JCO Interviews the Kesling & Rocker Group on Begg Technique, Part 2
HGB Do you treat high angle cases differently?
PCK To the untrained eye, all cases treated with the Begg Technique are treated essentially the same. All patients have archwires with anchor bends, and Class II or Class III elastics. The differences, however, are the amounts of anchor bend placed in the archwires, and to some extent, the strength of the intermaxillary elastics. The appliances used to treat high angle open bite cases are essentially the same as those used in low angle cases. Arch length/tooth mass discrepancies determine the need for reduction in tooth mass. Usually the first premolars are removed. Archwires are placed with very slight anchor bends, so that the depressing forces on the upper and lower anterior teeth are very light--perhaps only ten to twenty grams. Therefore, the wearing of two and one-half ounce (seventy gram) intermaxillary elastics on each side will overcome the light depressing force, to create a net elongation effect on the anterior teeth. Quite often this force system alone, plus the teeth becoming more upright (if they have been inclined labially from a tongue thrust), causes an open bite to begin to close. If after two appointments (approximately three months), there has not been a reduction in an open bite, we would apply anterior vertical elastics. Preferably, these elastics are engaged on the lingual surfaces of the anterior teeth, to help discourage the tongue from thrusting between the teeth.
In treating a deep bite case (Class I or Class II), the mechanics would be the same as for a high angle case--.016" archwires with anchor bends mesial to the molars, and Class II elastics. The difference would be, of course, that the bite opening bends would be much greater, causing the anterior portions of the archwires to exert between one and one-half ounces (42 grams) and two ounces (56 grams) of depressive force on the anterior teeth. This amount of force surpasses the anterior vertical component of force of the Class II elastics, causing the bite to open.
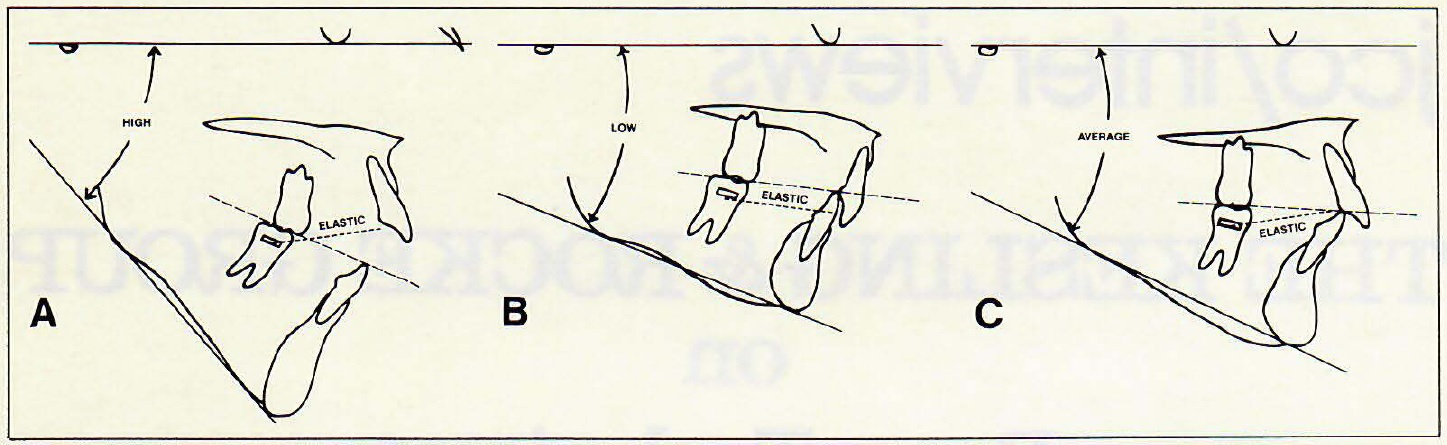
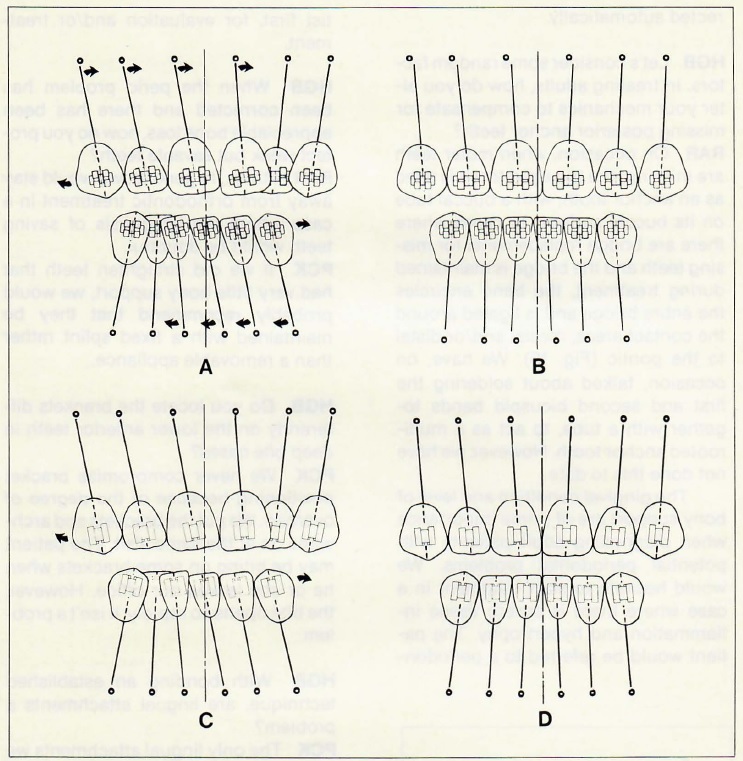
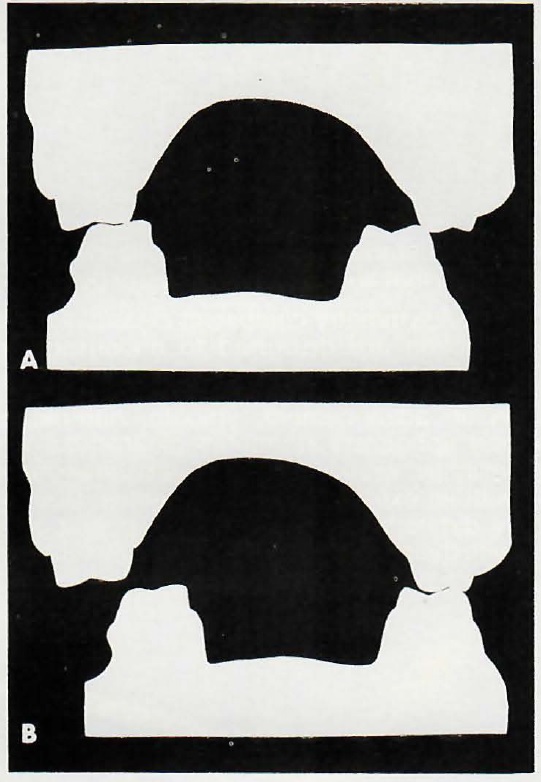
The changing "angle of attack" between intermaxillary elastic and the upper anterior teeth is also capitalized on in the Begg Technique to help produce the desired vertical changes. Open bites and high FMA angles go together. The "angle of attack" of the Class II elastics is high (Fig. 10A), resulting in an increase in the vertical elastic force component. This, coupled with reduced anchor bends, permits the open bites to close. Deep bite cases generally have low FMA angles. The "angle of attack" between elastic and anterior teeth, will therefore also be low--sometimes nearly parallel to the occlusal plane (Fig. 10B). This can result in almost no vertical component of force on the anterior teeth. Therefore, the nearly two ounces (56 grams) of depressive force that can be applied to the upper anterior teeth by the steep bite-opening bends in the archwire (hard ESP .016" Australian wire) is virtually unopposed. The deep anterior bites open quickly and consistently, as if by magic.
