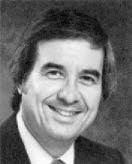
JCO Interviews the Kesling & Rocke Group on Begg Technique, Part 1
HGB The Kesling & Rocke Group represents the mother lode of Begg philosophy and treatment in the United States. Among you, you represent well over 50 years of Begg experience. Although the basics of Begg philosophy and technique remain essentially unchanged, your innovations in technical procedures and mechanics have improved Dr. Begg's original methods, and you have been instrumental in spreading the use of this philosophy of treatment through the many classes of orthodontists who have made the trek to the "Mecca of Begg Philosophy" at the Center in Westville in order to-learn the technique or refresh themselves with new thought and procedure.
Bob, the Kesling & Rocke Group is one of the oldest orthodontic associations. What do you believe is the reason for the long term success of your association with the late Dr. H.D. Kesling?
RAR Our relationship started during the depression, ripened with time, and eventually lasted over 45 years. In trying to analyze the success of any relationship, certainly hard work on the part of all parties is most important, and there must be mutual admiration and respect. There is no place in a successful partnership such as this for petty jealousy. And, the parties must have an understanding before the association starts.
HGB Would you have a written contract right from the start?
RAR We definitely would have some written arrangement with any associate joining the practice. There might be a trial period of three to six months, following this written arrangement and, if things do not work out, the contract could be made null and void without any ill feelings.
PCK Each partner should have certain areas of responsibility. This helps assure the smooth daily operation of the practice.
HGB Do you mean administrative or clinical responsibilities?
PCK I was thinking of administrative duties.
HGB On what basis do you divide up the duties?
PCK Duties are delegated, whenever possible, according to the individual's particular abilities, preferences, and time available.
HGB Do you rotate duties through the partnership?
PCK From time to time; but in general, if it works well, we just keep going with the same arrangement.
HGB What do you feel are the advantages of a group practice over a solo practice?
RAR The value of consultation with your associates makes a big difference in patient care. Vacation times can be readily arranged, and patients are better taken care of in a group practice than they are in a solo practice. I think that a group practice can grow more readily than a solo practice because of the association of the various partners in the community.
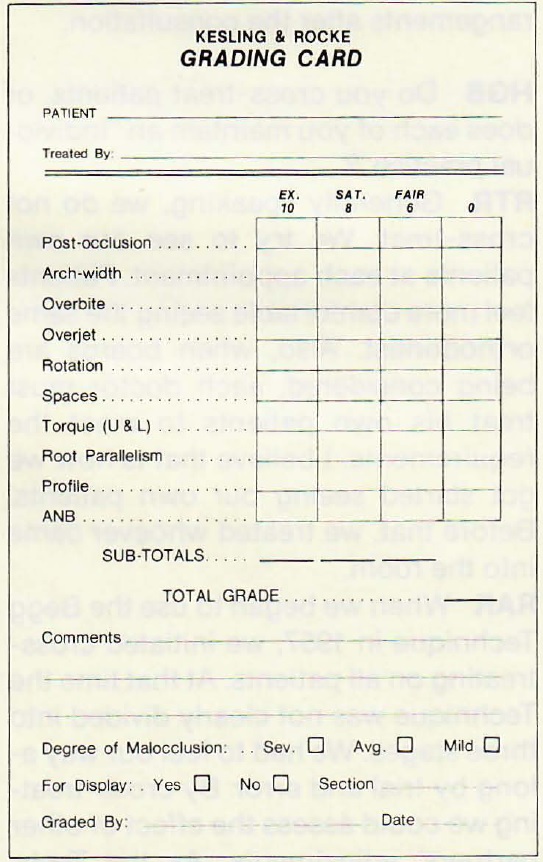
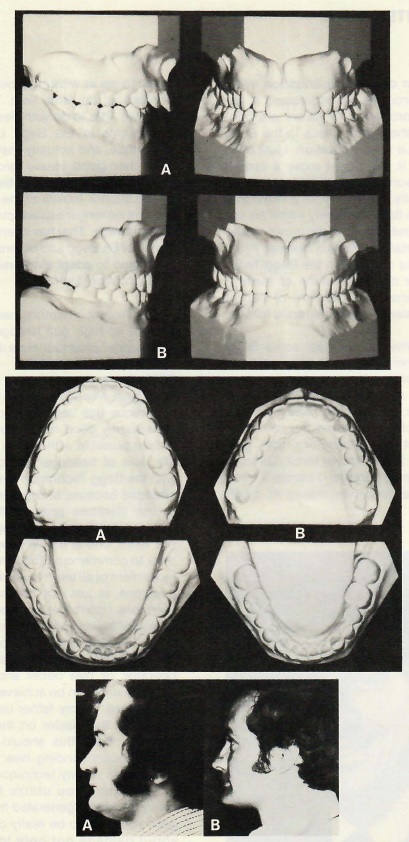
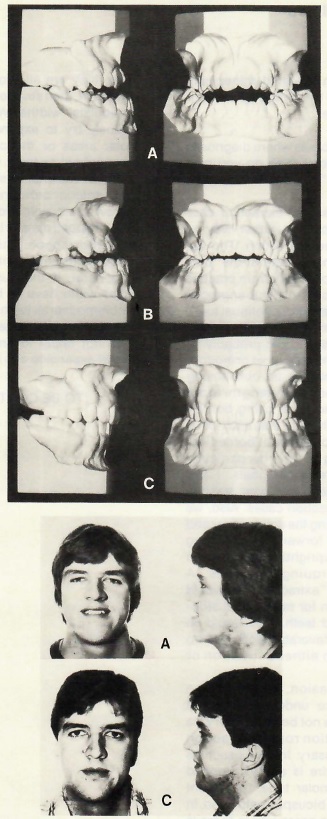
PCK The patients benefit because a member of the group would think twice before compromising an adjustment or a finish if one or two, or more, partners were going to judge his or her work. We review the final results of each case among all the members of our group. At the completion of treatment we evaluate each case, using a special grading sheet to assess the quality of treatment and result achieved (Fig. 1).
