JCO Interviews Dr. Eugene H. Williamson on Occlusion and TMJ Dysfunction, Part 1
We are indeed fortunate to interview Dr. Eugene H. Williamson on this increasingly-important subject for orthodontists. Dr. Williamson has been Associate Professor and Chairman of Orthodontics and Associate Professor of Anatomy at the Medical College of Georgia, School of Dentistry. Prior to receiving his orthodontic education, he was in the private practice of restorative dentistry. He has taught numerous courses on occlusion to both restorative dentists and orthodontists. He has lectured internationally, and published research papers on mandibular condylar position in the finishing of orthodontic cases, and equilibration. Radiography of the temporomandibular joint has been an area of special interest to him.--SIDNEY BRANDT, DDS, Interviews Editor
DR. BRANDT Let's begin with definitions of some of the terms that are bound to come up in the course of this interview. Centric relation?
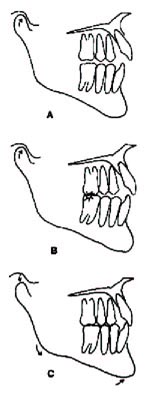
DR. WILLIAMSON In centric relation, both mandibular condyles are simultaneously seated more superiorly on the posterior slope of the articular eminences, with the menisci interposed properly between. They are placed in that position by the patient's own healthy closing musculature, which is contracting evenly on both sides. It is referred to as CR, and is prior to first tooth contact (Fig. 1A).
DR. BRANDT Centric relation occlusion?
DR. WILLIAMSON That is centric relation at first tooth contact. It is referred to as CRO or retruded contact position (RCP) (Fig. 1B).
DR. BRANDT Centric occlusion?
DR. WILLIAMSON Centric occlusion is that position of the mandibular condyles when the teeth are in maximum intercuspation. It is referred to as CO or intercuspal position (IP) (Fig. 1C). In most nontreated cases, CRO and CO will differ.
DR. BRANDT Terminal hinge axis?
DR. WILLIAMSON The axis, or the result of axes of rotation, around which the mandible rotates when opening or closing with the condyles at CR.
DR. BRANDT Anterior guidance?
DR. WILLIAMSON Anterior guidance is the direction of any mandibular movement dictated by the maxillary and mandibular canines and incisors. Posterior guidance is dictated by condyles and fossae. Anterior guidance should function easily and smoothly, displaying minimal fremitus of teeth with maximum muscular activity, which propels the mandibular condyles through their total area of movement. The premolars and molars must function within this envelope of motion without dictating guidance.
DR. BRANDT Prematurity?
DR. WILLIAMSON The first tooth contact which is made as the mandible closes with the condyles in CR. Usually, this is prior to maximum intercuspation.
DR. BRANDT Deflection?
DR. WILLIAMSON Deflection is a movement of the mandible from the prematurity to maximumintercuspation. This movement displaces the condyles from the CR position.
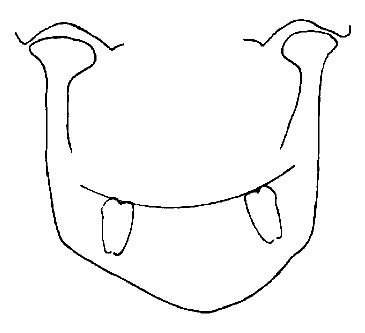
DR. BRANDT Mandibular asymmetry?
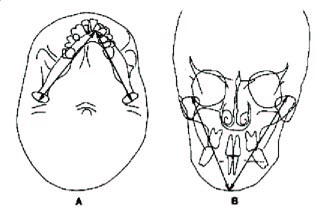
DR. WILLIAMSON This is a difference between the size or shape of the two halves of the mandible. This may occur in the frontal or horizontal (basilar) planes, or both, and be reflected in the sagittal plane (Fig. 2).
DR. BRANDT Physiologic condylar position?
DR. WILLIAMSON This is the position of one or both condyles--either static or dynamic--at any moment in time, in the absence of deflective prematurities. This position is dictated by neuromusculature, ligaments, bone, and fibrous connective tissue.
DR. BRANDT Laminagraphy?
