JCO Interviews Dr. Eugene H. Williamson on Occlusion and TMJ Dysfunction, Part 2
DR. BRANDT Gene, have you found that the growth pattern has any correlation with the incidence of dual bite, prematurities, etc.? Do high angle patients have a greater incidence of molar prematurities?
DR. WILLIAMSON Yes, Sid. Class II vertical patterns seem to be the real problems. Studies have shown that open bites (no anterior guidance) and deep bites (too much anterior guidance) display symptoms most frequently.
DR. BRANDT What are the orthodontist's treatment options for a posttreatment dual bite?
DR. WILLIAMSON My first question is, "Does the patient have symptoms?" If he does not, a simple explanation to the patient may be in order. I would not intimate to the patient that this was a fault of treatment; only that a skeletal discrepancy is present that could have resulted from a lack of proper growth. If any symptoms should develop in the future, the patient should return to the orthodontist's office for treatment. This approach relates to the patient being properly informed. If, on the other hand, the patient is symptomatic, treatment may be in order.
DR. BRANDT What treatment?
DR. WILLIAMSON It should begin with a mandibular repositioning splint. When symptoms have subsided, models should be properly mounted, and a new diagnosis and treatment plan formulated. A least invasive approach to treatment should be followed.
DR. BRANDT Does this apply to all classes of patients--I, II, III? Deep bite and open bite?DR. WILLIAMSON Yes. Usually, the patient seen with a dual bite will originally have been Class II.
DR. BRANDT Can a bite plate be used in place of a repositioning splint?
DR. WILLIAMSON I do not use a traditional orthodontic bite plate. In such an appliance only the anterior teeth touch. This type treatment may allow posterior teeth to erupt, and active movement is therefore instituted. The appliance which I use has been referred to as a bite plane or mandibular repositioning splint. It is made on the maxillary arch by forming a heat softened plastic template on a model of the patient's mouth. The template is trimmed and placed on a second model, which is articulator-mounted. It is adjusted, by grinding, until a minimum vertical opening is achieved (approximately .5mm thickness between first tooth contact). Autocuring acrylic is added to the template and the articulator closed to the previously established vertical dimension. After the acrylic sets, the splint is adjusted by grinding to the following specifications:
1. All teeth contact evenly at centric relation. Only the buccal cusps of the mandibular posterior teeth contact. The contact for each cusp tip is very small. The anterior teeth contact very lightly.
2. The cuspids and incisors disclude all the posterior teeth in any eccentric movement. This is achieved by means of a gentle incline plane for anterior guidance.
DR. BRANDT What are the objectives of this appliance?
DR. WILLIAMSON No orthodontic tooth movement should be achieved. By removing the ability of the patient to return to his tooth-dictated maximum intercuspation position, the programmed neuromuscular reflex from periodontal ligaments to the muscles by way of the CNS will be eliminated. This reflex causes specific motor units in the muscles to predominate, thereby positioning the mandible so that the teeth will maximally intercuspate without discomfort. Usually, it requires the condyles to be eccentrically placed. By means of the splint, the neuromuscular reflexes will change, gradually allowing the condyles to migrate towards a seated position, dictated by balanced muscle contraction. As the muscles change the condylar position, the teeth will no longer contact the splint as they originally did. Therefore, the splint is adjusted at frequent appointments to the previously mentioned criteria by grinding. When the patient becomes stable on the splint, that is, no more adjustments are required to remove deflections, the mandible is considered to be at centric relation.
DR. BRANDT For how many hours do you prescribe the splint be worn?
DR. WILLIAMSON I ask the patient to wear the splint 24 hours per day.
DR. BRANDT Does wearing the splint usually provide immediate relief?
DR. WILLIAMSON Quite frequently we see immediate relief. It depends upon the severity of the dysfunction.
DR. BRANDT What if the splint does not relieve the symptoms?
