JCO Interviews Dr. Brainerd F. Swain on Current Appliance Therapy
DR. BRANDT Barney, you were the originator of the Siamese bracket. How did that come about?
DR. SWAIN Well, I came out with it in 1949 after several years of experimenting with what was then a relatively new problem in orthodontics, namely, paralleling roots when closing extraction spaces. Let me explain that.
Up until the late 1930's, orthodontists were dominated by Angle's dictum that proper treatment required a "full complement of teeth". In other words, orthodontic treatment meant nonextraction treatment for all, except perhaps cases of severe crowding. There was a stigma surrounding extraction treatment. In those days, the single bracket, used with a full-sized wire that had the proper bends, was adequate to produce the three orders of tooth movement required with Angle's nonextraction treatment. Then Tweed came along and changed all that. He did it in the following manner. He recalled 150 of his treated nonextraction patients whose teeth and faces he didn't like, and had four bicuspids removed. He retreated them (without charge, incidentally) and then compared the results of each treatment. The improvement resulting from extraction treatment was so dramatic and compelling that, for most of us who practiced in that era, Tweed--by this one stroke alone--cut the Gordian knot and made extraction treatment acceptable.
However, closing extraction spaces meant moving teeth further, and orthodontists soon had difficulty obtaining root parallelism when doing so. A lot of experimenting was done, including changes in the archwire, in the positioning of brackets, and in the size and shape of the bracket itself. For example, one ingenious archwire designed for paralleling was the gable roof arch invented by Dr. Harry Bull and still in use today. It included a loop and not only paralleled the roots, but maintained the crowns in contact while doing so.
In an effort to "build treatment into the brackets" and reduce or eliminate bends in the archwire, orthodontists began to place brackets in positions that would offset the tendency of the roots to fall behind during space closure, and also to compensate for some undesirable rotations occurring at the same time. We came to realize that when closing an extraction space, the teeth on either side of the space tend to tip and to rotate toward it. From this it was a simple step in the middle 1940's to devise what I called a double offset technic, namely, placing brackets (these were molar or double width brackets) on either side of the extraction space to offset undesired rotation and tipping. Then we found it could be made more efficient, if short lengths of .030 or .040 wire were soldered on the bands beside the brackets, either vertically or horizontally. The archwire rested against these when tied into the bracket slot. They had the effect of increasing the distance between the bearing points of the archwire, and that in turn permitted reducing the amount of offset in bracket positioning. When these spurs or cleats were soldered on (most of us used gold in those days), they acted like two walls of a bracket, so the obvious next step for many of us was simply to solder on another bracket, particularly on molars. This introduced problems in getting the brackets properly alined, especially on the curved surfaces of bicuspids and cuspids, and that led to my placing the two brackets on a common base in order to assure alinement and facilitate attachment. Incidentally, as a matter of interest in these times of high gold prices, the first Siamese Twin brackets were milled out of solid bar stock, and this meant a lot of gold dust lost in the process.
DR. BRANDT Why did you call it the Siamese bracket?
DR. SWAIN Well, actually I call it the Siamese Twin bracket because of the famous circus twins from Siam, who were joined together near the waist by a connecting tissue link. The analogy of two brackets also joined at the waist by a connecting strip seemed logical enough, hence the Siamese Twin bracket.
DR. BRANDT Have there been many refinements in the bracket since then?
DR. SWAIN Yes, many. Probably the most important are those that extend the principle of "building treatment into the bracket": such as tip, torque, rotation, and the in/out feature, or variation in labiolingual thickness of certain brackets, which reduces or eliminates inset or outset bends in the archwire. In addition, the tie wings are taller and have been reshaped. The incisal wing of lower incisor brackets has been chamfered to reduce occlusal interference. The gingival tie wing, on the other hand, has been extended out labially, in order to improve access when ligating. Also, the tie wing grooves are now deeper, and that helps in ligating or placing elastomeric thread or chain. Accuracy in bracket placement got a boost when the edgewise slot was placed at an angle to the sides of the bracket, so that when these sides are placed parallel to the sides of the crown, then the edgewise slot will have the right amount of tip.
These changes are all helpful, but probably require a word of caution, which is that where the original bracket was symmetrical from top to bottom and side to side, and the slot was parallel with the upper and lower edges, the current brackets are so modified and so variable in shape that it is important to keep in mind that the "bottom line" in bracket placement is the position of the slot Don't let your eye be diverted by the orientation of other parts or by curved mesial and distal surfaces or visual reference lines such as incisal edges. As Williamson puts it, "When you think of placing brackets, think of placing slots".