Between these two extremes lie the "average" cases, requiring moderate changes in the anterior overbite (Fig. 10C). In these cases, it is even easier to achieve the proper relationship between elastic and archwire forces, to open or close the anterior bites as desired. This, of course, is why the Begg Technique, when practiced properly, does not create "gummy smiles".
HGB Does the skeletal pattern affect your treatment plan with regard to extraction versus nonextraction?
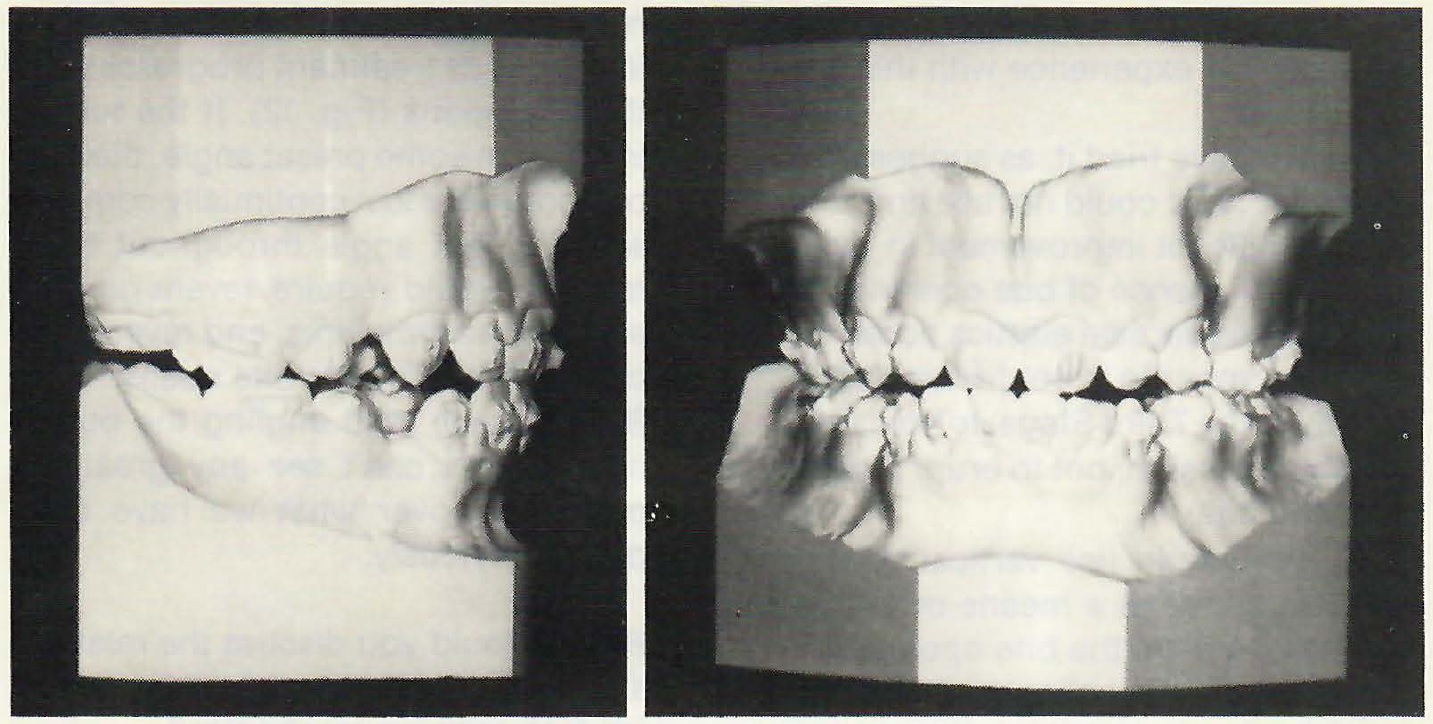
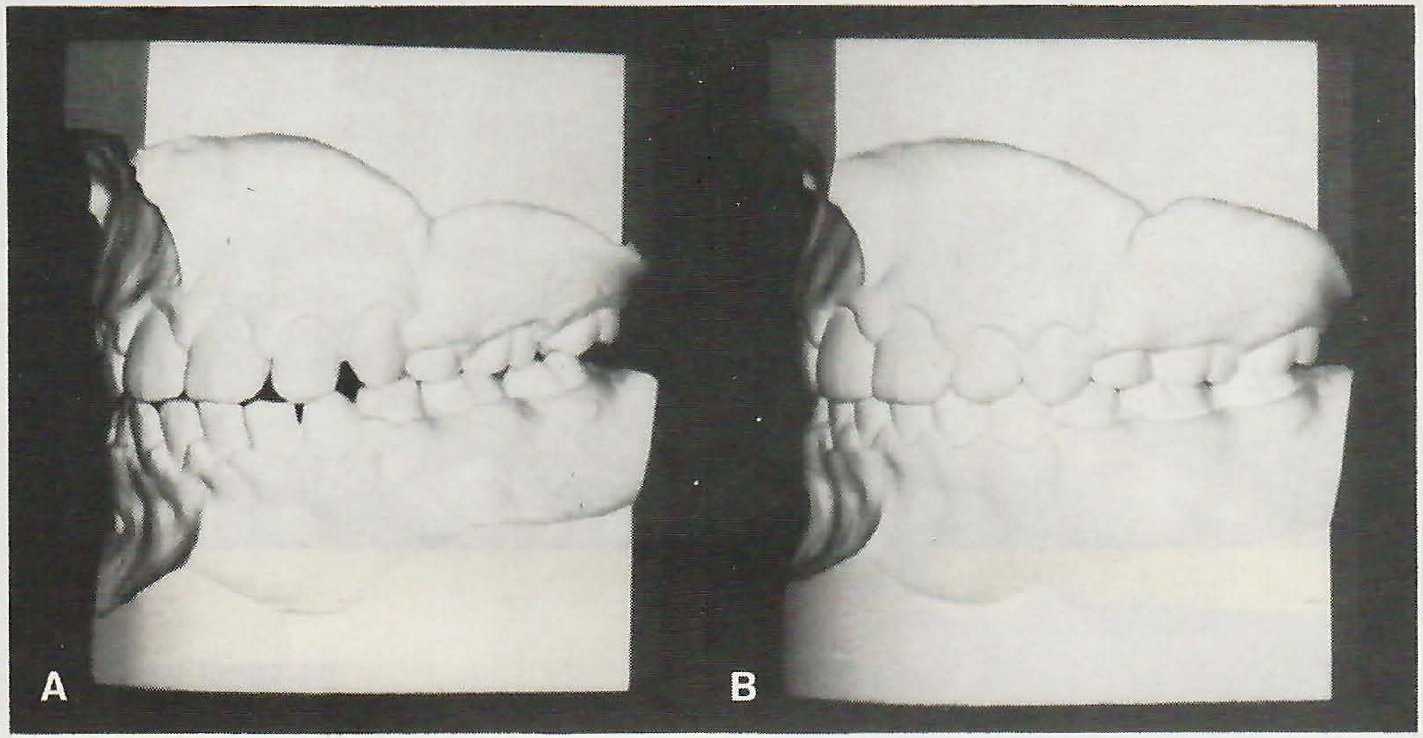
RAR Certainly in low angle cases, the tendency would be toward nonextraction. However, if there is extreme crowding, we would not hesitate to extract teeth. I think the final judgment would have to be made with the facial profile in mind. In high angle cases, we feel there is more tendency toward extraction. However, the treatment plan would then proceed the same as low angle cases. This is one of the unusual things about Begg treatment. At the end of Stage I practically all cases look alike--anterior teeth edge-to-edge, rotations except for molars overcorrected, anterior spaces closed, and an overcorrected Class I molar relationship (Fig. 11).