Another advantage of a group practice is, of course, the economics of sharing overhead--items that in a solo practice would have to be carried on one man's shoulders can be distributed. And, as Bob mentioned, vacations, illnesses, and business trips can easily be covered in a group practice.
HGB How are the patients assigned to individual doctors?
RTR Basically, the patients are randomly assigned to doctors, unless they express a preference. It is up to the receptionist to assign new patients in a fair manner, according to the percentage of ownership each member has in the partnership.
HGB Who does the diagnosis, case presentation, and financial arrangements in your practice?
RTR Each doctor does his own diagnosis and case presentation. We do get together on those cases where the diagnosis is difficult. The financial arrangements are presented by the doctor at the time of each presentation. The secretary then makes the detailed arrangements after the consultation.
HGB Do you cross-treat patients, or does each of you maintain an "individual practice"?
RTR Generally speaking, we do not cross-treat. We try to see our own patients at each appointment. Patients feel more comfortable seeing the same orthodontist. Also, when boards are being considered, each doctor must treat his own patients to meet the requirements. I believe that is how we got started seeing our own patients. Before that, we treated whoever came into the room.
RAR When we began to use the Begg Technique in 1957, we initiated cross-treating on all patients. At that time the Technique was not clearly divided into three stages. We had to feel our way along by trial and error. By cross-treating we could assess the effect of other partners' adjustments. As the Technique developed into its present state, we stopped this practice. However, we certainly cross-treat on emergency appointments, or if one is away from the practice for any length of time.
PCK Having done it both ways, I would say that everything else being considered, one can do a better job if he sticks with the same patients. You get to know each patient personally, and have a better chance of having them help you through maximum cooperation.
HGB What do you do if there isn't enough time to make the required adjustments at a given appointment?
RTR In general, we don't have that problem, perhaps because our practice is better organized than most. However, I feel that if an adjustment is necessary, it should be made at that time, even though it may create a backlog in the reception room. This would be particularly true if a problem were developing for that particular patient. It is very important to correct any existing or developing problem at the time it is noticed.
HGB What role do you assign to your auxiliaries?
PCK We don't have auxiliaries do as much work at the chair as I am sure is being done in other offices. Our assistants mainly hand us the instruments. They do not place archwires in the patient's mouth.
RTR In Indiana, auxiliaries can take impressions for diagnostic purposes, but not for the fabrication of appliances. They can also take x-rays, but cannot do irreversible procedures.
PCK Our practice is organized to take advantage of the efficiency of the Begg Technique. We only see our patients every six to eight weeks. We don't have to run a lot of patients through here like a mill. We have enough time set aside so that we can do whatever is necessary at each appointment. We have had patients come to us from other practices where they were upset at having assistants working on them most of the time.
HGB Do you use an open, or closed-end fee?
PCK We have a flat, closed-end fee for treatment, and that includes all the appliances we feel will be necessary to complete treatment, including positioners. And it also includes retreatment, if necessary.
RTR That is a firm fee, regardless of inflation, and it can be paid over an extended period of time, without interest charges. However, I am sometimes tempted to charge an additional fee if they missed retention appointments, and all of a sudden a year or so later they come in complaining of crowding.
PCK We all have some patients come back ten years later, with a little lower anterior crowding. If they want to go through corrective measures, there is no charge.
HGB Do you mean full appliance retreatment, or just corrections such as rotations or a slipped contact?