DR. BRANDT How important is the placement of Siamese brackets in Straight Wire technic?
DR. SWAIN Sid, before answering that, may I repeat a point that has been emphasized by Andrews and Roth, namely, that Straight Wire means an appliance, not a technic. Anybody's edgewise technic can be used with the Straight Wire appliance. I use Roth's technic and his new hookup, which was brought out in the fall of 1979. These brackets, which contain a new prescription for the amount and direction of tip, torque and rotation force, are designed to provide not only for correction but for overcorrection, which is Roth's "End of Appliance Therapy Goal". If you believe in overcorrecting, and I have for a long time, then with all that good stuff built into those brackets, placing them accurately is just more important and more rewarding than ever before.
DR. BRANDT Is bracket placement any more significant to Siamese brackets than others?
DR. SWAIN Yes. If you insert a wire that fills the slot on single, double width, and Siamese Twin brackets, there will be greater control over the positioning of the crown and root. Logically, the more accurate your bracket placement, the more accurate your leveling, alinement and rotation. That's an advantage, not a handicap.
DR. BRANDT What is your feeling about the importance of interbracket distance?
DR. SWAIN Sid, interbracket distance is probably more important with treatment mechanics that require archwire bends between brackets and where ample space is needed for them. Interbracket space is much less important with a technic such as Ron Roth's, where you start out with either looped or plain light wire arches and gradually level up to heavier flat archwires. Roth's bracket prescription and recommendations for bracket placement build treatment, and indeed overtreatment, into the brackets, so that, ideally, the objective is to produce all required final detailing movements with a flat archwire. While that can be difficult, because errors of bracket placement, or occasional variations in facial surfaces that affect placement may require some compensatory archwire bends, the interspace between the Siamese Twin brackets is still ample.
Another factor that effectively reduces the need for wide interbracket space has been the introduction of newer wires such as Nitinol and D-Rect, with their high resiliency and low load/deflection rates. For example, when alining irregular anterior teeth and when there is little interbracket space, these wires can be deflected considerably while ligating and yet not distort in the process. Furthermore, they exert a light but relatively constant force. Even when crowding and irregularity are severe and a looped archwire is used, if lack of interbracket space is a slight problem while ligating, this clears up after one or two appointments. From that point on throughout treatment, interbracket space is of little concern, except perhaps after finishing space closure and other major tooth movements, and when preparing for final detailing. At that time, I relocate or replace brackets that aren't positioned accurately, because although the brackets may look good at the outset of treatment when the teeth are rotated and irregular, they often show need for improvement when commencing final detailing. After relocating, brackets are often at a different level from those mesial or distal, and it's usually necessary for one or two appointments to drop back to a lighter archwire, such as Nitinol or D-Rect, in order to be in the slot while leveling. Also, these wires are easier on the patient, and usually after one or two appointments a full-sized archwire can be put in again.
DR. BRANDT When placing brackets, do you place them at the center of the crown or at some measured distance from the incisal edge or buccal cusp?
DR. SWAIN I've done it both ways. In fact, I've switched back and forth several times. Angle and his students, such as Strang, from whom I took my first Edgewise course, used the middle third of the crown, so that's how I started out. Several years later, while at a Tweed Foundation meeting, I heard about the use of a bracket gauge, and shortly after, at the recommendation of Dr. Harry Bull, who invented the Bull loop and the gable roof arch, I standardized on bracket height, using a measuring gauge and keying on the second bicuspid crown, which, as he'd noted, usually has the shortest crown. I continued with this for both Edgewise and Light Wire strapups until I went into Straight Wire in 1976, and my first dozen cases had indirect bands done by "A" Company, with the brackets located in the middle third of the crowns. That, of course, was where they were designed to be, but revived some old problems such as the strong reverse curves needed for overbite correction and some undesirable torque effects I hadn't seen for a while. Since then, I've gotten back to the practice of measuring for bracket placement. Measurement is made from the incisal edge or tip of the buccal cusp to the edgewise slot. If either the slot or incisal edge is tipped, I usually key on the slot at the mesial half of the bracket. In both arches, the incisors, bicuspids and molars are set at 3½mm, except the upper second molar which is placed about 3mm. The lower cuspids are placed at 4 and the upper cuspids at 4½mm. These measurements may be increased slightly with large or tall crowns. If so, the same increase is used for each tooth.