HGB Gentlemen, I would like to pursue the question of vertical control a little more specifically. Some very excellent papers have been written on this subject, not the least of which have been by Ten Hoeve and Mulie. How do you respond to their findings?
PCK I would say articles such as this have been beneficial to orthodontics in a general way. They have renewed an interest in, and appreciation for, the extreme importance of bite opening, which I believe is necessary for treatment to progress properly in any orthodontic technique. However, these articles haven't changed our mechanics for bite opening. We still rely completely upon our hard .016" ESP Australian archwires, modified to open the bite in conjunction with light Class II elastics. It has worked successfully for us on every patient for over twenty years, and we just can't see any justification to consider changing our mechanics, based upon these reports. To date no one using extraoral forces, to our knowledge, has shown finished results that are consistently of a higher quality, or even equal to those we have been able to obtain with the completely intraoral technique as developed by Dr. Begg.
RAR When Pete talks about "hard wire", he is talking about ESP wire, which is the hardest wire drawn by A.J. Wilcock of Australia. It should be used right at the start of treatment in the first archwires, and carried through until .020" wires are placed in the Second or Third Stage. Relative to this bite opening, we have checked our records at the Center, and have found the average time to reach an edge-to-edge anterior bite is six months. Since we have eliminated the use of anterior vertical loops in 90% of our cases, the average time is even less. Of course, this also depends on good patient cooperation, which requires conscious effort on the part of the orthodontist.
PCK Variations in established techniques should not be suggested until it can be shown that either the results are superior to conventional methods, or the procedures reduce treatment time and/or patient inconvenience.
HGB Another method for increasing bite opening potential has been to use vertical elastics on anchor molars. What is your experience with this procedure?
RAR We have tried it, as suggested in an article,1 and could not see any clinically significant improvement in rapidity or permanence of bite opening. We have utilized vertical elastics occasionally from upper to lower first molars--usually in the Third Stage, to hold them in tight occlusion, not to erupt them to open the bite.
PCK We would use vertical elastics on molars, not as a means of extruding them to prop the bite open, but to change their buccolingual or mesiodistal inclinations. I think it would be wrong to encourage bite opening by an excessive eruption of the posterior teeth. We get some elevation of anchor molars due to the vertical component of force in the Class II and Class III elastics. We do recognize that this is part of the bite opening of the Begg Technique. It is not necessarily what we would desire, but it does help to get the anterior teeth edge-to-edge and out of occlusion, to facilitate rapid anteroposterior changes in the dental arches and individual tooth movements.
HGB Another factor in bite opening in the Begg technique is the angle of the molar buccal tube to the occlusal plane. It has been suggested that the angle be altered mesiogingivally. Would you find that an asset?
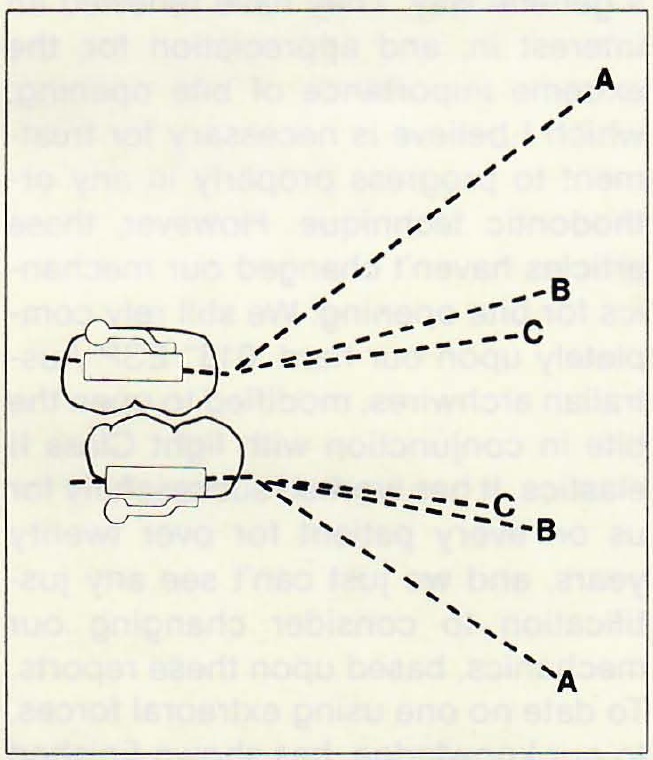
PCK There seems to be no justification for angling the buccal tubes. The only purpose that we can see is to place the anterior portion of the archwire lower in the mucobuccal fold. Anchor bends are designed for this purpose. They can be modified according to the needs of each case, and also changed in degree as treatment progresses and the bite opens (Fig. 12). If the tube is inclined at some preset angle, then the orthodontist must continually compensate for that angle throughout treatment. It would require severe gingival steps in the archwires, and reverse anchor bends once the bite opens.
RAR I have tried angling the buccal tubes, but I can't see any great improvement over what we have been doing previously.
HGB Would you discuss the relationship of root apex to cortical bone during bite opening mechanics?