DR. WILLIAMSON Most people will make improvements. When a patient does not improve, I assume the occlusion of the teeth and jaws is not the etiology of the patient's pain. Therefore, occlusal therapy is not instituted. The patient is then referred to another discipline for diagnosis.
DR. BRANDT If relief does occur promptly, does this prove that the occlusion was the primary cause of pain?
DR. WILLIAMSON Yes, that the occlusion was at least closely associated with the problem. If the patient remains stable on the splint, diagnostic procedures are begun to determine the least invasive therapy.
DR. BRANDT How long should the splint be worn before performing an occlusal analysis?
DR. WILLIAMSON At least until the patient remains asymptomatic and stable for six to eight weeks.
DR. BRANDT At what point should the plaster casts be mounted on an articulator to perform the occlusal analysis?
DR. WILLIAMSON After the patient is stable for six to eight weeks.
DR. BRANDT What is the main purpose of mounting the casts?
DR. WILLIAMSON The purpose is to diagnose the malocclusion with the mandible at centric relation and to compare that with the occlusion at maximum intercuspation. One is truly the skeletal relationship, while the other is a tooth-dictated position. Dramatic differences are frequently seen in vertical, mediolateral and anteroposterior dimensions. These alarming differences may require entirely different treatment modalities.
DR. BRANDT What are the accepted methods of recording bite registration?
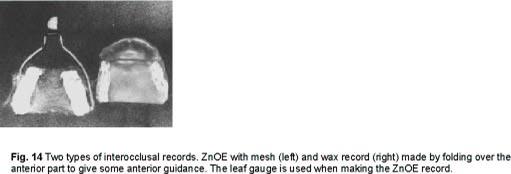
DR. WILLIAMSON There are basically three methods. Wax recordings, mesh and zinc oxide eugenol, and acrylic or impression materials.
DR. BRANDT Which method do you prefer?
DR. WILLIAMSON I prefer the mesh and zinc oxide eugenol method utilizing some type of anterior guide such as the leaf gauge. This type registration has been shown to be the most accurately reproducible (Fig. 14).
DR. BRANDT Should wax setups be done more often?
DR. WILLIAMSON Wax setups should be used in unusual extraction cases.
DR. BRANDT How much adaptability is there to the various dysfunctions? Do many patients just absorb what is wrong and display no significant symptoms?
DR. WILLIAMSON It seems to depend on tissue adaptability, Sid. There is the robust individual to whom it seems almost any trauma is insignificant. Then there are those who respond with tissue destruction. Again, the question of prediction.
DR. BRANDT And, of course, there is an age factor in the degree of adaptability.
DR. WILLIAMSON Yes. It is absolutely amazing how youngsters we treat adapt and respond. The same treatment mechanics applied to a middle-aged patient may not be acceptable. The high degree of metabolic activity associated with adolescents certainly is a factor with adaptability. I think this is one of the reasons that the children may adapt to deflective malocclusions so much better. If overt dysfunctional symptoms appear, it is usually in the twenties and thirties.
DR. BRANDT Do some conditions have transitory pain symptoms?
DR. WILLIAMSON Apparently so, Sid. An example of such a condition would be the person who have deflective malocclusion and is routinely bruxing, but not having overt symptoms. If that person is suddenly placed under a more stressful situation, he may awaken one morning with overt symptoms.
DR. BRANDT How does that happen?
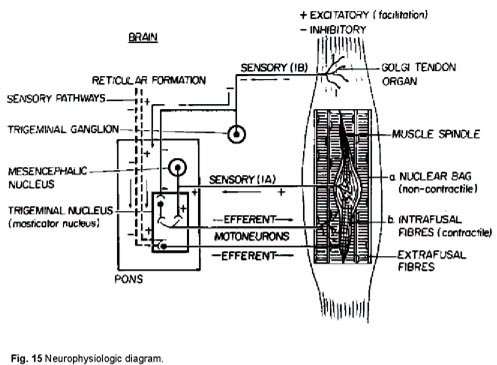
DR. WILLIAMSON I think the neuro-physiologic diagram (Fig. 15) explains the circumstances well. It may be seen that the muscle spindle is connected to the striated muscle fibers by way of the connective tissue perimysium. If the striated muscle fibers are stretched enough, the nuclear bag is stimulated and that initiates a reflex arc. The afferent impulse is therefore initiated and causes the striated muscle fiber in a muscle of mastication to contract in order to prevent that fiber from being injured by overstretching. In the patient who has subclinical symptoms, the bruxing does not overstimulate the muscle spindle and the muscle does not overcontract. Note, however, in the diagram that the muscle spindle itself contains some muscle tissue capable of contracting.