DR. BRANDT Why do you place the upper second molar tube at 3mm?
DR. SWAIN The practice of banding upper second molars at age twelve or early in the teens, and then uprighting them into a full vertical adult position makes me uneasy. These recently erupted teeth are often tipped both distally and buccally. In this age group, I'm going back to a policy I used for many years (when soldering tubes on freehand), which was to place the upper second molar tube slightly occlusally in relation to the first molar attachment, close to the occlusal edge of the band and with the mesial end of the tube tipped up gingivally. This keeps the tooth slightly intruded and tipped back distally, and it eliminates the need for an upward bend in the archwire, such as usually placed in this region. In turn, that helps when placing the usual buccal root torque in these upper molars, because it can be placed in a relatively straight, flat wire. To explain that, if the tube is at the customary height and with the usual angulation, if buccal crown torque as well as an upward bend are placed in the archwire, this creates a compound curve and the wire spirals outward as well as upward.
It seems more in keeping with the concept of building treatment into the bracket and using a straight wire for treatment, if the upper second molar tube is placed more occlusally on the tooth as described, so as to produce slight intrusion and to maintain the distal inclination usual in this age group. Finally, this slightly intruded or undererupted position is an advantage from a functional standpoint, since the lingual cusp of the upper second molar is one of the most common causes of occlusal interference during excursive movements. Furthermore, a slight extrusion of this tooth, for example through failure to place enough of the usual upward or intrusive bend in the archwire to keep it slightly intruded, can create what Roth calls a molar "fulcrum" and that can lead to occlusion problems.
DR. BRANDT What does Roth mean by a molar "fulcrum"?
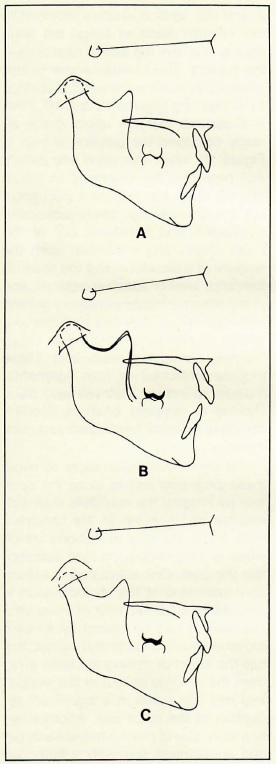
DR. SWAIN It refers to the effect on the occlusion or the temporomandibular joint when a molar is extruded or overrupted. The consequences of this are illustrated in Figure 1. Figure 1A is taken from the Broadbent-Bolton Atlas and represents the 12-year normal. Figure 1B shows the upper molar extruded 2mm by, for example, cervical headgear. The jaws have been forced apart, the axis of jaw rotation during closure is still at the condyle, but the anterior teeth are in open bite. Figure 1C shows a different consequence of the same extrusion. The teeth are together in centric occlusion, but the condyle is subluxated downward and backward, the axis of jaw rotation during final closure is at the extruded molar.
In the course of a panel discussion, Roth commented on the prevalence and significance of molar extrusion or fulcrumming in TMJ dysfunction problems: "I have not yet seen a TMJ case that has responded to occlusal therapy, in which there wasn't some degree of what I call a fulcrum, or rocking, or inferior displacement of the condyles at the time the mandible was placed in a stable position. This was a big revelation to me because initially, in my introduction to gnathology, a centric slide was a deflection off the arc of closure and the mandible came forward and off to the side a little bit. In my observations over the last 15 years, I would say the majority of TMJ cases I treat and that I see are more vertical problems than anteroposterior problems. There is a share of anteroposterior problems, but most of them are an inferior displacement of the condyle."
My experience with TMJ patients has been very limited, Sid, but as a teacher and practitioner I have a special interest in the significance of these observations on molar fulcrumming in orthodontics. I feel they should be of concern, because so much of what we do tends to extrude molars. For example, a simple thing such as bracket placement. Let's say that a molar band (usually a second, but possibly a first molar) is fitted too far to the gingival, so that the tooth is extruded. Let's also assume it is held in this position long enough for bone to fill in beneath the root, so that it is stabilized in this position. Will the intermittent forces of occlusion pound it back down again after debanding? Not likely. Anyone who's experienced the discomfort of a "high" filling knows that rarely happens. So, this molar fulcrum either results in an anterior open bite (Fig. 1B) or condylar subluxation (Fig. 1C) and, unless the discrepancy is sufficiently mild or some very helpful condylar growth and remodeling takes place, the patient may be predisposed to a TMJ problem because of a bracket placement error.