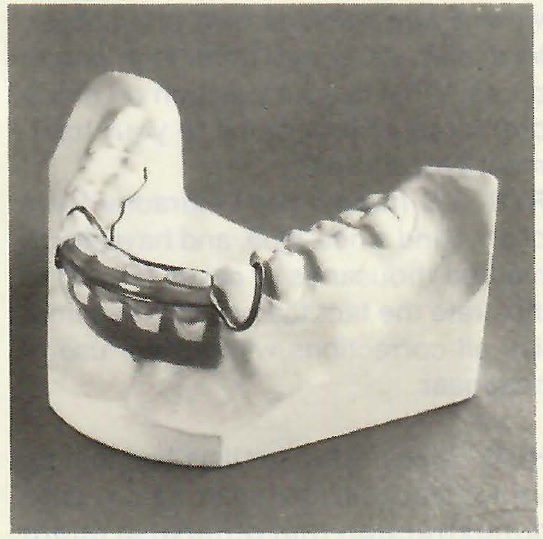
PCK The degree of retreatment would, of course, depend on the degree of relapse. We would do whatever is necessary to correct the situation, from full appliances on both arches to perhaps the simple placement of a Spring Aligner to correct lower anterior crowding (Fig. 2).
Happily, there are very few cases such as this. If it got to be a high percentage, we would probably have to reassess our approach. If you have diagnosed the case properly and treated it properly, you shouldn't have much relapse. I feel relapse is usually caused by the orthodontist erring in some way, before or during treatment. Perhaps the case was not diagnosed correctly at the start. We can do better today with better procedures, and more thought to overcorrection.
HGB What posttreatment changes would you accept before saying the case has relapsed sufficiently to require some active retreatment?
PCK Minor crowding of upper and lower anterior teeth, slight rotations of bicuspids, deepening of the bite. A decision to retreat is usually not made by the orthodontist alone. The patient's degree of satisfaction and wishes must be considered, also. It is sometimes surprising when we suggest retreatment to patients and they don't want it. They are perfectly happy. On the other side of the coin, one may have what he considers to be a beautiful result, and the patient (or "Mama") doesn't like it.
HGB Have you given any consideration to inflation? Since we quote long-term fixed fees, do you make any adjustment?
PCK We presently review our fees annually, and attempt to increase them to keep up with cost-of-living increases. In the 1960's we were lax on this point, and I feel we let our fees stagnate to relatively low levels. Of course, we don't adjust a patient's fee once it has been accepted. Once we quote a fee, that's it.
HGB Now that we have a little overview of your administrative procedures, let's discuss some treatment procedures. What is your position on extraoral force as it pertains to your treatment procedures?
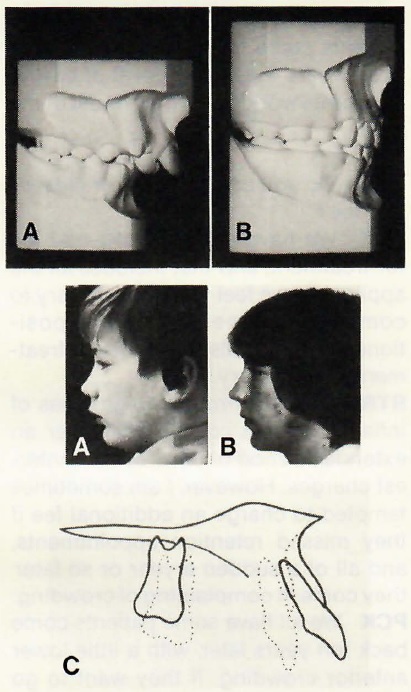
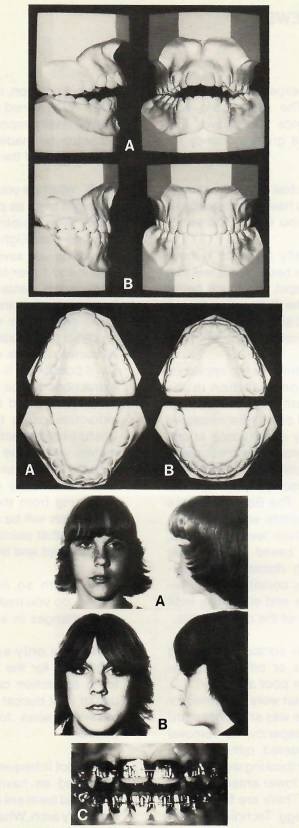
RTR We haven't used extraoral force of any kind since 1959, and have documented thousands of cases (Fig. 3) to illustrate the fact that we can accomplish all corrections without the use of headgear.
HGB Many orthodontists feel that by using headgear they can treat a case nonextraction that otherwise might require extractions. They don't want to "doom" the patient to the extraction of bicuspids.
RTR We would probably have a higher percentage of nonextraction cases if we used headgear. However, our feelings are that in "borderline" cases the results will be more stable if tooth substance is reduced, rather than teeth held back temporarily during treatment with headgear.
PCK Orthodontists with ten, twenty or thirty years of experience in treating patients usually agree that the results are more stable in those cases where no headgear was used and teeth were removed when necessary.