DR. WILLIAMSON Laminagraphy is a method in which the x-ray tube head and film move in opposite directions during exposure in such a way that the radiographic shadow of a selected plane within a body remains stationary. Shadows of all other planes have a relative displacement and are blurred in varying amounts. The degree of blurring depends upon the distance of the planes from the one in focus. It is therefore possible to eliminate superimposed shadows of overlying structures and circumvent the problems of dense bone.
DR. BRANDT Gnathology?
DR. WILLIAMSON Gnathology is the study of the jaws or gnathic system. The word has taken on the connotation of implying a specific condylar position, which in the past was thought to be unchangeable--one axis of rotation for the mandible on closing and opening when the condyles are at CR; tripod contacts of centric holding cusps in fossae when placing restorations; light contact of the anterior teeth in CRO; CRO and CO coincident; and the canines and incisors separating all posterior teeth on any eccentric movement of the mandible. The clinical connotation of the term originated on the West Coast and emanated from a dedicated study group, which developed sophisticated mechanical devices that traced the functional movement of the mandible. These movements could then be transferred to an articulator, which was "fully adjustable" and could be set to duplicate human jaw movements. In this manner, the group could study occlusal patterns or schemes, which functioned best within these jaw movements; and they restored patients' mouths utilizing these concepts. Some of the most excellent dentistry in the world has resulted from their endeavors. Since these procedures required a substantial amount of hardware, the concept of the group became labeled as mechanistic and "too articulator conscious" by those who deemed themselves true biologists. There then developed a split between groups and misunderstandings resulted. The point that was missed is that the articulator simply echoed the effects of the biological determinants of jaw movement, i.e., the four basic biological tissues--nerve, muscle, epithelium, and connective tissue. The fully adjustable articulator was, and is, a means through which the effect of these determinants can be studied and programmed onto the enamel tooth surfaces or restorations.
DR. BRANDT Gene, as an orthodontist and a gnathologist, how do you examine a new patient? What records do you take? What do you look for clinically?
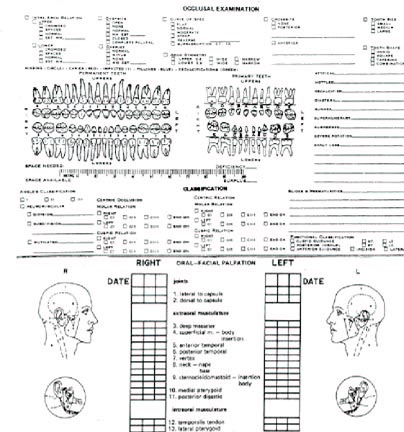
DR. WILLIAMSON When the patient is first seen at the chair, a health history has been completed (Fig. 3). Clinically, the main indications of incipient dysfunction seen at the screening are joint noises and pain on palpation in the muscles of mastication. In adolescents, clicking will be observed much more often than crepitus or grating. Crepitus may indicate the possibility of true joint pathology or degenerative processes. Clicking or popping can indicate congenital anomalies in the meniscus or incoordination between the condyle and meniscus on movement. More frequently seen than joint noise, however, is pain in the muscles of adolescent patients on palpation.
DR. BRANDT Please describe how you perform the muscle examination.
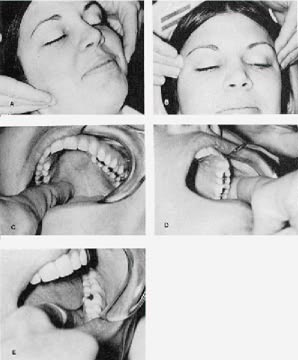
DR. WILLIAMSON The procedure I use for muscle examination is as follows. The patient is told, "I am going to press on some muscles around your face and jaws. Tell me if you feel pain while I am doing this. Differentiate between any pressure you feel and pain. (Press on the patient's shoulder to indicate how pressure feels.) If you feel pain, is it mild, moderate, or severe? Mild is defined as 'it hurts a little bit' Moderate is 'I wish he'd take his fingers away' Severe is 'ouch"' With severe pain, the patient will usually flinch. On the screening form, mild is designated 1, moderate 2, and severe 3. The palpation is done bilaterally and simultaneously for the masseter and temporalis. The lateral and medial pterygoids are done unilaterally and intraorally (Fig. 4). Substantial pressure is utilized. If a patient shows moderate or greater pain in four of the eight muscles, his chart needs to be identified. That case will need special attention throughout treatment, and care in retaining.