Cervical headgear on upper molars and Class II elastics on lower molars also can extrude these teeth. I realize that from the orthodontic viewpoint these mechanics have both defenders and critics. I'm suggesting that from a jaw relation and functional occlusion standpoint, their use should be reduced as much as possible or else avoided, especially among patients with a short ramus, short posterior face height, or anterior open bite.
DR. BRANDT In view of the hazard of creating a molar fulcrum, how should the orthodontist treat an open bite?
DR. SWAIN Sid, first let me say that the gnathologic approach to correction of an open bite is the same in principle, whether it's being accomplished by orthodontics, equilibration, occlusal restorations, surgery, or some combination of these four. That principle is to close the bite by hinging the mandible shut, with the axis of rotation being at the condyle. This is in contrast to conventional orthodontic mechanics, which use vertical elastics attached to the anterior teeth to hinge the teeth shut, and where the axis of rotation is at the molars. The consequences of this changed occlusion are again illustrated by comparing Figures 1B and 1C. First, let's assume that the upper molar already occupied the position shown in Figure 1B when this open bite patient first presented for treatment. In Figure 1C, the teeth are in centric occlusion, but the condyle has been subluxated downward and backward out of the fossa. Depending somewhat upon the amount of subluxation and the patient's tolerance level or adaptive capacity, and in the absence of compensatory growth and remodeling, this can give rise to a variety of problems, which may occur promptly or appear years later. These include stretched or torn ligaments, muscle splinting, stiffness and pain, clicking or popping, bruxism, accelerated enamel wear, headaches and neck aches.
If the orthodontist seeks to avoid these problems and to close the open bite by hinging the mandible shut with rotation taking place at the condyles, then there are several options which alone or in combination may accomplish the goal. One alternative is extraction treatment. If the malocclusion is sufficiently mild that most of the extraction spaces can be closed by forward movement of bicuspids and molars, this has the effect of pulling the teeth away from the condyle or "out of the wedge", and this can result in a significant reduction of the open bite. Another option would be to place a transpalatal bar and supplement this with a high pull headgear to the upper molars. With good cooperation this might result in 1 or 2mm of intrusion, and that can mean 3 or 4mm closure at the anterior teeth. It may not be possible to entirely close the open bite orthodontically, but if the cuspids can be brought into occlusal contact, this provides anterior guidance during function, which is important in avoiding TMJ problems.
Aside from orthodontic movement, there are other options such as equilibration, extraction of extruded teeth, rebuilding of occlusal surfaces, and surgery for more severe open bite problems, especially those with associated TMJ problems.
One additional word, Sid, on open bites. It's good practice to x-ray the anterior teeth after four to six months of treatment to check on root resorption. Open bite patients notoriously are prone to considerable root resorption during orthodontic treatment. This also should be discussed beforehand as one aspect of a full and fair disclosure of the possible consequences of treatment, when the orthodontist is seeking the patient's informed consent.
DR. BRANDT How does the gnathologist's goal for anterior guidance correlate with the orthodontist's goal of flattening the occlusal plane to obtain overbite correction? Doesn't that affect the incisal guidance?
DR. SWAIN Most orthodontists find it necessary to flatten the occlusal plane during overbite correction, especially in deep bite cases. At the end of appliance therapy, the curve of Spee is leveled and overbite overcorrected. At that point, when the patient goes through mandibular excursions, the anterior guidance will be not quite adequate, and it would not satisfy gnathological goals. However, as the orthodontist is well aware, overbite seldom remains overcorrected. Almost routinely after appliance removal, the curve of Spee gradually returns and overbite deepens somewhat. That improves the anterior guidance, so that during excursive movements it will meet gnathologic goals. An awareness of known postorthodontic relapse tendencies in this situation could avoid possible misunderstanding between the orthodontist and the referring dentist, since with the passage of time, and with no other input, the occlusion will improve and satisfy their mutual goals.
DR. BRANDT Do you believe that other appliances can be used to achieve gnathological goals?
DR. SWAIN Yes, I believe that while you could probably achieve gnathologic goals with other appliances, you'd have to work a lot harder than with Straight Wire. Keep in mind that a lot of the elements we need in terms of tooth position were built in to Andrews' sample of nonorthodontic normals. Since he measured this sample in order to build his appliance, it has in it a lot of the elements we need to get a good functional occlusion.