Also, note that the muscle tissue of the spindle has an efferent nerve supply from the motor nucleus of Cranial Nerve V. There seems to be a route of connection between the efferent supply to the spindle and the reticular formation in the hypothalamus. The reticular formation is a very primitive portion of the brain and influences basic physiologic functions, such as blood pressure, heart rate and temperature. When a subject is placed under stress, this area influences these functions. Therefore, if we place a patient, who is already bruxing, under more stressful conditions, the reticular formation may activate the muscle tissue of the spindle and cause it to contract. This places more tension on the nuclear bag, and it takes less stretch of the striated muscle to stimulate a response from the bag itself. Suddenly, then, the striated muscle is forced to contract more often and for a longer duration with the same amount of bruxing. The increased activity in the muscle may result with muscle dysfunction and pain. If the patient is removed from the stressful situation, the influence from the reticular formation may be attenuated and pain may subside.
DR. BRANDT Can the orthodontist judge whether a condition. is temporary?
DR. WILLIAMSON You really are at the heart of the problem, Sid. The orthodontist is not able to predict adequately, at this time, which people can adjust and adapt, and which ones can't. We, therefore, need to eliminate the variable of deflective malocclusion in our treatment.
DR. BRANDT Is mandibular asymmetry a common phenomenon?
DR. WILLIAMSON Very common.
DR. BRANDT What are some of the causes?
DR. WILLIAMSON Genetics, function, and trauma.
DR. BRANDT What are some of the clinical implications of mandibular asymmetry?
DR. WILLIAMSON When an asymmetry exists, one of the problems the clinician faces is a malocclusion which is more severely Class II on one side. A subdivision case might be an example, or the typical Class II which is accentuated on the side what is less developed. If the orthodontist is treating to a concept of centric relation, he must generally treatment plan the case to have maximum anchorage in the maxillary arch on the deficient side. In some cases, the problem is so severe that he may be fortunate to achieve an end-to-end condition on the short side of the mandible posttreatment.
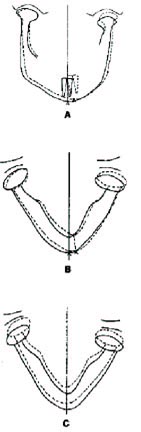
Obviously, as the mandible goes to centric relation, the mandibular teeth become more distally situated compared to the maxillary ones. This also causes a midline discrepancy, with the mandibular midline shifting to the deficient side as the condyles seat (Fig. 16). A good clinical example might be the case in which asymmetric elastics are utilized and the midline will not correct. in the asymmetry study that we did, 32% displayed 3 millimeters or more mandibular asymmetry in the frontal (posterior-anterior) or submental-vertex (basilar) dimensions. Three millimeters is approximately a cusp width, and would make a Class I at maximum intercuspation into a Class II at centric relation. The asymmetries apparently may occur either by means of a deficient mandibular corpus on one side (as viewed on the radiograph from the basilar or submental-vertex relation), or by means of lack of vertical growth in one condyle (as viewed on the posterior-anterior x-ray) (Fig. 16). In either case, the molar and canine relationship is more Class II on the deficient side when the mounted models are assessed.
DR. BRANDT Does a midline discrepancy cause you some special concern?