DR. BRANDT When palpating a patient who is in pain, should this be performed right over the TMJ?
DR. WILLIAMSON Yes, gently.
DR. BRANDT If the soreness seems to be right at the TMJ, would that indicate that the problem is right in the joint?
DR. WILLIAMSON Correct, at least according to most experts. It seems to indicate the possibility of intrajoint pathology, edema, etc.
DR. BRANDT If the pain is located below the TMJ, would that indicate a muscular complication?
DR. WILLIAMSON Most probably, in the masseter muscle.
DR. BRANDT Does the examination differ if the patient's chief complaint is "clicking"?
DR. WILLIAMSON No, Sid. Usually when clicking is present, the patient will have pain on palpation, generally in the pterygoid complex.
DR. BRANDT What other diagnostic records do you take?
DR. WILLIAMSON Following the clinical exam, routine intraoral and extraoral photographs are taken. Radiographs include the lateral cephalogram made at maximum intercuspation, frontal made at CR, submental vertex made at CR, panoramic, periapicals where deemed necessary, and bite wings.
DR. BRANDT You do not take the lateral cephalogram in CR?
DR. WILLIAMSON The lateral cephalogram is made at maximum intercuspation, since we found that the differences between films made at centric occlusion and those made as centric relation at the vertical dimension of maximum intercuspation were not statistically significant. However, this statement must be qualified, since we did see individual cases in the second standard deviation in which the differences were very significant. These are the cases needing special attention. Often, when assessing centric relation on them clinically, it may be necessary to mount the models on an articulator for diagnosis.
DR. BRANDT But the frontal and submental x-rays are taken in CR.
DR. WILLIAMSON The frontal and submental vertex x-rays are made in centric relation, in order to look for mandibular asymmetry. Since the goal is to finish the case at centric-relation, diagnosis utilizing that position is necessary. The seated condylar position frequently makes a difference in assessing skeletal disharmony.
DR. BRANDT Is there a cephalometric technique to help determine centric relation?
DR. WILLIAMSON I don't believe you can determine centric relation by looking at a radiograph. In studies with laminagrams, lateral cephalograms, and transcranial x-rays, the range of biological variation in joint space is great. However, if a cephalogram with the mandible in centric relation prior to first tooth contact is desired, it is taken with a leaf gauge in. In cases of surgical maxillary impaction, where a prediction tracing is needed with rotation of the mandible to close the vertical, I use this type of lateral cephalogram.
DR. BRANDT But the usual lateral cephalogram tracing at maximum intercuspation is not a true representation of centric relation.
DR. WILLIAMSON It is by no means a true representation of centric relation, although it might be close in some cases. When the lateral cephalogram is assessed, we are looking at a tooth-guided position of the mandible. It is not a true skeletal relationship of the mandible to the maxilla and cranium. We must consider the seated condylar position by means other than the lateral head x-ray, and adjust our treatment plan accordingly. Generally, and particularly in Class II cases, we are treating a more difficult case than appears from the cephalometric numbers. That is why we must have a concept of where the physiologic functional condylar position should be. A great deal of my research has been aimed at trying to answer that question.
DR. BRANDT What type of x-rays are required to get a truer picture of centric relation?
DR. WILLIAMSON By far the best x-rays available are laminagrams or polytomes.
DR. BRANDT Do most orthodontists have sufficient training to analyze the TMJ and make critical judgments and treatment recommendations about it?
DR. WILLIAMSON I am sorry to say "no", most orthodontists do not. It is my opinion that this is the fault of the training institutions. There is very little emphasis on dysfunction. However, in fairness to the institutions, a two-year training program is minimum time, at best, for the student to learn the basics of routine orthodontic diagnosis and treatment planning.
DR. BRANDT Are those clinicians who perform this type of service to be considered a subspecialty of orthodontics?
DR. WILLIAMSON I think that is a good description.
DR. BRANDT Can an orthodontist who is depending upon the usual lateral cephalogram tracing be misled into thinking there had been mandibular growth, when there actually had not?