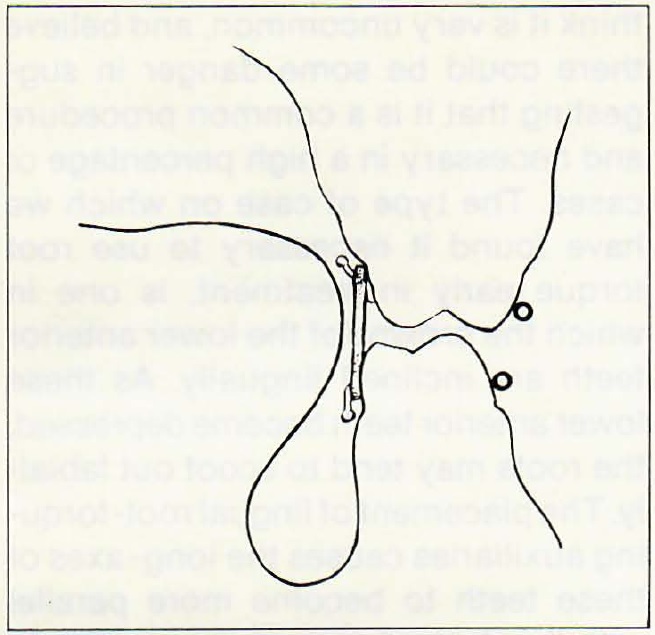
PCK Harry, I think we would agree that there are times when it might be advisable to alter the relationship of the apices to cortical bone; in other words, indications for anterior root torque early in treatment. However, I think it is very uncommon, and believe there could be some danger in suggesting that it is a common procedure and necessary in a high percentage of cases. The type of case on which we have found it necessary to use root torque early in treatment, is one in which the crowns of the lower anterior teeth are inclined lingually. As these lower anterior teeth becomedepressed, the roots may tend to scoot out labially. The placement of lingual root-torquing auxiliaries causes the long-axes of these teeth to become more parallel with the desired path of depression. In the upper arch, I can't think of ever having to do that sort of thing in twenty years.
I think we find bite opening most difficult in low angle cases. I believe the reason could be related to the very fact that it is a low angle case. It might be that the patient has stronger musculature, stronger masseter muscles than say, a patient with a normal angle. He or she could even be a habitual "clencher". Therefore, there is very little chance for us to benefit from the slight elevation of anchor molars from the Class II elastics, which is a recognized part of bite opening. The persistent heavy forces keep these teeth down.
PAR Adults with deep bite, low angle malocclusions are often bruxers. A mild muscle relaxant before bedtime has been useful in my practice to help break the bruxing pattern. This permits the slight elevation of the anchor molars from the light Class II elastics to help open the bite.
HGB You mention that you do not use looped arches in 90 per cent of your cases. How does the looped arch affect bite opening?
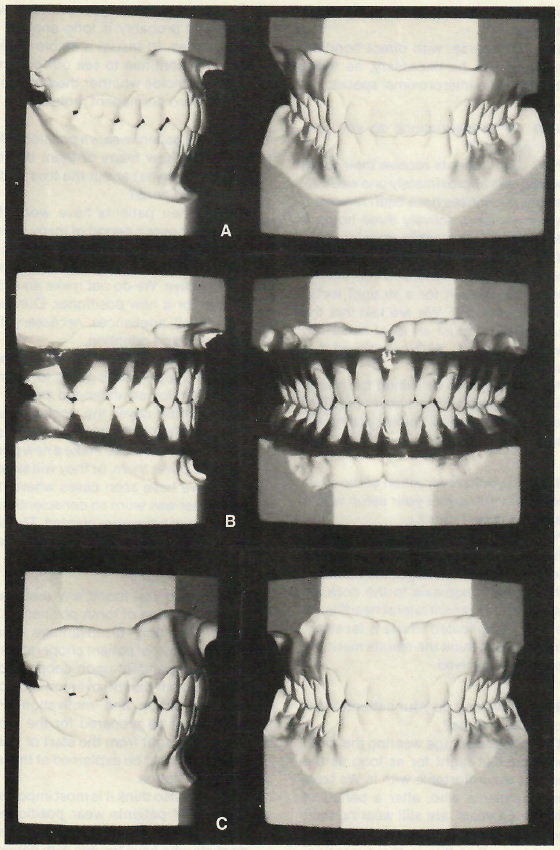
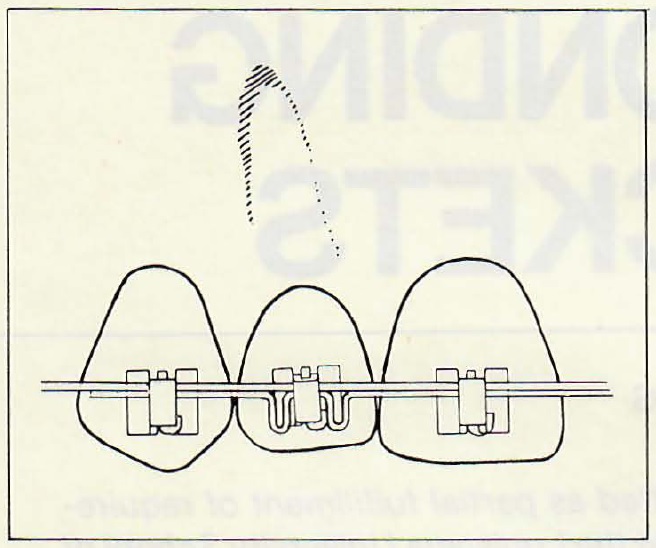
PCK I think we have all recognized for years that the looped archwire is not as efficient for bite opening and anchor molar control as a plain archwire. We have all tried through the years to eliminate the loops wherever possible. Now, with our CO-AX wire, we can delegate the alignment of anterior teeth to an archwire auxiliary, much as we have delegated the torquing of teeth to an auxiliary in Stage III. This enables us to use a harder .016" wire (ESP) for bite opening. We get much more rapid and controlled bite opening. By controlled I mean that all the anterior teeth seem to move together. With anterior vertical loops, the canines would go first, then the laterals, then the centrals, giving a "rainbow" effect (Fig. 13). Of course, anchor molar control is also much better in the absence of vertical loops in the anterior. In the future, we are going to see very few loops in the Begg Technique, and bites opening much more quickly, with anchor molars under much better control.
HGB Let's turn the question around and consider the open bite, anterior and posterior. How do you utilize your intermaxillary elastics in these cases?
PCK Class II or Class III elastics are a very integral part of treatment of an open bite case, because the vertical component of force from these elastics can help close the bite, in conjunction with archwires having very slight anchor bends. This phenomenon was illustrated earlier in this interview. Of course, the function of the anchor bends in these cases would be for anchorage, not for bite opening.
RAR It must be remembered that most cases are started alike--Class II , Class I, deep overbite, open bite--they are all started with Class II elastics. The only time we wouldn't start with Class II elastics is where we have an edge-to-edge, or slight Class III tendency of the anterior teeth. If this were an extraction case, we would start with horizontal elastics.
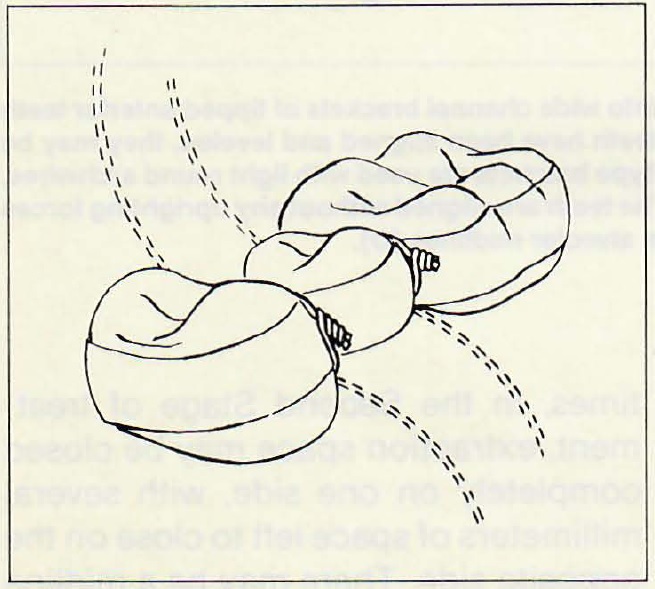
Posterior open bites are not too common. However, we now use vertical elastics from the lingual of the upper molar to the lingual of the lower molar to help control tongue position (Fig. 14). If necessary, we would also use them on the buccal. However, the lingual elastic is usually enough. If we find posterior open bite developing in Stage III, it generally is a result of too much curve in the archwire, or too much bite opening bend. Usually in these situations, we use vertical elastics on the buccal.