DR. BRANDT Are Andrew's Six Keys to Normal Occlusion useful to you in treatment.?
DR. SWAIN Yes. All Six Keys were common characteristics among his 120 normals, but relatively uncommon among the 1000-plus treated cases that he studied. To me this indicates that we had then, and I suspect still have (speaking for myself), a ways to go before we match the fine detailing reflected in these six characteristics. As a matter of personal interest, I have occasionally checked my own patients and found this can be a humbling experience. It's tough to make all six. Reopening of contacts at extraction spaces was the most common hangup for me.
DR. BRANDT Would you list the Six Keys for us?
DR. SWAIN The Six Keys are as follows:
1. Molar relationship. The distobuccal cusp of the upper first molar occludes with the mesiobuccal cusp of the lower second molar.
2. Crown angulation or tip. The gingival portion of the crown is distal to the incisal portion in most individuals.
3. Crown inclination or torque. Anterior crowns have an anterior inclination; posterior crowns have a lingual inclination.
4. Rotations. There are no rotations.
5. Spaces. There are no spaces; contacts are tight.
6. Occlusal plane. Varies between flat and a slight curve of Spee (1.5mm or less).
DR. BRANDT What's the concept behind the Straight Wire appliance? Does it actually mean a straight wire?
DR. SWAIN Yes, Straight Wire means a flat edgewise wire that fills the slot and has idealized arch form, but no other bends. The concept as I see it, is to provide (1) an individualized bracket at (2) a prescribed position on each tooth, so that (3) a straight wire can be used to finish treatment for 95% of patients.
Let me explain that statement as it applies to the Roth bracket setup and his mechanics:
(1) The individualized bracket used in this setup is designed to not only correct, but to overcorrect each tooth position after a straight wire is inserted and sufficient time allowed for full expression to take place. The rationale behind overcorrection is to acknowledge that teeth move aftert appliance removal, and therefore one should leave each tooth in such position before debanding that it will settle back into normal alinement and occlusion from the overcorrected position. The amount and direction of overcorrection built into these brackets is the result of 3 to 4 years of clinical trial and modification. As a long-time believer in overcorrection and its benefit to stability, Sid, I think this advance is an idea whose time has come and come to stay. I know that two manufacturers have either brought out or are working on their own versions of the new Roth setup.
(2) The prescribed position. Sid, I believe accurate bracket placement is a prime weakness among orthodontists, and I include myself in this group. Unfortunately, accurate placement is becoming more important as more and more treatment is built into the bracket. That wasn't always so. When Angle introduced his Edgewise appliance, there was one standard bracket and treatment was accomplished with bends in the archwire assisted by auxiliaries. Bracket placement deficiencies were compensated by altering the bends. However, with this new setup, the amount of treatment built in has reached its logical conclusion. The torque, tip, rotation, overcorrection and final detailing are all in the bracket provided three conditions are satisfied:
(a) a straight wire is placed,
(b) sufficient time is allowed for full expression of movement, and,
(c) the brackets are in the right place. If some are not, then bends will have to be placed and the simplicity and efficiency of treatment will be reduced proportionately.
(3) To finish treatment. I did not say and don't want to imply that a straight wire is used from start to finish. While that's been done, Roth's mechanics, like most others, use looped and plain round and edgewise wires, plus auxiliary wires and headgear to accomplish movements such as leveling, alining, rotating, retracting anteriors, closing extraction spaces, correcting Class II relationships and overbites. Once these are accomplished, the straight wire is placed for overcorrection and the final detailing which is Roth's "End of Appliance Therapy Goal."
DR. BRANDT Why does the upper cuspid have 13° of mesial tip?
DR. SWAIN In order for the upper cuspid to function properly, it has to have enough mesial tip so that when a patient with a Class I occlusion goes into a lateral excursion, the tip of the upper cuspid will function against the lower cuspid to give immediate separation or, disclusion of the posterior teeth. Now, if the buccal segments are in Class I and the upper cuspid has little or no mesial angulation, the incisal tip will pass through the embrasure between the lower cuspid and bicuspid and there will be no cuspid rise. If there's no cuspid rise, there will be cuspal interferences on both the working and nonworking sides and that often leads to bruxing, which adversely affects postorthodontic stability. From the standpoint of functional occlusion, there may be harmful consequences of this occlusal interference, including occlusal wear, periodontal disease (where local or systemic predisposing factors are present) and temporomandibular joint dysfunction.