DR. WILLIAMSON Yes. I'm sure most clinicians have seen a case where the progress tracing superimposed on the original actually shows a decrease in mandibular growth. It can usually be explained by realizing that the patient was reaching forward to attain maximum intercuspation on the original cephalogram. With treatment, the mandible may begin to migrate toward centric relation, since a comfortable maximum intercuspation position is removed via tooth movement. It, therefore, appears that the mandible has actually shortened with treatment.
DR. BRANDT How do you go about finding CR at the initial examination?
DR. WILLIAMSON Establishing a mandibular position close to centric relation can be accomplished quickly by having the patient attempt to close on the posterior teeth, while having a leaf gauge between the maxillary and mandibular incisors (Fig. 5). A leaf gauge is similar to a spark plug gauge, with individual leaves that can easily be added or taken away. My gauges are made from exposed radiographs, which have been through the developer. After removal of emulsion and processing solution, these are cut into 1cm by 5cm strips and fastened by a staple or link chain through a hole in one end. A sufficient number of leaves are placed between the patient's incisors, and he is asked to try to bite the back teeth together evenly on both sides at the same time. If he can contact teeth, another leaf is added. The process is repeated until the patient can bite for five minutes without contacting any teeth. At this time, the gauge is removed and the patient closes to first tooth contact, with the condyles seated in centric relation. The difference between CO and CR is now assessed. if the difference is 3mm or more, the models are mounted on a semi-adjustable articulator. If the difference is less than 3mm, I take a wax record for grinding the models at CRO.
DR. BRANDT How is that accomplished?
DR. WILLIAMSON This is done by having the patient close to CRO and asking him if he can feel where the first contact is. When he tells me he feels it, he is asked to point to it. He is then told that a piece of wax will be placed between his teeth and he should close through it until tooth contact is made. During this procedure, an operator-guided technique is used, whereby I place the index and second finger of my right hand on the gonial angles and press lightly upward. The thumb is on pogonion, pressing lightly downward. When the models are ground to this record, they can be laid on their backs and be close to centric relation. There is no stability mediolaterally, but it gives me a quick reference during treatment.
DR. BRANDT Does the examination procedure change for different types of malocclusion?
DR. WILLIAMSON Yes, Sid, it does. The major difference occurs with the Class II's. It was found in the Centric Ceph study that the Class II's show the greatest deviation between CRO and CO. Therefore, I assess them carefully. When a pretreatment diagnostic articulator mounting is needed, it is generally a Class II case. In our study, the range of deflection for 28 Class II cases was up to 4mm with a mean of 2.5mm horizontally (anteroposteriorly). Vertically, the difference in condylar position between CRO and CO was as much as 5mm (more superiorly at CRO). The mean was 1.37mm. The Class I cases showed a range of 0mm to 2.5mm anteroposteriorly. The mean was 1.5mm. The condyles of the Class I cases seated up to 2.5mm more superiorly at CRO, with a mean of 1mm. Therefore, I seldom see an adolescent Class I which requires pretreatment mounting. It should be kept in mind that we are referring to the routine adolescent patient so far, not the adult.
DR. BRANDT Tell us about your electromyographic studies in this regard.
DR. WILLIAMSON I have found, utilizing electromyography, that if the masseter and temporalis are monitored on the working side, and a patient has a cuspid disclusion on that same side, when he is closed at centric occlusion, both the temporalis and masseter are very active. As soon as the patient moves eccentrically in a working motion, the masseter immediately stops being active. If we take the same patient and introduce a small piece of gauze between the premolars, or any teeth distal to the canines, and have the patient repeat the working excursion so that we have developed a group function, the masseter continues to be extremely active throughout the working movement (Fig. 6). If the same muscles are monitored, but the patient begins a working excursion on the opposite side (making the side we are monitoring the non-working or balancing side), when the mandible leaves centric occlusion and there are no balancing contacts distal to the canines, the temporalis and masseter on the balancing side immediately become quiescent (Fig. 6). If a balancing contact is introduced with a small piece of gauze, continued heavy activity of the temporalis and masseter is observed throughout the excursion (Fig. 6). These observations indicate that, with posterior tooth contact in any eccentric movement of the mandible, the pterygomasseteric musculature is very active, and placing forces on the posterior teeth which are at angles to the long axis of the teeth. If there are no posterior tooth contacts in eccentric mandibular movements, the temporalis and the masseter are quiet on the balancing side, while the temporalis (a positioning muscle with relatively light force) is the only one active on the working side. Therefore, with proper anterior guidance, the front teeth accept a relatively small load from the musculature when the back teeth are not functioning.