HGB While we are considering the anterior teeth, please explain why midline discrepancies seem to correct so readily with Begg mechanics.
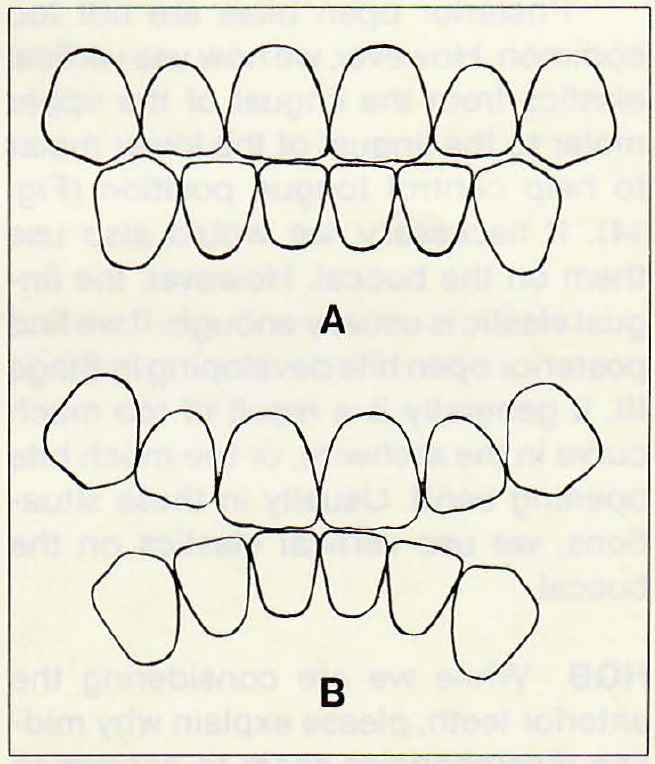
PCK Because the Begg Technique avoids the application of any mesiodistal uprighting forces to teeth until the Third Stage. This is possible through the use of a modified ribbon arch type bracket. In other words, if force is applied, it is strictly applied to the crowns of the teeth during Stages I and II. The single point contact between the archwire and the bracket leaves the root apices relatively undisturbed. In most malocclusions, midline discrepancies are originally caused by mesiodistal tipping of the anterior teeth, permitted by asymmetrical tooth loss or crowding. However, when wide channel brackets are used, even the lightest, most resilient archwires would immediately begin applying pressures to upright teeth, which cause the crowns of the teeth to move in one direction, and the roots in the other. The result is that the teeth become uprighted across the midline.
If, initially, the anterior teeth in one arch lean to the left, and those in the other arch lean to the right, and light archwires are placed in wide channel (Edgewise) brackets, a real midline discrepancy is created (Fig. 15). As extraction spaces are closed, this discrepancy is passed on to the buccal segments, creating a tendency for a Class II occlusion on one side and a Class III on the other.
RAR Orthodontists who have practiced the Begg Technique over a period of years very rarely report a problem with midline discrepancies. Many times, in the Second Stage of treatment, extraction space may be closed completely on one side, with several millimeters of space left to close on the opposite side. There may be a midline discrepancy at this time. However, as al I spaces close, or teeth become uprighted during Stage III, the midline is corrected automatically. HGB Let's consider some random factors. In treating adults, how do you alter your mechanics to compensate for missing posterior anchor teeth?
RAR On occasion, when molar teeth are missing, the bicuspid tooth is used as an anchor tooth, with a buccal tube on its buccal surface. In cases where there are bridge replacements for missing teeth and the bridge is maintained during treatment, the band encircles the entire bridge and is ligated around the contact areas, mesial and/or distal to the pontic (Fig. 16). We have, on occasion, talked about soldering the first and second bicuspid bands together with a tube, to act as a multirooted anchor tooth. However, we have not done this to date.
The gingival condition and level of bony support are of prime importance when diagnosing adult patients with potential periodontal problems. We would hesitate to start treatment in a case where there is severe tissue inflammation and hypertrophy. The patient would be referred to a periodontist first, for evaluation and/or treatment.
HGB When the perio problem has been corrected and there has been appreciable bone loss, how do you protect weak but savable teeth?
RAR I think, in general, we would stay away from orthodontic treatment in a case where the prognosis of saving teeth would be doubtful.
PCK If we did straighten teeth that had very little bony support, we would probably recommend that they be maintained with a fixed splint rather than a removable appliance.
HGB Do you locate the brackets differently on the lower anterior teeth in deep bite cases?
PCK We never compromise bracket positioning because of the degree of overbite. We put the brackets and archwires on at the same visit. The patient may be biting on some brackets when he or she leaves our office. However, the bite opens so rapidly, it isn't a problem.
HGB With bonding an established technique, are lingual attachments a problem?
PCK The only lingual attachments we normally use are molar hooks. Since we still use bands on most molars, we usually are not bonding on the lingual. However, special attachments are presently being produced for lingual bonding.
HGB Without lingual attachments, how do you "fix" the posterior segments to avoid space opening?
PCK We simply bend the ends of the archwires around the distal ends of the molar tubes. Sometimes we run elastomeric thread, or a steel ligature tie, from the molar lingual hook to the archwires between the canine and the lateral. This tie prevents distobuccal rotation of the molar and/or keeps spaces closed, if the end of the archwire is too short to be bent around the distal of the molar tube.
HGB Do you incorporate the second molar into the appliance in Stage III?
PCK On rare occasions, when patients have been uncooperative to the degree there has been an abuse of anchorage, we will band the second molars. In these cases the prolonged treatment time has caused the first molars to tip to such an extent they no longer have value as anchor teeth. They are then treated as "third" bicuspids, with brackets replacing their molar tubes. Of course, we also band second molars when they are rotated, or need to be corrected buccolingually. If an orthodontist is continually having to band second molars because they are rotated or displaced buccolingually, he is probably not reducing tooth substance as much and/or often as necessary.
RAR On occasion, at the start of treatment second molars are rotated, particularly lower second molars, and in cases such as this we would band second molars. The molar tube is put on the second molar, and a regular bracket on the first molar.
PCK If the case Bob just referred to were an extraction case and teeth were extracted prior to treatment, rotations of the second molars may improve without dealing with them directly. As the first molars move mesially during space-closing procedures, the second molars may, for the first time, have adequate space to assume normal positions. Pressures acting on these teeth from the tongue, cheeks, transeptal fibers, occlusion and the natural tendency for mesial migration, are often all that is needed, given adequate space, to correct a malpositioned second molar.