HGB What about bumpers and activators?
RTR I don't think we can really comment on these appliances, since we have not had much experience with them in our practice.
PCK I don't think there is any technique that can get things going as fast as the Begg Technique. If the child is old enough, if you can band the upper and lower six anterior teeth and the first molars, I think you ought to start the Begg Technique and forget about the lip bumpers.
HGB Would you discuss your use of early treatment in the mixed dentition?
RAR In certain cases such as:
(1) In Class III malocclusions, which may require one or two, or more periods of treatment until full growth is reached.
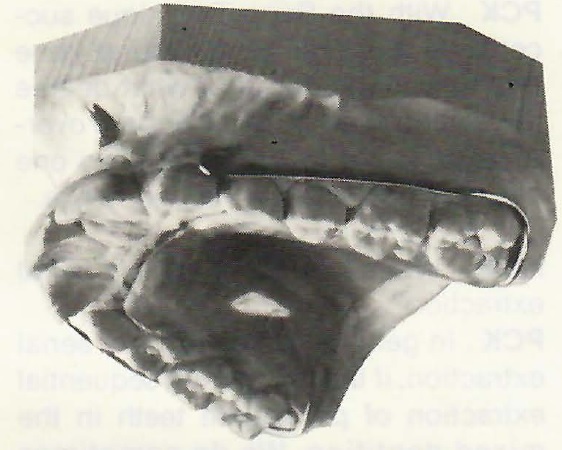
(2) In cases with extreme overjet, to reduce the maxillary protrusion to help insure that the upper anteriors will not be fractured, and assist the developing child psychologically. This is accomplished with a removable palatal appliance having a circumferential wire or elastic across the anterior teeth (Fig. 4).
Other than that, we do no early treatment. In most cases our experience has shown that if cases are started too early (in the developing dentition), the treatment time will run extremely long. If partial treatment is completed before the permanent dentition has erupted, further treatment may be required. This only wears the patient out, and we feel that it is not necessary.
PCK Early treatment might also be detrimental in that the limited amount of movement possible due to the absence of many of the permanent teeth might only result in masking the true severity of the malocclusion. The orthodontist could then be misled in the diagnosis, and not extract in a case which required a reduction of tooth mass. The result could be a bimaxillary protrusion at the end of treatment and/or relapse.
RTR We find that the Begg Technique is most efficient in treating cases when the appliances can be placed on all permanent teeth at the beginning of treatment.
PCK With the Begg Technique success does not depend on how early one begins treatment, but to what degree the teeth and even the arches are overcorrected, and that doesn't mean one has to get started at a very early age.
HGB What is your view on serial extraction?
PCK In general, we do not use serial extraction, if that means the sequential extraction of permanent teeth in the mixed dentition. We do sometimes recommend the removal of deciduous canines to help facilitate alignment of the anterior teeth, especially the lower. This is done to help prevent the lower anterior teeth from being crowded to such an extent that there is a destruction, and permanent loss, of both hard and soft supporting structures.
RTR In cases where there is extreme crowding of the permanent cuspids, we may remove the first bicuspids, but not enucleate them, up to perhaps six months before the date the appliance is placed. This facilitates eruption of the permanent cuspids, and improves the esthetics for the child at that time.
PCK That would be a case in which space is not very critical. When every bit of space gained from the extraction of teeth is required for proper positioning of anterior teeth, the placement of appliances must not be delayed. Uncontrolled posterior teeth will tend to tip and migrate mesially into the extraction sites.
RTR Sometimes I find it advantageous to remove the first deciduous molars ahead of schedule, to allow the eruption of the first bicuspids before the permanent cuspids.
HGB Do you use orthopedic procedure in your treatment?
PCK Yes. Rapid maxillary expansion is an orthopedic procedure when the patient activates the expansion screw properly. Incidentally, this is an excellent example of differential force at its highest force level. If the patient doesn't activate the screw rapidly enough, the force is so light that the teeth move through the bone orthodontically. If activated as instructed, the forces are so high that the teeth resist movement, transmitting the force directly to the bone and causing the palate to split orthopedically. However, I would say that in our office, we don't use as much rapid maxillary expansion as we did ten years ago.
Now we have had more experience, and know better which cases require this type of treatment than we did four or five years ago. We might have used it too often. Rapid maxillary expansion can definitely be a part of the Begg Technique in those selected cases that require considerable overcorrection of posterior crossbites to help insure stability after the appliances are removed.
RTR My experience has been that you get less relapse in crossbites if you do use rapid maxillary expansion.
HGB You make no other use of orthopedic force?
RAR I think with our orthodontic appliances we manipulate the teeth, and also cause changes in jaw relationships, even though the forces are light (Fig. 5). This could be interpreted as both orthodontic and orthopedic movement, if one accepts the fact that orthopedic forces can also be light forces.