I have also observed that, when using the leaf gauge between incisors to register CR, the muscles contracting and seating the condyles when the posterior teeth are not contacting are the temporalis and the superior head of the lateral pterygoid (Fig. 7). As soon as the patient rotates the mandible closed to first tooth contact with the condyles still at centric relation, the masseter begins to be active.
DR. BRANDT What are the clinical implications of all that?
DR. WILLIAMSON Sid, what this means to me at the clinical level, is that I want a case finished with the condyles as close to centric relation as I can treat them, preferably CRO = CO, with as many cusps in fossae as possible, for stability. The cuspids and incisors should disclude all posteriors in any eccentric mandibular movement, with as little fremitus to the anterior teeth as possible, when maximum muscle force is utilized for eccentric movements.
DR. BRANDT How many orthodontic cases are finished to those criteria?
DR. WILLIAMSON The majority of orthodontic cases are not finished to those guidelines. In my opinion, the static Angle Class I is but one criterion, albeit an important one. It is very possible to finish a case in acceptable Angle Class I and still have deflections present when the patient is examined in function. For example, Andrews speaks of the distal incline of the distobuccal cusp of the maxillary first molar contacting the mesial incline of the mesiobuccal cusp of the mandibular second molar in the ideal Class I static occlusion. If the distobuccal cusp of the maxillary molar is not carefully checked in function, this relationship may lead to a working side deflection as the mandible leaves centric or returns to it. One may also frequently demonstrate a centric discrepancy by placing the patient on a leaf gauge for a few minutes and then checking the occlusion. When the condyles are seated, a totally different classification of the occlusion may be apparent.
DR. BRANDT What, in your opinion, are the consequences of not approaching or achieving CRO?
DR. WILLIAMSON It is my feeling that, if a deflective malocclusion is disregarded in treatment, the patient may be left with a potential for dysfunction and periodontal problems that might otherwise have been attenuated.
DR. BRANDT Is deflective occlusion a main cause of TMJ dysfunction?
DR. WILLIAMSON When examining patients with dysfunction there are two variables which always seem to be present. One variable is the abnormal emotional status of the patient, the other is the presence of prematurities or deflective tooth contacts. Substantial evidence is accumulating, indicating that the occlusal scheme is related to muscle function. You will note I did not say a cause and effect relationship. When treatment of a case is begun, a totally new occlusal scheme is being established. The mouth is being reconstructed, as well as the face of the patient. If the occlusal scheme is related to muscle function, it is my goal to provide the one which allows the best chance of health to muscle and teeth. The ultimate objective, since I am first a dentist, is to preserve the dentition and jaws in a healthy state for the rest of my patient's lifetime, with the least amount of treatment. Since the concepts listed so far seem to have some documentation from a biological point of view, they seem a valid goal for treatment. In treating to those goals I am removing the one variable over which we have control; that is, the deflective malocclusion. I believe in total patient care, but realize the patient will never be able to be shielded from the other variable present, which is the emotional stress of life.
DR. BRANDT Is it possible that habits cause deflections to occur?
DR. WILLIAMSON Yes, Sid, it is possible for habits such as thumb sucking to cause deflections, since tooth and jaw positions are influenced by it.
DR. BRANDT Could we say, on the other hand, that deflection causes bruxism?
DR. WILLIAMSON Bruxism might better be thought of as a result of the emotional factor, with the coincidental presence of a deflection. In other words, it makes a convenient spot on which the patient may grind and for muscles to get sensitive. EMG studies of bruxist patients before and after repositioning splints, and in comparison to controls, indicate a statistically significant decrease in muscle activity when occlusions are developed for the bruxer which discourage tooth grinding. These splints follow the concepts of centric relation and anterior disclusion of posterior teeth. This is one of the reasons that my goal in treatment is the removal of the one variable which can be controlled by way of treating the functional occlusion.
