought to refer anyone who wants more details on the construction of the FR-2 to your recent article in the American Journal of Orthodontics (McNamara and Huge, '81). Let's go on to the FR-3. When is it used?
DR. MCNAMARA The FR-3 appliance (Fig. 8) is used in Class III cases that are characterized, at least in part, by a skeletal maxillary deficiency. In some respects, it is like an FR-2 turned upside down. The labial pads lie in the upper region, rather than in the lower region.
DR. GOTTLIEB What is the purpose of the upper labial pads?
DR. MCNAMARA The purpose of the upper labial pads is to inhibit the function of the upper lip, thereby allowing the downward and forward growth of the maxilla to occur unimpeded. The force of the upper lip is transferred through the appliance to the mandible, although there is little evidence that the FR-3 significantly inhibits mandibular growth.
DR. GOTTLIEB No lip bumper effect?
DR. MCNAMARA Apparently not.
DR. GOTTLIEB Is there space between the tissues and the plastic of the shields and pads?
DR. MCNAMARA The FR-3 is constructed so that the shields and pads in the upper arch stand about 3mm away from the alveolus. In the lower arch, there is no wax relief used in the construction of the shields, so the shields fit snugly on the mandible. In contrast, the FR-2 has 3mm of relief in the height of the maxillary vestibule and 0.5mm in the mandibular sulcus. In both appliances, the pads should be parallel to the alveolus (usually vertical in the FR-2 and angled in the FR-3) and have a gentle teardrop shape in the sagittal dimension, to facilitate insertion and removal of the appliance and to prevent gingival stripping. The upper labial pads of the FR-3 should be extended quite far superiorly into the sulcus under the nose
DR. GOTTLIEB What are the differences in wire construction between FR-3 and FR-2?
DR. MCNAMARA The upper lingual wire in the FR-3 is an .036" stainless steel wire, which originally was used to protrude the upper incisors, but which now acts primarily as a vertical stop. The palatal wire is made of .045" stainless steel and passes across the palate, extending from one buccal shield across the palate to the other buccal shield. In contrast to the FR-2, in which the palatal wire lies in the interproximal area between the upper second deciduous molar and first permanent molar, the palatal wire in the FR-3 passes behind the last molar, in most instances the upper first molar.
DR. GOTTLIEB If Harvold's observation is right about relative eruption of molars, and I believe that it is, wouldn't it work better not to have the occlusal rest of an FR-3 on the upper molar, but to have it on the lower molar?
DR. MCNAMARA Well, in fact, there is an occlusal rest on the lower molars. The occlusal rest on the upper molars is optional and is used only to maintain an open bite anteriorly when anterior crossbite needs to be corrected. In contrast to the maxillary occlusal rest of the FR-2, which lies in the buccal groove between the mesial and centrobuccal cusps of the upper first molar, the maxillary occlusal rest of the FR-3 originates posteriorly to the upper molar, and extends anteriorly along the central groove. If there is no anterior crossbite involved with the Class III, or as soon as the anterior crossbite is corrected, the upper rest is removed. This is consistent with Harvold's thinking.
DR. GOTTLIEB What are the other wires on the lower portion of the FR-3?
DR. MCNAMARA On the mandible there are two wires: the occlusal rests mentioned earlier and the lower labial wire. The lower labial wire, made of .045" or .051" stainless steel, is not an active wire; it is primarily a passive support wire. However, a small series of notches can be placed on the work model across the central incisors, so that when this wire is fabricated, it can generate some pressure against the lower anteriors, if these teeth are to be moved lingually.
DR. GOTTLIEB How does the FR-3 work?
DR. MCNAMARA The exact mechanism by which the FR-3 works is not fully understood. It will take implant studies to determine what the mechanism really is. It is thought that the main effect of the FR-3 is that of eliminating the lip pressure on the maxilla with the upper labial pads and permitting the maxilla to move anteriorly. Whether the maxilla actually moves forward or whether there is bone deposition on the anterior aspect of the maxilla is not clear.
DR. GOTTLIEB If the maxilla moves forward to the limit of the appliance and more anterior movement is needed, I presume that the FR-3 can be advanced in a manner similar to that of the FR-2.
DR. MCNAMARA The FR-3 can be activated, but not in the same way as the FR-2. To advance the FR-2, the vestibular shields are split (Fig. 7). In the FR-3, only the upper labial pads are moved forward, usually after four to six months of full-time wear. To activate the appliance, the distal ends of the upper labial support wires are freed from the vestibular shields with a bur, and the pads are moved forward, so that the 3mm distance between the pads and the alveolus is restored. The holes in the vestibular shield then are refilled with acrylic.
DR. GOTTLIEB You said earlier that the FR-4 is used in open bite cases?
DR. MCNAMARA It is used in open bite cases in which there is no anteroposterior discrepancy.Therefore, it is constructed so that the mandible is in a comfortably retruded position. There is no attempt to posture the mandible forward. There are no lower lingual pads, but the FR-4 does have labial pads on the lower arch or on the upper arch or on both.
DR. GOTTLIEB How does the FR-4 work?
DR. MCNAMARA The FR-4 is essentially an exercise appliance that stimulates perioral muscle function, but does not interfere with tongue function.
DR. GOTTLIEB It is interesting that other removable appliances used to treat open bite cases are designed to interfere with tongue function.
DR. MCNAMARA Frankel has shown some remarkable changes using the FR-4. I have seen many cases in which he has clearly documented a closure of the mandibular plane angle of up to 10 degrees during the growth period. This closure is far greater than that which occurs during normal growth.
DR. GOTTLIEB How does the FR-4 overcome tongue thrust in open bite cases?
DR. MCNAMARA I think that Proffit ('78) and others have shown that the tongue is an extremely adaptable organ, which, in the vast majority of cases, is probably not the prime cause of the open bite. This is not to discount those cases that have a true neuromuscular problem that is causal; but, for the most part, tongue thrust seems to be a secondary and compensatory aspect of another problem, such as airway obstruction or enlarged tonsils. Frankel's rationale for the use of the FR-4 in open bite cases is that the key to a successfully treated open bite is the establishment of a proper oral seal, proper nasal respiratory patterns, and a proper level of perioral muscle function. In a growing individual, an FR-4 promotes closure of the bite by a true forward rotation of the mandible, and a change in the growth axis. This is remarkable, when compared to the lack of success of other treatment methods. For further information on this subject, the reader is directed to the article by Professor Frankel and his daughter in an upcoming issue of the American Journal of Orthodontics (Frankel and Frankel, '82).
DR. GOTTLIEB What percentage of the patients in your practice get an FR-2?
DR. MCNAMARA I use the Frankel appliance in about 20% of my patients. A third of my practice consists of adult patients, many of whom are orthognathic surgery patients. Functional appliances are rarely used in adult patients in my practice. Another third of my patients are the traditional adolescent patients, and approximately 10% of them get a Frankel or some other type of functional appliance. The remaining third are Class II and Class I crowded mixed dentition cases. Probably 75% of these Class II cases are treated with a Frankel. I am not yet encouraged about using an FR-2 in a Class I crowded case. The few that I have tried have not been as successful as I would like. I don't think that the patients are motivated as much. They do not necessarily look better with the appliance in, and sometimes they look worse. The Frankel appliance will not decrowd a severely crowded arch
DR. GOTTLIEB Jim, let's get into the clinical management of the FR-2 and the Frankel patient.
(TO BE CONTINUED)