DR. WILLIAMSON A midline discrepancy may be an indication of an asymmetry. It may indicate that one side of the occlusion will be more Class II than the other. If an asymmetry is present and the operator is treating to a concept of a seated condylar position, he may have to finish the case with one side a little more Case II than the other. An end-to-end molar and canine relationship would be an example. I know, before beginning treatment, that this case will need posttreatment equilibration. The patient is also prepared, by telling him the midline will not be symmetrical posttreatment.
DR. BRANDT If orthodontic therapy is completed with a midline disharmony, is this a harbinger of trouble to come?
DR. WILLIAMSON Only if the case is not properly finished with equilibration.
DR. BRANDT Many orthodontists correct midline discrepancies with heavy directional elastics. Do these heavy elastics have any adverse affect on the TMJ?
DR. WILLIAMSON It is very possible that heavy directional elastics will pull the condyle forward and away from its seated position on the Class II side. The midline discrepancy may be corrected, but one condyle is no longer seated. If no compensatory growth occurs on that condyle, which seems to be the average clinical situation, a deflection from centric relation occlusion to maximumintercuspation is produced. Therefore, when the midline is assessed with both condyles seated, it is still off.
DR. BRANDT If the midline problem is due to a tooth size discrepancy, how do you handle that?
DR. WILLIAMSON Possibly asymmetric extractions in extraction cases, or acceptance of the problem in nonextraction cases, with equilibration indicated posttreatment.
DR. BRANDT What are the most common functional occlusal schemes?
DR. WILLIAMSON Bilateral balanced occlusion, unilateral balanced occlusion or group function, and cuspid disclusion.
DR. BRANDT Please explain "bilateral balanced occlusion".
DR. WILLIAMSON Bilateral balanced occlusion is one in which the maxillary buccal cusp inclines are in even contact with the mandibular buccal cusp inclines on the working side. On the balancing side, the lingual cusps of the maxillary teeth contact the buccal cusps of the mandibular teeth evenly. In protrusive, the most posterior molars in the maxillary arch contact the most posterior molars in the mandibular arch bilaterally.
DR. BRANDT Is this scheme better suited to prosthetics than orthodontics?
DR. WILLIAMSON It has not been successful in dentulous mouths, since even contact along the buccal segments is extremely difficult to achieve and retain. Therefore, one or two teeth tend to take the total load. This may be very destructive, particularly with the EMG evidence accumulating, which demonstrates the accentuated contraction of the pterygomasseteric musculature, when posterior teeth contact eccentrically. Part of the problem stems from the fact that bone will bend. With the heavy forces; the mandible will flex, and it becomes virtually impossible to keep even contact of a buccal segment on the balancing side.
DR. BRANDT Has anyone ever actually measured the amount of bending that occurs in the mandible?
DR. WILLIAMSON Yes, Butler has shown good evidence of mandibular flexure. In his study he measured intermolar distance changes across the mandibular first molars. The greatest change occurred in protrusive (mean decrease of .43mm) and in wide opening (mean decrease of .22mm). However, he saw as much as .75mm decrease in protrusive and .61mm decrease in wide opening for some patients.
DR. BRANDT Can this type of flexure create any additional problems?
DR. WILLIAMSON Yes. I believe it must be considered when we think of fixed, nonflexible retainers. It also makes a difference when you make impressions with the mandible wide open, instead of a more closed position with relaxed suprahyoid and pterygoid musculature.
DR. BRANDT Please explain "unilateral balanced occlusion".
DR. WILLIAMSON Unilateral balance or group function has the cuspids and the maxillary buccal cusp inclines in even contact with the mandibular buccal cusp inclines on the working side. There are no tooth contacts on the balancing or non-working side. There are no posterior tooth contacts in the protrusive movement.
DR. BRANDT Now please explain "mutually protective occlusion".