HGB Many orthodontic treatment procedures rely very heavily on distalization of posterior teeth. What is your position on this?
PCK The movement of posterior teeth distally is contrary to the natural mesial migration of teeth. Distalization infers heavy forces as we understand it, extraoral forces. As far as we are concerned, there is no place in the Begg Technique for distalization. I just can't think of it. We might move a cuspid distally some, if it has been crowded out labially or mesially; or a molar that has been tipped mesially might be uprighted and therefore, the crown would move distally. However, I repeat again--there is no place in the Begg Technique for the distalization of teeth, if that means the movement of buccal teeth posteriorly with extraoral forces.
HGB Why do you feel some Begg practitioners use extraoral force?
PCK Some orthodontists with experience in other techniques that require headgear, feel they also need it with the Begg technique. When the results of treatment are satisfactory, they give credit to the extraoral force. Utilizing bite-opening bends and extraoral force to open a deep bite, makes as much sense to me as wearing a belt and suspenders at the same time. The headgear has little to do with desired tooth movements in the Begg Light Wire Technique, and actually may do more harmthan good. Heavy forces can be detrimental, because they tend to loosen the anchor molars to the point that they are no longer a satisfactory source of anchorage. That has been the experience of Dr. Begg and others who have attempted to adapt extraoral forces to the Light Wire Technique.
HGB Recent literature has stressed the use of high pull headgear to depress upper anteriors. How do you feel about this
PCK To my knowledge no one using high pull headgear with the Begg Technique has been able to show as consistently good results as has been proven possible without the headgear. My view of headgear in conjunction with the Begg Technique has not been changed because of recurring reports in the literature praising its virtues. Spectacular depression of upper anterior teeth, one at a time or all at once, prior to commencing the simultaneous movement of all teeth toward their final positions, is just not necessary. Furthermore, I don't feel it can be justified. It has not been shown that such procedures utilizing extraoral force place less demands on the patient and/or operator, or that better and/or more stable results can be achieved by such procedures. As my father used to say, "Let's put the plaster on the table". I certainly think this should be done before recommending new treatment procedures for any technique.
Any time you utilize forces as heavy as can be generated from headgear, you have to be really concerned about damage not only to cortical plates, but root surfaces as well. Dr. Milton Sims of Adelaide, South Australia, has reported amazing findings on the erosion of root surfaces caused by excess forces as delivered by headgear. I feel that as more is known about this, and as more orthodontists begin to respect mesial migration and appreciate the true normal occlusion for man, the use of extraoral force will diminish.
With light wire, we know from experience that no matter how much a tooth is tipped, the force is so light and physiologic that the cortical plates may be remodeled or bent, but never penetrated . Incidentally, we never have seen a tooth devitalized from tipping. In over twenty years of experience with the Begg Technique, I have never felt the need for headgear and I would not hesitate to compare my results with anyone else's.
RAR When we did use headgear, before we started with the Begg Technique, we felt treatment was adequate. However, since using the Begg Technique and discarding the use of headgear, our results are equal to, if not better than, any we ever previously accomplished. For this reason we see no need in using headgear with the Begg Technique. Over the years, our results have been viewed by thousands of orthodontists, and apparently are very acceptable. Actually, we feel that our results might be jeopardized by the use of headgear.
PCK I am sure that if we didn't stick to Dr. Begg's principles--that is, if we employed intermaxillary elastics of more than 2 ounces (56 grams), used archwires with inadequate anchor bends (bite-opening bends), or began treatment with relatively soft archwires rather than from Australian ESP wire--then we would feel the need for extraoral force. But since we try to do everything properly, the results are satisfactory. I would say, even superior to those results I have seen achieved by the use of extraoral forces with the Begg Technique.
HGB Don't you feel that the use of headgear might affect your diagnosis in critical anchorage cases and that many extraction cases could become nonextraction cases?
PCK The immediate factors which determine whether a case requires the reduction of tooth mass are the arch length/tooth mass discrepancy, the anteroposterior relationship of the dental arches, and the patient's soft tissue profile. Of course, one must also appreciate the continuous tendency for teeth to migrate mesially and erupt vertically. Perhaps an extraction case could be "masked" for a while by trying to hold things back, expanding the arches, or permitting contact points to slip past one another. However, when extraoral forces are removed, expanded dental arches will collapse.
When teeth are not in normal contact with their neighbors, they will press against one another along root surfaces, destroying both hard tissue and soft periodontal tissue.
In short, if a tooth mass/arch length discrepancy exists at the end of treatment, the teeth will relapse. However, relapse is not inevitable. It is only inevitable in the face of improper treatment; which, of course, includes failure to reduce tooth mass when indicated. All tooth movements must be overdone to have stability, and it is often impossible to overtreat to the extent necessary, unless one reduces tooth substance when indicated.
HGB Since you mentioned relapse, what is your feeling on muscle imbalance and myofunctional therapy?