HGB Class II mechanics is an important part of Begg therapy. Do you use Class II mechanics throughout all stages of treatment?
RAR As needed to maintain the anterior teeth edge-to-edge. At the end of Stage I, the anterior teeth would be edge-to-edge. The patient is then instructed to wear Class II elastics enough to maintain this relationship throughout the rest of fixed appliance therapy.
HGB What has been your experience with root resorption?
RTR Like other orthodontists who have been in practice for any length of time, we see a certain percentage of cases that show a greater, or lesser, degree of apical root resorption. It is difficult to know in advance which patient might show resorption. There doesn't seem to be any relationship between resorption and length of treatment time, the severity of the malocclusion, or the degree of tooth tipping during Stages I and II. For many years we took x-rays after each stage of treatment, to determine if and when root resorption occurred.
PCK It seems most apical resorption occurred in the nonextraction cases, during bite opening. It doesn't appear to be related to the tipping or torquing of teeth.
HGB When you have root resorption, do you ever stop treatment?
RAR We have never stopped treatment due to root resorption. Perhaps we have never had a case that had such extreme root resorption that would even be considered. To my knowledge, we have never had enough resorption that would bring a question to the mind of the dentist, or the patient.
I think that, no doubt, there is some root resorption in most cases that are treated, but certainly not to the extent that it would cause any alarm in the mind of the dentist, or the patient. In our practice, a panoramic x-ray is taken before treatment, when the appliances are removed, and again when finished records are taken months later.
RTR It is probably wise to mention the possibility of root resorption at the time of the consultation. However, this should be done in a manner so as not to alarm the prospective patient and parents. If root resorption does occur, I would just mention to the parents that this is often just a scar of orthodontic treatment, and that we have never seen a patient lose any teeth due to root resorption.
PCK Twenty years of practice have shown me that root resorption, related to tooth movement in the Begg Technique, is not a clinical problem. At least, it hasn't been for me. Of course, we look mainly at apical resorption. There are those who also measure, and look for, lateral resorption. We mentioned briefly, elsewhere in this interview, the research done by Dr. Milton Sims on lateral root resorption, evidently caused by excessive forces from headgear.
HGB Do you have thoughts on what predisposes to root resorption?
RAR The vertical movement of teeth, as might occur with anterior vertical elastics in the treatment of open bite cases. Of course, as mentioned before, we do not directly apply vertical forces to erupt teeth in the Begg Technique. We apply light, vertical elastics on the lingual to block and discourage the tongue.
HGB Do you think that Begg theory and treatment procedures routinely produce results compatible with the theories of good occlusion?
PCK I would say that the Begg Technique, when utilized properly, is able to produce results as compatible as possible, considering we are arranging unworn teeth with cusps and fossae. In other words, according to studies of stone age man's dentition, the proper occlusion for man includes an anterior edge-to-edge relationship and very little cuspal interference due to the wearing away of the teeth by coarse and gritty foods. Of course, during treatment with the Begg Technique, we attempt to simulate stone age man's dentition. We quickly bring the anterior teeth to edge-to-edge relationships. This facilitates interarch corrections, and makes possible the overrotations of teeth, which in many cases would be absolutely impossible if the normal degree of overbite existed throughout treatment.
I would say a properly treated case using the Begg Technique, which has included overcorrection of all tooth movements, uprighting of roots of teeth across extraction spaces, and the proper inclination of anterior teeth as well as overrotations would, after the removal of appliances and settling, exhibit the best occlusion possible with civilized man's dentition.
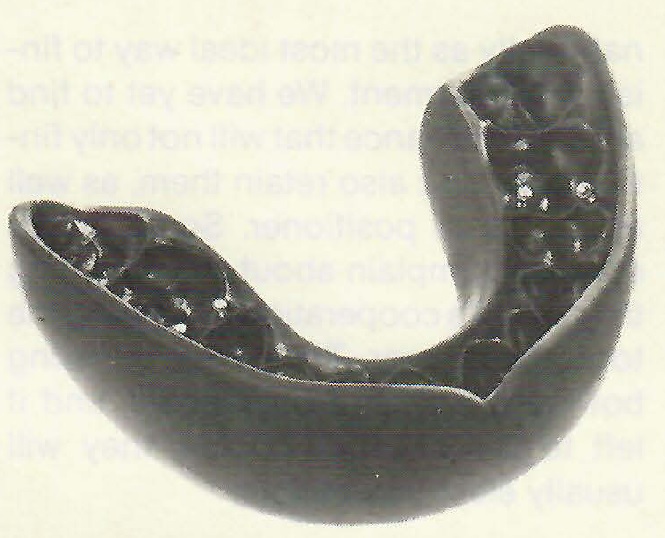
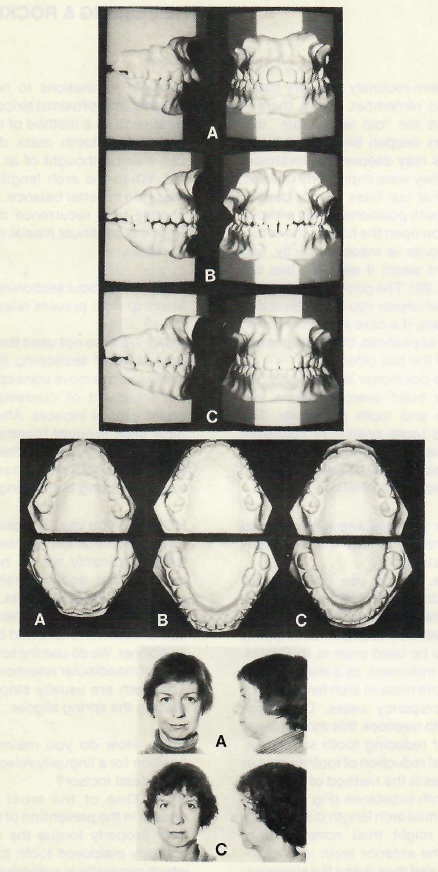
RAR I might add to this, the fact that the finest method to finish treatment is with a tooth positioner. This is not to say that Nature does not have the final say on how the teeth will settle. However, with the aid of the positioner in controlling this settling, we feel that we have the best chance to maintain ideal occlusal relationships..
HGB Do you find, posttreatment, that molar cusps are in poor position because of improper mesiodistal or buccolingual axial inclinations of the molars?
RAR I believe this gets back to the basic treatment in following the Begg theory. The rotation of upper molars particularly, is an important point in finishing cases. The upper molars, especially in extraction cases, have a tendency to rotate around their lingual roots, causing distobuccal rotations. This must be guarded against, if we are going to finish with molars in good relationships.
PCK During the Begg Technique we attempt to keep the anchor molars upright at all times. Molars are not tipped distally to "set up anchorage". The best anchorage is provided by an undisturbed tooth. It is only through poor patient cooperation, or the use of excessive anchor bends or archwire sizes, that anchor molars tip distally.