DR. BRANDT How do you rate tongue thrust in this picture?
DR. WILLIAMSON Tongue thrusting is another problem. I totally agree with Proffit, and the indications from his research. He advocates the resting position of the tongue to be the important factor, not the instantaneous thrust of the tongue. It may well be that the tongue is resting in a particular position to prevent the discomfort of a deflection from occurring. I have a number of clinical cases in which mild open bites, both anterior and posterior, have been corrected by occlusal equilibration. No retaining appliances have been used, and they are stable (holding .0005" shimstock) as long as five years posttreatment (Fig. 8). These are not skeletal open bites.
DR. BRANDT Once deflections are present, what are some of the symptoms?
DR. WILLIAMSON Symptoms may include wear on the occlusal surfaces of the teeth, pain on muscle palpation, joint noises, and frequent headaches.
DR. BRANDT Is the onset of these symptoms gradual--so perhaps the problem can be diagnosed and treatment initiated before the pain becomes too intense?
DR. WILLIAMSON The onset of the symptoms depends upon the emotional status of the patient. The more stress the patient takes out on his teeth, the sooner the symptoms will appear. As an example, I recently saw a fourteen-year old male who had worn one-half of the anatomical crowns from his permanent canines bilaterally. Now, Sid, you know how long those canines had been in this patient's mouth. Not more than a couple of years, correct? It so happened that this boy was a superachiever from a superachieving family. It has been shown by Roth, and I will verify his findings with my own, that every time a cuspid tip is worn, there is a balancing deflective contact in the area of the opposite second molar. When these cases are mounted on a fully adjustable articulator and studied, it appears that the-patient is bruxing on the balancing deflection, and, with the high velocity of mandibular motion which Hannam and others describe, slides off that contact and shears into the canines on the opposite side. In other words, he is not bruxing on the canines themselves. However, the effect on them is the result of bruxing on the second molars.
DR. BRANDT Should the clinician be on the alert for any rare or unusual conditions?
DR. WILLIAMSON Absolutely. A differential diagnosis must be made to rule out the rare pathologies. The repositioning splint helps to do this, along with the initial examination.
DR. BRANDT What percentage of orthodontic patients have incipient levels of dysfunction prior to treatment?
DR. WILLIAMSON In an attempt to answer that question, I did a survey of 304 patients who presented for screening in the orthodontic clinic. Thirty five percent displayed incipient signs or symptoms of dysfunction prior to orthodontic therapy.
DR. BRANDT How do you determine which of these is heading for some more serious dysfunction?
DR. WILLIAMSON It is very difficult to predict which ones with incipient symptoms will some day become overt. This is why we must record those at the examination appointment and be careful in treatment to finish them with the best functional occlusion possible. The goal for that functional occlusion must be based upon the best research available. We are back to a concept of the ideal functional occlusion. From a scientific point of view the best method currently available to predict muscle dysfunction is the silent period. The silent period can be seen on a special electromyographic readout and measured in milliseconds. It is done by monitoring the masseter muscle with surface electrodes and having the patient bite in centric occlusion while a tap is made on the chin. Apparently, the muscle spindles and the periodontal receptors combine to stop the contraction of the mandibular closing muscles. This is regarded as a protective mechanism to muscle and teeth, and can be seen on the EMG as an absence of muscle activity. Hence, the name, silent period (Fig. 9). Researchers have found a positive correlation between the amount of overt dysfunction present and the length of the masseteric silent period.
DR. BRANDT Suppose the orthodontist misses the deflection?
DR. WILLIAMSON A potential problem exists indefinitely. It becomes a matter of adaptability. When the patient can accommodate to the deflection, he may get along with incipient symptoms only. My concern is being able to predict which ones will adapt and which ones may not, when placed under enough emotional stress.
DR. BRANDT If a deep anterior bite deepens again following correction and retention, what is the effect of that?
DR. WILLIAMSON Overeruption of the anterior teeth may cause a patient to be overcoupled or locked in with too much anterior guidance. This limits condylar freedom, and can be as much of a problem as no anterior guidance at all. In order for the patient to make eccentric movements, he must first open the mandible. Electromyographically, it has been demonstrated that the inferior head of the lateral pterygoid is first to contract on opening. It also seems to be the muscle complex most sensitive to palpation in these dysfunctional people.