PAR It appears that myofunctional therapy is indicated in severe situations as soon as the child is able to understand the problem and cooperate with the therapist. Often the orthodontist can instruct the child in the proper way of swallowing, and this knowledge, coupled with changes in the relationships of teeth during orthodontic treatment, can correct the problem. Sometimes there is success, and sometimes there isn't.
RAR The history of tongue thrust therapy in our practice might be interesting. About fifteen years ago, we obtained a speech therapist to correct all tongue thrust problems among our patients. After about two years, we assessed his results and found that a percent of the patients he had taken care of were helped. However, there still remained a small percent that continued to tongue thrust.
Assessing our treatment before we employed the speech therapist, we found that most of the patients lost their tongue thrusts during orthodontic treatment, and we still had the same, small percentage that continued to thrust the tongue after orthodontic treatment. For this reason, we have more or less given up tongue thrust therapy among our patients. This is not to say that we do not advise the patient, and explain the proper method of swallowing. We do this, and try to work along with them throughout treatment.
We have had some success in treating open bite cases by having the patients wear very light elastics between lingual hooks on the upper and lower lateral incisors. The elastics exert practically no vertical forces, functioning mainly to prevent the tongue from thrusting between the teeth. We are not using the elastics to close the bite, but rather as a barricade to block the tongue (Fig. 6).
HGB Let's give some attention to diagnosis and treatment planning. What is your opinion of computerized cephalometrics as a routine diagnostic aid?
RTR We don't use computerized cephalometrics. We do have our office personnel trace our cephalometric head-plates, and we use the tracing as an adjunct in our diagnostic procedures. For me, a cephalogram is just about equal in importance to the photograph of the patient, or the model.RAR We use cephalometrics as a diagnostic aid. However, our best judgment comes from looking at welldefined models, and a good profile photograph .
HGB What are your diagnostic criteria for nonextraction treatment
RAR The curve of Spee in the lower arch has to be considered. If we are going to reduce overbite, and level the occlusal plane, the lower anteriors will be moved forward. Pogonion has to be considered. If a patient has a prominent pogonion and a large nose, we would hesitate to extract teeth, as this might result in a more concave profile. I think, generally, low angle cases would lend themselves to nonextraction as well as Class II, division 2 type cases. This judgment would need to be tempered with stability of result, and the facial profile in the finished case.
PCK In our diagnosis we never consider the distal movement of teeth as a solution for arch length/tooth mass discrepancies or mesiodistal interarch discrepancies.
HGB When you do treat by nonextraction, how much expansion do you allow in the canine and molar areas?
RTR I try not to expand cuspids in the average case. The same goes with molars. Experience has shown that there would be a great tendency for relapse.
HGB When you feel that extraction is indicated, do you have a preference as to which teeth you would like to remove?
PCK We generally prefer to remove the first bicuspids because we feel that the second bicuspid has much better relationship to the first molar than a first bicuspid; and also, with differential forces we can move posterior teeth forward, if need be.
RTR The mechanics of the appliance itself is not a consideration in the choice of what teeth to extract. Through the application of differential forces we are able to easily close space at any location in the arch. The frictionless, one-point contacts between the archwires and the brackets also facilitate tooth movement. The Begg appliance itself does not dictate whether to extract or not, or which teeth to remove. That decision is based on the tooth mass/arch length discrepancy, interarch relationship, condition of individual teeth, profile, and of course, individual preference of the orthodontist.
HGB Would you consider removing second bicuspids or other teeth because of caries, or poor anatomy?
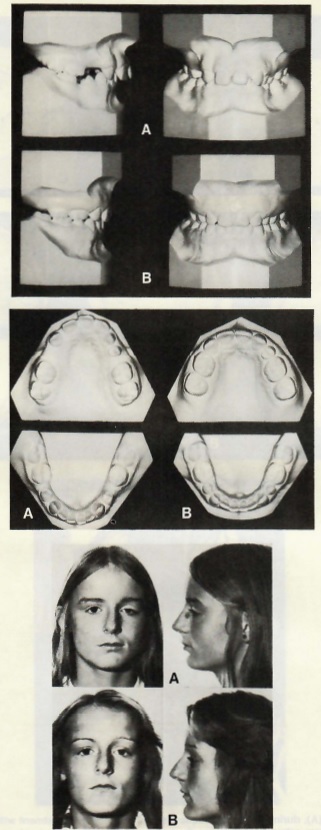
PCK If a first molar were deformed, or carious, and there was an arch length/tooth mass discrepancy, its removal should be considered rather than a sound tooth. That thinking would apply to any tooth--a lower anterior rather than a bicuspid. There are few limitations with the Begg Technique when considering the closing of spaces in any quadrant. One can move a molar to a cuspid position, if necessary (Fig. 7).