Weak anchor bends, or archwires, can result in the mesial inclination of anchor molars during treatment. However, when treatment is done properly, with the molars held upright, there should be no mesiodistal inclinations. Of course, in the Third Stage we can have our patients wear vertical elastics near the end of treatment, to encourage the desired relationships between the distobuccal cusp of the upper first molars and the mesiobuccal cusp of the lower second molars.
HGB Are there special steps you take to avoid molar cusp interference?
PCK No. When a round wire is employed, there are no buccolingual root-torquing forces applied accidentally to anchor molars. These teeth are free to "rock" buccolingually into good occlusion during all stages of treatment. It is no problem with the Begg Technique.
HGB With the molars having such "freedom" do you use any special finishing procedures?
PCK Of course, until just recently the only precision finishing in this office has been done by use of the tooth positioner (Fig. 17). We know that a tooth positioner, properly made and worn, can produce the finest occlusions possible. Lately we have been working with finishing archwires, bent to a setup made near the end of treatment. The archwire is bent to fit passively on the setup, and transferred to the patient's teeth near the end of Stage III, to provide the same tooth movement normally accomplished with a positioner. We haven't had enough experience with this technique to evaluate it. At this point, I would say it seems as though it will work. However, the present procedure involves a lot of extra work on the part of the orthodontist. If more of the steps could be delegated to laboratory personnel, it may hold some promise as a method of precision finishing in the future.
RAR Certainly over the almost forty years in our practice we have used tooth positioners to finish our cases. Of course, the positioner was invented by the late Dr. H. D. Kesling in the early 1940's, to finish Edgewise treated cases. It now has been accepted internationally as the most ideal way to finish any treatment. We have yet to find another appliance that will not only finish cases, but also retain them, as well as the tooth positioner. Some orthodontists complain about not obtaining the patient's cooperation in wearing the tooth positioner. They may be using both retainers and positioners, and if left to the patient's choice, they will usually elect the retainer.
HGB I appreciate the importance of the positioner for finishing, but let's consider the appliance itself a little bit more. Do you find it possible to obtain optimum cuspal occlusion and centric occlusion prior to appliance removal?
PCK In general, the answer would be "No': because our appliances are designed with bayonet bends and offset brackets to hold teeth in positions of overcorrection throughout treatment. I am thinking especially now, of the rotations of anterior teeth. As long as the appliances are in place, one wouldn't be able to achieve what is called the optimum cuspal occlusion. But we know, from our own experience and that of Dr. Begg, that overcorrection of all tooth movements helps insure stability after the appliances are removed. We use a tooth positioner to bring the teeth into the desired occlusion. Dr. Begg uses an upper circumferential retainer to help guide his overcorrected teeth into normal relationships.
RAR I think Dr. Begg's theory of overcorrection is one that has never been emphasized enough. In our past experience, before Begg treatment, we never overcorrected to the extent we are doing at present. By overcorrection we mean finishing with the anterior teeth nearly edge-to-edge, and individual tooth rotations slightly overcorrected. However, the tooth positioner is made with the teeth in proper alignment. It works with the natural tendency for relapse, to create the finest occlusion possible, and then functions as a retainer (Fig. 18).
HGB Do you think that ideal cuspal occlusion in centric relation is the primary treatment goal vs. what we find in normal non-treated occlusions?
PCK We are striving for a better relationship of teeth than you would find in the "normal" nontreated occlusion. We are attempting to place the teeth in the best relationships possible, removing tooth substance when necessary, to obtain the proper balance between teeth and basal bone. Proper axial inclinations are achieved for stability, so that the occlusion can withstand the constant mesial migration and vertical eruption that is going to go on in the years after treatment. So we might, in treating our cases, set them up with this in mind--so that they will be more stable in the years ahead than those "normal" nontreated occlusions to which you referred.
HGB A good stable occlusion is certainly important because of the problems we run into when it doesn't exist. What is the incidence of bruxism and TMJ dysfunction in your practice?
RAR Fortunately it is not a frequent problem in our practice. Most patients we see with this problem, usually come in after having first seen a physician or general dentist. They do not seem to migrate to our office when this problem first develops. The cases we have seen have been out of treatment from three to ten years, or have never had orthodontic treatment. They are not necessarily deep overbite cases, and generally the occlusions are almost ideal. Of all the cases we have had, all but one have been female, ages from twenty to thirty years.
HGB Do you find that these patients exhibit any specific primary etiological factors?
RAR Apparently problems develop in younger women who are under stress or strain of some kind, creating a bruxism and muscle spasms.
HGB How do you treat them?
RAR After a recent conversation with Dr. Fay Culbreth of Charlotte, North Carolina, we have adopted his procedure in correcting these problems. He uses an equilibrating paste, much the same as would be used in equilibrating dentures in an articulator. This is usually accomplished within three to eight adjustments, about one week apart. We have had great success in this method of eliminating the TMJ problem. This really gets back to attritional occlusion, and reduces prematurities which evidently have a tendency to create this bruxism .
PCK In the treatment with the paste, we might precede that with some spot-grinding, using an indicator wax and a diamond stone to take down any obvious prematurities. However, the fine wearing-away of the teeth accomplished by the patient going into lateral and anteroposterior excursions, is far more accurate.
HGB Do you equilibrate prior to appliance removal?
RTR No, we would not equilibrate while the appliances were on. If the patient is asymptomatic, I would question whether equilibration later on is even necessary.
PCK I think we all would equilibrate incisal edges of fractured anterior teeth, or the tips of canines that have been moved into lateral incisor positions.
HGB What about equilibration during and after retention?
RAR The only time we might equilibrate after appliances have been removed, would be if the patient were having some TMJ problems.
PCK We couldn't afford to adjust all of our patients forever. I think they get locked into an occlusion that is the best occlusion possible, in the absence of attritional occlusion.
RTR I see no reason to continually equilibrate. If the patient is happy and the occlusion seems good, I question the need for continual equilibration.
HGB Since you don't find much TMJ dysfunction, do you think that there is "inherent oral protection" of the temporomandibular joint and muscle system?
PCK I would say, "No": based on Dr. Begg's study of the normal occlusion for man. It is not normal for man to retain cusps and fossae on his teeth throughout life. Man's dentition has developed over millions-of years. The joints, muscles, supporting bone--everything is designed to cope with an occlusion that has no cuspal interference at all. Primitive man chewed with wide lateral excursions, often with occlusion only possible on one side at a time--"X" occlusion 2(Fig. 19). Those who feel "cuspal protection" is some grand design of nature should study the development of man's dentition. Dr. Begg's greatest contribution to orthodontics (and dentistry as a whole) has not been his treatment methods, but rather his explanation of the development of man's occlusion.
HGB Does this account for asymptomatic joints and muscles in malocclusions?
PCK Man's occlusion and supporting structures have the ability to adapt (within limits) to any situation. The fact that a patient is asymptomatic indicates his or her particular limits have not been violated. Cuspal interference (rise) probably causes more TMJ discomforts than it "protects"
HGB Do you have a special procedure for retention?
PCK The best procedure for retention is overcorrection, which we have stressed throughout this interview. Not overcorrection near the end of treatment; overcorrection must be practiced right from the start. The teeth and arches should be held in positions of overcorrection as long as possible. Our procedure for retention at the end of treatment is the placement of a custom tooth positioner. Some orthodontists remove all bands (except from cuspids and molars), and place archwires and space-closing elastics to close spaces while the positioner is being constructed.