DR. WILLIAMSON Mutually protective occlusion implies that different segments of the dental arches protect others in specific function. For example, the posterior teeth act as jaw stops on closure. This protects the anterior teeth from detrimental forces. On the other hand, the anterior teeth act as the discluders of the posteriors on any eccentric movement. When the mandible is closed at centric relation, all the posterior teeth contact simultaneously and the anterior teeth are very slightly out of contact. In the lateral excursive movements, the canines accept the majority of the load, with some help from the incisors. In the protrusive movement, the incisors accept the majority of the load, with some help from the maxillary canines and mandibular first premolars. This approach is very similar to canine disclusion. I am not so concerned about the maxillary canines contacting the mandibular first premolars, due to recent EMG evidence. The most important time frame for protrusion is the initial forward movement of the mandible from centric relation occlusion. At this moment, the masseters, medial pterygoids, and inferior heads of the lateral pterygoids are very active. This means heavy forces are acting on the teeth. In a Class I occlusion, these forces are distributed among the incisors and canines initially. Hopefully, the canines absorb the very first load. The more anterior the mandible moves (with no posterior tooth contact), the less activity is seen in the pterygomasseteric sling. Most muscle activity is coming from the inferior heads of the lateral pterygoids. Therefore, there is less force on the anterior teeth. At the end-to-end incisor position, there is minimal activity elicited from the closing muscles. Therefore, my concern is primarily that the incisors are separating the posteriors at that position. An interesting point to note is that, in the protrusive movement, the superior heads of the lateral pterygoids are inactive in the healthy system, until the incisors are end-to-end. At that time, they become active. That would mean the disc is moved anteriorly by its mediolateral anatomical attachments to the condyle, not initially by muscle contraction.
It is my postulation that some joint clicking or anterior disc displacement, may be due to early contraction of the superior head of the lateral pterygoid, since it inserts into the meniscus. This might pull the meniscus forward too early and cause the typical noise. I am presently beginning to work on that project.
DR. BRANDT In each of the three occlusal schemes you explained, where should the condyles be when maximum intercuspal position is attained?
DR. WILLIAMSON I n centric relation, the condyles should be simultaneously in a most superior position on the posterior slope of the articular eminences, with the meniscus properly positioned. Lundeen and Gibbs have demonstrated that the condyles will reach a most superior position on the working side when chewing hard, resistant foods. This may also be interpreted as meaning that a subject's condyle may reach that position when bruxing. If posterior teeth are able to contact prior to the condyle reaching its most superior position, a deflection is present. Bruxism may be thought of as an attempt by the patient to grind the interfering tooth surfaces out of the way, in order for the condyle to have a free path to its most superior position. It has also been demonstrated by Hylander that the TMJ is a load-bearing joint, at least in the rhesus monkey, when chewing. This indicates that the mandibular condyle places pressure on the meniscus and subsequently against the posterior slope of the eminence. Moffett has indicated histologic evidence that the posterior slope of the eminence is, indeed, load-bearing.
DR. BRANDT Some patients display a functional shift prior to teeth meeting. How can that be explained?
DR. WILLIAMSON If the patient is closed to the point that translation is not occurring in the superior parts of the joints, any functional shift prior to tooth contact is generally due to asymmetric muscle contraction or relaxation. There are times when a meniscus anomaly or displacement might be the etiology. When the teeth are not involved, functional shifts are usually seen on opening. An example is a deviation of the mandibular midline to one side on opening. This is usually caused by asymmetric muscle contraction, predominantly the lateral pterygoid on one side. If the patient is gently guided to centric relation and a hinge type movement encouraged, the deviation will be eliminated. Unguided deviations upon opening may be regarded as a possible sign of muscle dysfunction. Even if a patient has an asymmetric mandible, the midline will not significantly deviate, if the condyles are in the seated position prior to translation in the joint. About the only time the mandibular midline will deviate upon opening when both condyles are in centric relation is when one glenoid fossa is more superior than the other relative to the transpupillary axis. This can be demonstrated by bending a clothes hanger wire to approximate the shape of a mandible, either symmetrical or asymmetrical. The ends of the wire, which represent the condyles, may be placed on a horizontal line of a piece of graph paper and rotated without displacing the ends. It will be seen that the midline will not deviate from a vertical line, which is perpendicular to the line connecting both free ends of the wire (the axis of rotation). However, the mandibular midline will deviate from the same vertical line on the graph paper, if one end of the wire is raised or lowered, but the horizontal line no longer represents the axis of rotation of the condyles. The mandibular midline always remains on a perpendicular to the hinge axis of rotation of the condyles.