DR. BRANDT What should be done in these cases?
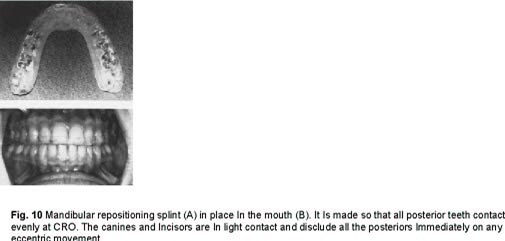
DR. WILLIAMSON If the patient is not displaying symptoms of dysfunction, and they are not particularly displeased with esthetics or the degree of relapse, possibly nothing should be done. If they are developing dysfunctional symptoms, a mandibular repositioning splint should be made on the maxillary arch (Fig. 10). Once the symptoms have been alleviated with splint therapy, a diagnostic mounting should be made on a semi-adjustable articulator. Assessment of the case should then be done, and treatment should follow the least invasive technique. These would be (1) equilibration, (2) orthodontics, (3) restorative dentistry, (4) oral surgery, and (5) a combination.
DR. BRANDT Let's reverse the malocclusion. What about a recurring open bite?
DR. WILLIAMSON The reestablishment of an open bite is one of the most perplexing problems to the orthodontist. The degree to which it relapses and whether it is anterior or posterior are important questions.
DR. BRANDT Let's assume we are talking about an anterior open bite.
DR. WILLIAMSON Generally speaking, if the patient is examined at centric relation occlusion, the open bite will be more severe than at centric occlusion. It all results in a lack of anterior guidance out in front of the pterygomaxillary sling of musculature. As was pointed out earlier, when posterior teeth are allowed to contact eccentrically, it opens the door for bruxing within that heavy musculature. We then begin to see symptoms of dysfunction developing, along with wear of the posterior teeth. The one situation that becomes extremely difficult to handle is idiopathic condylar degeneration. When this occurs, the open bite continues to get worse.
DR. BRANDT What should be done?
DR. WILLIAMSON The diagnostic procedure with recurrent open bite would be similar to those for recurrent deep bite. Repositioning splint therapy is of utmost importance in these cases. If condylar degeneration does happen to be the problem, it is important to see stabilization on the splint, with no change of the occlusion for a period of 4-6 months, prior to establishing a definite treatment plan. After this period of time, we may consider the process to be in a state of remission, at least temporarily. It would be a shame to treat such a case a second time, and then see it relapse again, due to continued degeneration.
DR. BRANDT Could many of these problems have been avoided if the case had been analyzed with an occlusal study prior to band removal to determine both the static and functional occlusion?
DR. WILLIAMSON A great many, Sid. It would be even better if certain cases were mounted and analyzed prior to any treatment. This will frequently change a treatment plan. It is not unusual for a patient to be a typical Class II when his models and headplates are examined. However, when his articulated casts are observed, they demonstrate even more severity. In such a situation, it may be prudent to suggest the possibility of future surgery to the parents, particularly if growth is not favorable. Mounting models toward the end of treatment is extremely enlightening. You certainly are able to diagnose detailing and to assess maxillomandibular discrepancies. It is a common practice, especially in difficult cases requiring more attention.
DR. BRANDT Does it need much of a prematurity to create occlusal problems?
DR. WILLIAMSON No. Some individuals are much more sensitive to minor discrepancies than others.
DR. BRANDT Is there a quick method of determining the presence of prematurities?
DR. WILLIAMSON There are a number of quick methods. One way which works particularly well is the use of the leaf gauge and the .0005" shimstock material. Just a few minutes of leaf gauge therapy will reveal a great deal (Fig. 11).
DR. BRANDT If an orthodontist does find a cusp striking prematurely while the appliances are in place, should that cusp be ground down, or would it be preferable to torque or move the tooth to eliminate that cusp prematurity?
DR. WILLIAMSON I am very much opposed to indiscriminate grinding on teeth, Sid. If the orthodontist finds deflective malocclusion present, he should be able to do the majority of correction with the appliances. This is one reason the pretorqued and tipped brackets are an advantage in treating to good functional occlusion goals. When they are properly placed they can circumvent some of the more common problems.