RAR With varied tooth extractions, I think it is very important that a diagnostic setup be made first, to permit 3D visualization of the final occlusion.
HGB What are your criteria for removing eight teeth as part of treatment?
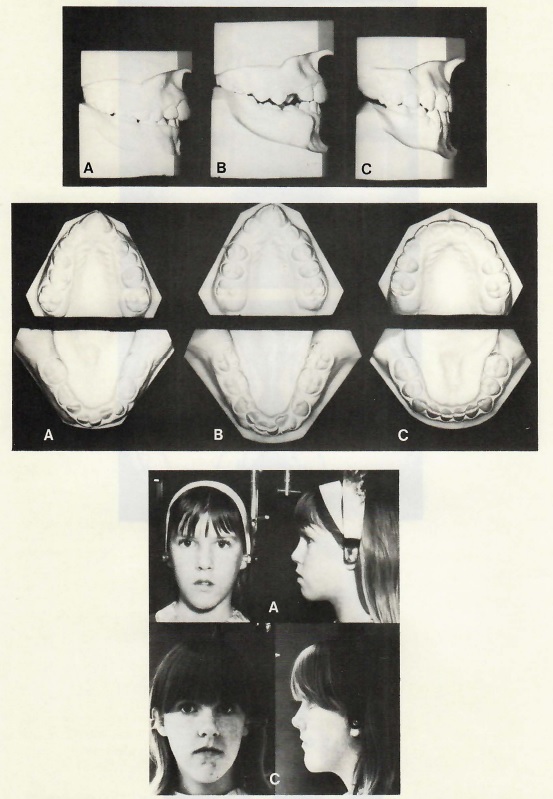
PCK The combination of factors creating the "Eight Tooth Syndrome" would include severe crowding of the upper and lower teeth, Class II molar relationship, dental arches forward off basal bone, prominent lips, and an FMA of 35 degrees or more. Probably the toughest part of treating an eight-tooth extraction case is making the diagnosis. If possible, it is advantageous if the extractions can be "timed" (Fig. 8). For most Class I and Class II eight-tooth extraction cases the preferred order would be to extract the first permanent molars just as the second permanent molars begin to erupt. When the second molars have erupted, the space remaining from the extraction of the first molars will be approximately half-gone. At that point the first premolars are removed and treatment begun.
HGB With so much space to be closed, do you make any special technical changes in appliance manipulation?
PCK The only appliance changes suggested for the treatment of eight-tooth extraction cases would be the use of oval buccal tubes and doubleback archwires for increased molar control.
HGB Not infrequently we hear a case described as having a "good lower arch" and teeth are removed only in the maxillary arch. What are your thoughts about single arch extraction?
PCK Usually, if a person has a tooth mass/arch length discrepancy in one arch, he or she will have it in the other arch. Therefore, those good lower arches may not be so good a few years down the line.
RTR When patients have been transferred to our office, in whom upperfirst bicuspids only were extracted, they subsequently developed lower anterior crowding. Also, single arch extraction usually does not permit the most favorable posterior occlusion.
HGB Do you object to leaving molars in a Class II position posttreatment?
PCK We object to the reasoning that has created the Class II occlusion, not the occlusion itself.
HGB Why?
PCK Because the vast majority of patients exhibit arch length/tooth mass discrepancies in both arches. An individual must have an excess of tooth substance in both arches to survive on a coarse, gritty diet; which, of course, is why we and our patients inherit teeth that are seemingly too large for our jaws. It is an inherited trait linked to survival, and explained in Dr. Begg's writings on attritional occlusion. Orthodontics as a whole, and patients in particular, would be much better off if all orthodontists understood the processes of mesial migration and vertical eruption, and realized that these phenomena persist throughout life even in the absence of tooth attrition. Show me a patient out of retention, who was treated with the removal of teeth in the upper arch only (either to alleviate crowding, or reduce an overjet), and I will show you a patient either with spaces in the upper arch, an overjet, crowded lower anteriors, or impacted lower third molars.
HGB Does your group assign the cephalogram a specific role in helping you determine extraction needs?
RTR We have for the past ten or fifteen years used the APO line as a criterion for deciding where to put the lower incisors. This follows the work of Raleigh Williams, who showed that the angular inclination of the lower incisor is not as important as its linear anteroposterior relationship in determining good facial esthetics. Therefore, we try to position the incisal edge of the lower incisor on, or close to, the AP line. We also use other angular and linear measurements as an aid in diagnosis, including SNA, SNB, ANB, FMA and upper incisor to SN.
HGB What do you feel is the role of soft tissue in deciding the need for extractions?
RAR In assessing whether or not a case is going to be an extraction case, we always take into consideration the soft tissue profile. If an individual has a prominent nose and/or chin, with the possibility that either or both may continue to grow, we would hesitate to extract teeth and flatten the face. In this type of case we would settle for anteriors that are tipped forward some, particularly the lower anterior teeth, and admit the possibility of some relapse of lower anterior teeth over a period of time.