Now, having said that, I have to add that I'm a little uneasy with the 13° tip on the upper cuspid bracket, because of the amount of tipping of roots in finished cases. I have a good panoramic x-ray, one that provides an uninterrupted and continuous scan from third molar to third molar. When I take an x-ray following treatment, I can see how every root relates to every other root, upper and lower as well as right and left. Far too often, I see the cuspid roots, particularly the upper, too far back and too close to the bicuspids. Of course, that's no surprise, because if the bicuspid bracket has 0° tip and the cuspid bracket has 13°, even though allowance is made for differences in the root/crown axis of each tooth, those roots are going to be pretty close. I know that sufficient mesial tip of the cuspids is important from the standpoint of functional movements, but I'm concerned that 13° might just be a couple of degrees too far.
DR. BRANDT How is the new Roth setup working out for you?
DR. SWAIN Well, it's a bit early to be able to talk from experience, but I had seen the prototype brackets undergoing trial in Roth's office, and liked what I saw. I haven't finished any cases with the new setup, but expect it will provide the degree of overcorrection he seeks as his "End of Appliance Therapy Goal' and will do that with a full-sized archwire containing few bends or, hopefully, none. I also like the bracket placement he is now using with the setup, in part because it's so close to what I was using with Edgewise years ago.
Three changes in the buccal segments are particularly important: (1) the upper bicuspids and molars are tipped back slightly to 0°; the lower bicuspids and molars are tipped back slightly more to -1°. That helps with anchorage control and has other benefits; (2), built-in upper buccal root torque has been increased and is now progressive torque, upper bicuspids are -7° and molars are -14°. That saves a lot of wire bending; and (3), the upper first and second molars now have 14° rotation. This will overrotate these teeth and that will mean better occlusion in the buccal segments.
DR. BRANDT Did you say that overrotation of the upper first molar often aids Class I interdigitation in the buccal segments?
DR. SWAIN Yes. For many years, when molar tubes were soldered on freehand, I made it a policy to overrotate upper first molars, and did this by offsetting the molar tubes at the distal and using the following guide: Bend a short piece of edgewise wire so that if forms two legs that meet at a right angle. Using a model of the upper teeth, place one leg tangent to the mesial surface of the upper first molar and the other leg extending back along the buccal surface. This leg will touch near the center of the mesiobuccal cusp and will form an "offset" angle with the buccal surface, usually ranging between 12° and 15°. That's kind of interesting, because the new Roth bracket is 14°. Now, if the tube is on the band at this angle and a straight wire inserted, it will overrotate the upper molar slightly, and that has a beneficial effect on occlusion, because the mesiolingual cusp, which fits into the central fossa of the lower first molar, is moved forward by this rotation. In turn, patients usually bite forward slightly, since the lower molar will fit better with the mesiolingual cusp of the upper at that point, and most of us "tend to bite where our teeth fit best". The lower second molar also occludes further forward, and the distobuccal cusp of the upper molar can more easily settle down and back against the lower second molar in Andrews' key position. In addition, the tip of the upper second bicuspid tucks neatly into the interspace between the lower second bicuspid and first molar, and that intercuspation is hard to achieve with inadequate molar rotation.
Overrotation of upper first molars is also helpful where stubborn midline problems or cusp-to-cusp relationships in the buccal segments seem to be responding slowly to treatment. From my experience with the Straight Wire appliance in the past three years, I wasn't seeing enough overrotation of molars with the brackets and bands as they were supplied. While this could be remedied with a toe-in bend in the archwire, then it is difficult to engage the upper second molar. However, with the increased rotation (14°) available in the new Roth upper molar brackets, I expect to again see some of the improved intercuspation that occurs when these teeth are overrotated.
DR. BRANDT Does the Straight Wire appliance require a broader arch form?
DR. SWAIN I don't know that it requires a broader arch form, but it was certainly designed for one. Andrews uses an arch form with the Straight Wire appliance obtained from measuring his 120 untreated normals. Roth's arch form, the Tru-Arch, is based on observation of occlusal contacts and functional movement patterns, posttreatment settling, and long term stability. Roth's arch form is somewhat broader than Andrews'. Another broad arch form, the Penta-Morphic form, was brought out by Ricketts in 1979. It was formulated from his research on normal occlusions, successfully treated cases, and computer analysis of frontal, labial and vertical coordinate data. Incidentally, Roth's Tru-Arch form and the "normal" form in Ricketts' series are just about identical except at the second molars, where Roth's curves slightly to the lingual.