DR. BRANDT What effect does gnathological treatment have on drifting of teeth?
DR. WILLIAMSON Clinically, the stability seems to be very good. I believe this is due to the increased number of cusp-fossa occlusal contacts, along with lack of forces at an angle to the long axis of posterior teeth, when condylar movements are considered. Certainly, a properly gentle anterior guidance is required.
DR. BRANDT Does equilibration following orthodontic therapy have an effect on the stability of the treated dentition?
DR. WILLIAMSON There is no question in my mind. We do not have scientific documentation of this presently. However, the cases which I have equilibrated, and in which no retainers were used, have remained very stable. This statement does not mean to imply that I never use retainers. it is my observation that treating to a concept of a physiologically seated condylar position and providing proper posttreatment equilibration can eliminate retainers in many cases and minimize retainers in many others. Posttreatment equilibration is not a panacea for pretreatment misdiagnosis.
DR. BRANDT Should an orthodontist equilibrate during treatment?
DR. WILLIAMSON The orthodontist should not equilibrate during treatment, Sid. Posttreatment equilibration is ideal therapy in my opinion.
DR. BRANDT On every case?
DR. WILLIAMSON It is unreasonable to perform a proper equilibration on every case. You will remember that I said earlier in the interview that patients who display moderate pain to palpation in four of the eight muscles of mastication should be finished precisely. I think these cases should be equilibrated. All others should be finished close enough to centric relation that, should equilibration be required in the future, it can be completed with no problems.
DR. BRANDT At what point should equilibration be done?
DR. WILLIAMSON I will equilibrate the patient as soon as I think the maximum has been attained from a hinge axis positioner. Generally, a large amount of equilibration is not required.
This means that gross amounts of tooth structure are not removed to attain my goals.
DR. BRANDT Can occlusal adjustments be performed successfully without mounting the plaster casts on a fully adjustable articulator?
DR. WILLIAMSON Proper occlusal adjustments may be completed by using a semi-adjustable articulator. The main advantage of a fully adjustable articulator is the ability to program the immediate side shift (Bennett movement) and border movements of the patient. This allows the operator to make more accurate adjustments on the occlusal surface of the casts. It also allows him to better visualize where tripod contacts will be made on the occlusal surfaces. The fully adjustable articulator is a very sophisticated instrument, and requires a good deal of training and use for one to become proficient. Since we have found most adolescent patients to have a minor amount of side shift, it is my opinion that these subjects do not require fully adjustable instrumentation. The adult patient who is a true TMJ problem is a different case.
DR. BRANDT in order to attain maximum benefits from mounting the casts, is it necessary to locate the terminal hinge axis?
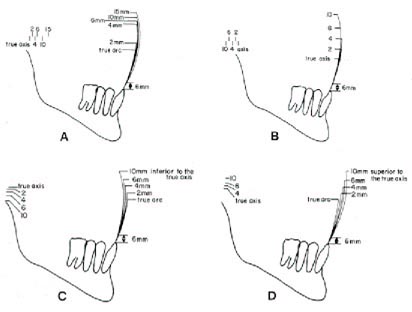
DR. WILLIAMSON The key word in that question is "maximum" I would have to say that, in order for maximum benefits to be attained, a terminal hinge axis recording and transfer is necessary. However, in most situations near-maximum benefits may be achieved with a properly done arbitrary facebow transfer, along with an accurate interocclusal record. In the process of teaching occlusion courses to orthodontists, using the fully adjustable instrument and determining the axis of rotation of the mandible, we did an interesting clinical study. The models of the subjects were mounted on the Stuart instrument by utilizing the hinge axis. A second set of models of the same subjects were mounted on a semi-adjustable articulator by means of a Whip-Mix quick mount, arbitrary facebow transfer. The same interocclusal record was used for both mandibular model mountings. The interocclusal record was made utilizing ZOE and an anterior guidance prosthesis, which is similar to a leaf gauge. It was made at a most closed vertical dimension, just prior to first tooth contact. When the models were mounted, the interocclusal records were removed and the articulators closed to first tooth contact.