RTR Of course, with direct bonding this may not be necessary, as there should be no interproximal spaces.
HGB What instructions do you give your patients?
PCK Our patients receive their tooth positioners approximately one week after the appliances have been removed, and wear them actively three hours a day, and passively while sleeping.
RTR Some orthodontists place the positioner on a Friday, and instruct the patient to wear it for a straight forty-eight-hour period. We are told that the patient has almost an ideal occlusion within one week. We haven't tried that procedure.
PCK It seems to be asking too much, since it is possible to obtain excellent results without resorting to such measures.
HGB In your construction of the positioner, do you orient your setup with a facebow registration?
PCK We use a custom hinge-axis in the construction of all of our tooth positioners. However, we get the relationship of the hinge-axis to the occlusal plane, from a recent lateral headfilm. It is very complicated to use a facebow, and we don't think the results merit the extra time involved.
HGB How long do your patients wear tooth positioners?
RTR We encourage wearing the tooth positioner at night for as long as the patient is comfortable with it. We have many patients who, after a period of five to ten years, are still wearing their positioners when sleeping. However, I would say that this is the exception. Most patients tend to tire of wearing the positioner after a year or two. However, that probably is long enough in most cases, to insure a stable occlusion. We continue to see our patients until we decide whether there is room for the third permanent molars.
HGB If a patient wears a positioner for ten years, how many of them do you make? And what about the fees under these conditions?
RAR When patients have worn the positioner over a period of many years, certainly there is somedegeneration of the rubber to the point where it is not too effective. We do not make an extra charge for a new positioner. Our fees include all appliances necessary for treatment and retention.
It might be well to remind the readers that if a patient is going to wear a positioner for an extended period of time, it must cover the occlusal surfaces of all teeth. As third molars erupt, it will be necessary to make a new positioner to cover them, or they will super-erupt. We have seen cases where the positioner was worn so conscientiously that open bites were created. The only teeth in occlusion were the super-erupted third permanent molars.
HGB Have you found any disadvantages in the use of tooth positioners?
PCK The only disadvantage I can think of is lack of patient cooperation. It is 100% dependent upon cooperation. This problem can be overcome by patient education and motivation. Patients must be prepared for the tooth positioner right from the start of treatment. It should be explained at the initial consultation.
RAR We also think it is most important to have all patients wear positioners, not just a few. It seems that the orthodontists who have trouble with patients wearing positioners are those who do not use them routinely on every case.
RTR Also remember, Harry, there is nothing to the "old wives' tale" that positioners deepen bites. That is not true. Bites may deepen posttreatment because they were improperly opened. We find that our bites do not deepen any more with positioners than without.
PCK If you open the bite on the setup, the positioner is made correctly, and the patient wears it well, the bite will open (Fig. 20). The positioner will do to the teeth whatever you do to the setup.
RAR Again, if a case is overcorrected with fixed appliances, there is not much chance of the bite closing.
PCK The positioner is set ideally. We no longer build overcorrections into the setup and tooth positioner. The setup and tooth positioner represent the ultimate in precision finishing. Overcorrection should take place during fixed appliance therapy.
HGB Do you use any other special forms of retention aids, such as interproximal stripping?
PCK Yes, we do use interproximal stripping during the retention period, to increase the stability of the lower anteriors. However, interproximal stripping could also be used prior to treatment, or during treatment, as a means of reducing tooth mass in arch length/tooth mass discrepancy cases. Orthodontists tend to overlook this most natural method of reducing tooth substance. Mesiodistal reduction of tooth widths in many cases is the method of choice to reduce tooth substance (Fig. 21).
RAR In a mild arch length discrepancy case, we might treat nonextraction, bringing the anterior teeth into alignment first, and then doing the stripping. We feel the surfaces created are then better able to prevent relapse following appliance removal.
PCK This stripping could also be done at slight inclinations to help prevent relapse. Interproximal stripping prior to treatment, as a method of reducing an arch length/tooth mass discrepancy, can also be thought of as a retention aid. When the arch length and tooth mass are in better balance, there is less chance of a recurrence of crowding from the continual mesial migration of the teeth.
HGB How about sectioning transeptal fibers to help prevent relapse of rotations?
PCK We have not used the "Edwards" procedure of sectioning fibers. However, we do remove transeptal fibers in our treatment of diastemas between upper central incisors. After the teeth have been brought together, we don't have just the fibers cut. Rather, the tissue is removed. The teeth are then held together during the healing process.
HGB Do you use "A" splints or other forms of permanent splinting?
RAR Ordinarily we do not use any type of splint, and we rarely use lower cuspid-to-cuspid retainers. Stability is gained through overcorrection during active treatment, followed by the tooth positioner. We do use the spring aligner type of mandibular retention, if needed. The teeth are usually stripped before placing the spring aligner.
HGB How do you maintain proper position for a lingually relapsing maxillary lateral incisor?
RAR One of the most important phases in the prevention of this relapse is to properly torque the root of the lingually malposed tooth to the labial, which generally is sufficient to prevent relapse in this type of case.
PCK I think the best way to retain that tooth would be to retreat with some fixed appliances to overtorque the root of the tooth labially (Fig. 22). This, of course, should have been done during the Third Stage of appliance therapy. Stabilization of the crown with the usual retainers (fixed or removable) will only delay the eventual relapse of the tooth. The proper way to retention is through overcorrection. I often wonder why it is so difficult to get orthodontists to consider overcorrection during active treatment.
HGB Do you assign a role to the third molar in relapse?
PCK I personally don't assign much importance to the third molars (upper or lower) when looking for the cause of relapse. Mesially inclined lower third molars with their crowns caught under the distal contact areas of second molars, are the effect of crowding, not the cause. Study the development of man's dentition for the answer. Don't blame the third molars.
RAR I am in agreement. It is just coincidental that third molars often erupt at the same time relapse occurs. Perhaps much of this is due to mesial migration occurring at the time of the eruption of these third molars.
PCK If you feel the third molars are causing lower anterior crowding, merely take dental floss to see if there are tight contacts. Quite often the contacts are not tight, especially in extraction areas. This indicates the third molars are not the direct cause of the crowding.
HGB Can growth and development be controlled orthodontically as a means of relapse prevention?
RAR We don't consciously attempt to control growth and development. It may be affected during normal treatment procedures, through the application of our relatively light forces, and perhaps to some extent this does control the direction of growth.
HGB Do you feel that precision finishing helps reduce the chances of relapse?
PCK A precision finish, whether created by the ever-elusive "automatic appliance" or diligent wire bending on the part of the operator, would not, in itself, create a stable result. We feel stable results are caused by proper diagnosis in the beginning, and overcorrection during treatment.
HGB Then there is still a place for the clinical orthodontist?
PCK Definitely! Can't be done any other way.
RAR No matter how we try, I don't think there is any type of automated appliance. The operator must use judgment and care in the manipulation of any orthodontic appliance. There certainly is still a place for the clinical orthodontist.
HGB Gentlemen, thank you on behalf of JCO and its readers.