For orthodontists brought up to the Bonwill-Hawley form, or who believe that, insofar as possible, the arch form of the malocclusion should be retained in treatment, these newer arches are clearly broader. However, in each instance they are biologically based rather than, as in the case of the Bonwill-Hawley chart, derived geometrically. Hopefully this will lead to greater posttreatment stability.
DR. BRANDT What is unique about Roth's "End of Appliance Therapy Goal"?
DR. SWAIN It refers to his goal for positions teeth are to occupy when fixed appliances are removed at the end of treatment. He believes that they should be overcorrected, in order to allow for the anticipated posttreatment settling or rebound or relapse or whatever you choose to call it. Now although overcorrection as a treatment strategy isn't new, I don't recall any previous recommendation that it be done in all three planes of space in anticipation of relapse in all three areas. And, I don't know anyone who has gone so far as to build that overcorrection into his brackets.
DR. BRANDT Do you foresee doing an entire treatment with a single straight wire for each arch?
DR. SWAIN Not right now, but continuing bracket modifications and improved physical properties of wires are bringing us closer. These new brackets, which have not only treatment but overtreatment built in, would probably serve, if given an archwire whose physical properties could be changed during treatment. At the outset of treatment it should have high flexibility or low stiffness, high resilience, and a low load/deflection or low spring rate. Nitinol (edgewise), for example, has these properties and it certainly simplifies the alining, leveling and rotating usually required at the beginning of treatment. However, when treatment gets into correcting overbite and overjet, closing spaces and paralleling roots, establishing arch form, width and symmetry, these require higher stiffness, while high resilience and a low spring rate are less important.
DR. BRANDT Barney, when you were in Light Wire, it was said that you never did pure Begg, because you used the "chicken" bracket. What is the "chicken" bracket?
DR. SWAIN Sid, that refers to the combination bracket which provides for a free-pivoting gingival slot and also has an edgewise slot. Years ago, to use something like that, or in fact anything but a "pure Begg" bracket, was regarded as "chicken". Recently, however, there's been more interest among light wire practitioners in combination brackets that do have an edgewise slot.
DR. BRANDT How do you feel about the current interest among Light Wire practitioners in these brackets with pretorqued and preangulated slots?
DR. SWAIN The idea is to use the gingival slot for the usual three stages of Begg technic, and then go into a fourth stage, using the edgewise slot for more precise final detailing. One of the manufacturers recently brought out such a "Four Stage Bracket". It looks interesting, but from my own experience with the "chicken" bracket, I know that to make that edgewise slot work efficiently without a lot of wire bending, it's going to require really accurate bracket placement Anyway, I respect their attitude and interest and hope something comes from it, as there seem to be some interesting possibilities. For example, one would be to place short segments of Nitinol edgewise wire in the edgewise slots of cuspids and bicuspids during Third Stage paralleling. As already noted, this wire has such high resiliency and such a low deflection rate that a full arch might serve for the leveling, aligning, and rotating required in the Fourth Stage detailing.
DR. BRANDT Barney, you've always cautioned your students or listeners against the unilateral Class II problem. Would you care to comment?
DR. SWAIN Sid, I believe you're referring to my statement that a unilateral Class II malocclusion may be a tooth discrepancy case in disguise, and to be very careful in planning treatment. For example, assume that a patient with a full Class II molar relationship on one side and Class I on the other presents for treatment. Overbite and overjet are moderate (3 to 4mm) and there is no crowding and no spacing. Given those six conditions, this has to be a tooth-size paradox. Measurement and comparison of the upper and lower tooth widths in this case will usually show an unfavorably high Bolton tooth-size ratio, probably 80% or above. Now, if models are made and a diagnostic setup done with molars on both sides placed in Class I, there will not be room enough for the upper anteriors to enclose the lowers properly.. Either an edge-to-edge bite or very slight overbite (1 to 2mm) will result. So, if the patient is treated and the Class I molar relationship holds, but the edge-to-edge or slight overbite relationship does not, then the lower anterior teeth will probably crowd up as overbite deepens, and the orthodontist is in a difficult spot explaining those crooked teeth, because that's not just relapse. It's much worse than that. You have to explain, if you can, why those lower front teeth are crooked after you treated them, when they were straight before you did so.