DR. BRANDT Many clinicians depend upon "settling" after appliance removal to establish their completion goals. Is this a practical idea?
DR. WILLIAMSON No Sid, not in my opinion. All the practitioner has to do to disprove that hypothesis is to mount a few cases properly. Generally, he will find not only centric prematurities, but balancing and working as well. I say mount them on an articulator, because just looking in the mouth may not be adequate to observe them. One of my goals in treatment is to finish with as many cusps in fossae as possible. When cases are allowed to "settle in" the maxillary lingual cusps frequently will not seat into the mandibular fossae, particularly in the premolar region. This phenomenon can't be observed just by looking in the mouth. Under these circumstances, we have more of a potential for relapse, and cases must be retained longer.
DR. BRANDT Not infrequently, when orthodontic therapy has been completed, the maxillary lingual cusps are too long, or the molars are contacting only along their buccal edges. Are these conditions fraught with danger?
DR. WILLIAMSON No question about it. When maxillary first and second molar lingual cusps are hanging too far occlusally, it is an open invitation for balancing contacts to occur. When maxillary buccal cusps are left too far occlusally, the opportunity for working deflections to occur becomes great. In the process of teaching occlusion courses, I include waxing exercises. We have found through experience that the best functioning position for the maxillary molar lingual cusps is approximately one millimeter longer than the buccal cusps, when you sight straight across the occlusal plane. This provides the curve of Wilson with a proper radius (Fig. 12). A goal for treatment is therefore established, which may be assessed at each appointment.
DR. BRANDT Another popular aid to "sock in" the occlusion is the positioner. How reliable is this appliance to eliminate occlusal interferences?
DR. WILLIAMSON The positioner made from properly mounted models can help a great deal, Sid. However, it is not the panacea some people would like it to be. In remounting cases after the hinge axis positioner has been used, and comparing the amount of deflection before and after, we still see some discrepancy. This tells me that the majority of the correction must be completed with the fixed appliances. Nothing seems to take the place of the astute clinician's treatment.
DR. BRANDT Is there any danger that the positioner itself can create deflections and/or prematurities?
DR. WILLIAMSON An improperly constructed positioner may cause more problems than it solves. If the positioner is constructed so that a large discrepancy exists between the arc of mandibular closure that is required for the patient to close into it, and the arc which the patient truly has, an accommodation must be made by the patient when he bites into the positioner. Under these conditions, the positioner creates a deflection, since the patient's condyles must leave the seated position in order to bite into the dictated position. The teeth are positioned to that bite. When the positioner is removed, and the patient closes with a leaf gauge between the anterior teeth, his muscles seat the condyles superiorly. If he then closes with the condyles in centric relation, he makes a tooth contact prematurely to maximum intercuspation. A deflection now exists upon which the patient may brux.
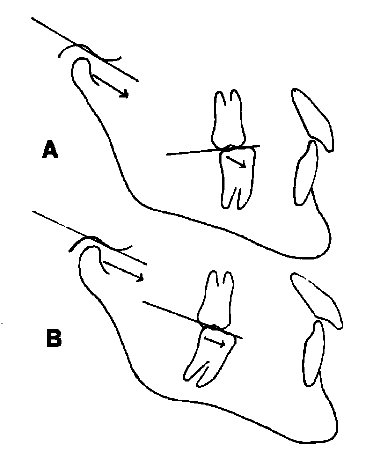
DR. BRANDT Many mandibular second molars have hypererupted distal marginal ridges at the beginning of treatment. Would correction of their axial inclination along with some intrusion be an advisable procedure?
DR. WILLIAMSON Absolutely, Sid. If the distal marginal ridge is too high, or left high after treatment, the occlusal plane for that individual tooth more closely parallels the protrusive and mediotrusive path which the condyles follow. When this occurs, the condyles lose their potential to separate the maxillary and mandibular teeth. Eccentric posterior contacts are therefore available (Fig. 13). We all know that intrusion is, therefore, advisable, but difficult to achieve with posterior teeth.
(TO BE CONTINUED)