In all cases the first contact was the same on the semi-adjustable articulator as it was for the same patient on the fully adjustable one. This indicated that the centric closures were extremely close, when using a hinge axis and comparing it to the arbitrary facebow, using the same interocclusal record for mounting the lower models. However, this investigation was done with asymptomatic patients. It did not mean that eccentric condylar recordings would be identical. The diagrams in Figure 17 indicate that if the arc of closure at the lower incisor does not exceed 6mm, the tolerances indicated are available for error in the arbitrary hinge axis compared to the true one. What it doesn't show are the errors at the occlusal surface in the buccolingual dimension. Slavicek has mathematical data indicating that, if the axis used differs from the true hinge axis by 4.2mm vertically and in combination with error of 4.2mm anteroposteriorly on the same side, the error at the occlusal surface can be .52mm buccolingually. This much error certainly is clinically significant. It becomes obvious that the critical dimension for hinge axis is vertical.
At this point, Sid, I think a word concerning the so-called hinge axis is in order. There is evidence that there may not be a single axis of rotation for the mandible prior to translation. However, it is the clinical result and application of the effect of the axis, or axes, at the skin surface, and the transfer of this result to the articulator, that is important. It is purely an academic question if one true axis exists or not. It's importance is magnified when there is a rotation of the mandibular casts from the point in space that the interocclusal record was made to the vertical dimension of occlusion. The less this rotation is, the less chance there is for error in the arc of closure. Therefore, the interocclusal record should be made at centric relation and maximally closed prior to first tooth contact. It must be kept in mind that the final measure of accuracy is the clinician's ability to transfer the results of his diagnostic mounting and equilibration to the patient's mouth. If tripod contacts for cusps cannot be duplicated in the patient's mouth by the clinician during equilibration, it is difficult to rationalize the time and effort spent with the fully adjustable instrument. On the other hand, if good occlusal anatomy exists in the mouth and the patient exhibits a substantial immediate side shift, it is difficult to rationalize not using the advantages available with such instrumentation. These factors become very important to the restorative dentist, who has the ability to wax occlusal surfaces and is seeking the utmost in accuracy.
DR. BRANDT What articulator would you recommend for an orthodontist who wishes to performgnathological treatment and occlusal adjustments?
DR. WILLIAMSON I believe that the average orthodontist needs only a semi-adjustable articulator. Three examples would be the Denar Mark II, the Whip-Mix, and the Panadent.
DR. BRANDT One must conclude from what you have said, that you believe that all practicing orthodontists should fully understand functional occlusion and be prepared to apply it routinely to their patients.
DR. WILLIAMSON It is my contention that the orthodontist is the primary oral reconstructionist. He is rebuilding mouths of children at age 12 with the goal of tooth retention and good function for the rest of their lifetime. With such a responsibility, he should know more than any other discipline in dentistry about functional occlusion. This also implies that he should be able to deliver the best functioning occlusion for each individual patient.
DR. BRANDT What courses should an orthodontist consider if he is interested in learning more about gnathological treatment?
DR. WILLIAMSON If an orthodontist is seeking training, an orthodontist should be the teacher. It should be a participation course, in which the student applies the clinical skills. Ideally, it should be a course in which the student becomes reeducated in biological principles, and is taught to apply them clinically. He may then bring cases and clinical examples to the next session for critique.
DR. BRANDT Thank you on behalf of our readers for this splendid, informative, and thought-provoking interview. We appreciate your time and effort, and willingness to share your knowledge and experience with us.