Treatment planning requires some kind of compensation, such as stripping or reproximation, or else extraction of a lower incisor, to reduce the discrepancy enough to permit a realistically deeper overbite and overjet, while still maintaining the Class I relationship on both sides. The diagnostic setup is the best means for deciding between these alternative compensations, because it's a three-dimensional resolution of a three-dimensional problem.
DR. BRANDT Are Class II elastics an integral part of your mechanics?
DR. SWAIN Yes, they are an integral part, but that doesn't mean that they're used steadily throughout treatment. In fact, I prefer to avoid them whenever possible, except perhaps in the skeletal deep bite case, for example, where some lower molar extrusion with Class II elastic force would be of help with overbite correction. As a general rule, I prefer to rely on headgear force attached directly to anterior teeth for purposes of retraction, unless Class II elastics at this time would be of help for intentional forward movement of lower molars.
The Class II elastics are of two types, the short Class II and the conventional or long Class II. The short Class II is attached from a power arm or loop in the upper cuspid area and extends to the power arm on the lower second bicuspid. In a nonextraction case, it might hook onto the lower first bicuspid, and another short Class II might be attached from the upper first bicuspid to the lower second bicuspid. The action of these elastics initially seems somewhat like a paradox, but is understandable. Since they stretch in a more vertical than horizontal plane, the initial reaction is to suspect that it would bring about quite a bit of extrusion among the lower teeth. However, it should be recognized that the lower arch normally contains a heavy wire with a reverse curve, which ordinarily tends to extrude bicuspids and hold molars and incisors down during flattening of the occlusal plane. Cephalometric records taken before and after the use of short Class II elastics indicate that there is little or no lower molar extrusion or tipping of the occlusal plane, certainly less than that which frequently occurs with conventional or long Class II elastics stretched from the upper cuspid area to the lower first molar. While this is an advantage with the short Class II elastics, there is a disadvantage that occasionally arises, namely, insufficient correction in the buccal occlusion, and that requires conventional Class II force to bring about.
DR. BRANDT You mentioned headgear for retraction of anteriors. Do you retract all six anteriors simultaneously, or do you retract cuspids and then go back for the incisors?
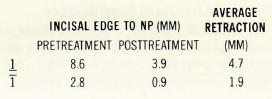
DR. SWAIN I retract all the anteriors simultaneously, Frankly, that worried me back in 1976 when I started with Straight Wire, because for the fourteen years I had used Edgewise in the 1940's and '50's, retracting six anteriors at once was almost universally regarded as a great way to blow your anchorage and end up with everything too far forward in the mouth. However, Andrews and Roth were doing it routinely, and despite misgivings based on my earlier experience, I did also. It seems to work, and when I checked a hundred finished cases recently. I came up with the following:
DR. BRANDT How do you correct the Class II relationship in a nonextraction case?
DR. SWAIN Through many years of both Edgewise and Light Wire technic, I've generally preferred to correct the Class II relationship during the mixed dentition wherever possible. In the permanent dentition, after growth is pretty well completed, correction of a Class II relationship without extracting teeth would be unusual, unless the problem was quite mild and spacing is present in the buccal segments so as to permit correction by tooth movement rather than jaw movement. In severe problems, such as skeletal Class II with an open bite, where the use of Class II elastics might result in lower molar extrusion and aggravate the open bite, I may extract only in the upper arch, retract the upper anteriors, and leave the buccal segments in Class II. These patients usually have a short posterior face height, and it's important to stay away from Class II elastics or other mechanics that might subluxate the mandible and create TMJ symptoms for the patient.
DR. BRANDT Barney, orthodontists and other dentists have been at loggerheads regarding occlusion for a long time. Do you see any signs of reconciliation of their views?
DR. SWAIN Yes, Sid. Occlusion problems, by their very nature are complex, and solutions more often than not require the services and knowledge of people with skills in more than one area of practice. Small multidisciplinary study groups made up of dentists in various practice areas can help. In addition, continuing education courses given by orthodontists and restorative dentists, for example, and intended for both orthodontists and restorative dentists, can be superb. I think perhaps the best opportunity is at the community level, where the orthodontist and the restorative dentist collaborate in the diagnosis and planning and then in the ongoing treatment of patients with occlusion problems. This kind of relationship is a special challenge to an orthodontist working with a younger practitioner whose educational background included training in functional occlusion concepts and goals.