HGB Today the literature is full of orthognathic surgery. Does it play an important part in treatment planning?
PCK To date the only surgery we have been involved with has been the reduction of prominent mandibles.
RTR If a case exhibits an extreme skeletal discrepancy, and we feel that the case is too severe to treat by orthodontics alone, we would consider surgery. Surgery should not only improve the treatment result, but also reduce the treatment time.
PCK If a patient has had proper orthodontic treatment (including the reduction of tooth substance when indicated), and has relapsed into an open bite, a Class III malocclusion, or even a severe Class II, one would have to think of surgery .In general, patients presenting to our office are thinking of orthodontic treatment. We, therefore, consider first the possibility of treating those patients solely from the orthodontic approach. It is amazing what can be done utilizing the Begg Technique on cases that others might think would require surgery. Time and time again, we have seen Class III and open bites treated without surgery, just by following the Begg Technique.
HGB When you do resort to a surgical procedure, do you maintain control of the case?
PAR I think it is important that the orthodontist control the case from beginning to end. He will be dealing with the patient for the most part, and this includes making any modifications in the diagnostic material or models, and constructing the splints. We feel that the orthodontist is more qualified to do this than the surgeon.
RTR I think it is important from the start, that the orthodontist and the surgeon get together and discuss the case. In my surgical cases, I have made the diagnosis and performed a certain amount of orthodontic treatment before surgery. I then made splints to facilitate proper placement of the jaws during the surgical procedure. Prior to treatment, we did a complete diagnostic workup on the models, cephs, and photographs, to determine the surgical treatment goals.
HGB I infer from what you are saying that you incorporate preorthodontic treatment in your surgical orthodontic cases. Is that so?
PCK Yes, we usually place the appliances on both the upper and lower dental arches. Teeth are aligned in each arch, reducing tooth substance as necessary. The dental arches are leveled, and arch forms developed that can be related to each other properly during surgery, with or without the aid of a splint. Of course, whenever possible, overcorrection should be practiced by the surgeon for the same reason it is a vital part of all orthodontic change--to minimize the effects of relapse. After the surgeon has done his work the fixed appliances are again used to bring the teeth into the best relationship possible (Fig. 9). In our practice surgery is just a massive "jolt" to the occlusion that occurs at some point during our fixed appliance therapy. It is our responsibility to prepare the dental arches orthodontically for surgery, and then to orthodontically finish and retain the case. Surgery is merely an adjunct to orthodontics, not a substitute.
HGB Good postoperative stabilization of the fragments is essential. Do you find the Begg appliance stable enough for this purpose
RTR Yes. However, we would advise that round archwires not be used when the surgery is being stabilized. It is suggested that .019X.026 or .0215X.027 archwires be bent in the ribbon arch plane and placed in the vertical slots of the brackets. Hooks or lugs can then be soldered to the archwire to facilitate placement of elastics, or Super High Hat pins could be used as engagement points.
HGB What about rhinoplasty or genioplasty?
RTR Yes. When indicated, rhinoplasty can even seem to change lip contour and prominence.
HGB In those cases where diagnostic decision is difficult, how do you plan treatment in the "borderline" extraction case
PCK A "borderline" extraction case suggests one can go either way--extraction, or nonextraction. The degree of crowding present at the "borderline" level would vary from practice to practice. Because of our appreciation of the processes of continual tooth eruption and mesial migration, our "borderline" cases would probably be below average; that is, most orthodontists would probably be considering cases with more arch length/tooth mass discrepancies as being borderline. The point here is that each of us has a different concept of a "borderline" case, depending on his or her particular training and treatment goals. I feel there is a degree of increased stability inherent in extraction cases. Also, we know we can bring the entire upper and lower dentition forward by extending Stage III with uprighting springs and lingual root-torquing auxiliaries. A true "borderline" extraction case would be an indication for mesiodistal stripping of selected teeth. This would be an even more favorable approach to treatment than either extraction or nonextraction.
RAR On occasion, cases will be started with the understanding that should progress not be satisfactory via the nonextraction route, extraction would be necessary. In cases such as this, the archwire is always stopped mesial to the molar tube, to prevent crowding of the bicuspid teeth. Also, in some borderline cases where there is minor crowding of the lower anterior teeth, they are all brought into good alignment, then stripped to reduce their mesiodistal widths. We do not consciously try to expand, either in the molar areas or the cuspid areas, to avoid extracting teeth. Of course, there is the occasional case with extreme lower anterior crowding and extremely narrow intercuspid width. The cuspids may be tipped distally into the bicuspid extraction space, which necessarily would increase the intercuspid width. In general, if the cuspid width and molar width have to be expanded to accommodate all teeth, we feel it would be an extraction case. However, this does not apply to crossbites, where palatal expansion can be used.