JCO Interviews Dr. Charles J. Burstone on the Uses of the Computer in Orthodontic Practice, Part 2
JCO Now, will you demonstrate how you make and use the occlusogram?
DR. BURSTONE Digitizing the points of the 1:1 occlusal photograph of the model gives us both measurements and a diagram of the tooth positions (Fig. 4). While we are talking, out came a printout of tooth size discrepancy. The computer does a setup.
JCO Do you relate this to overbite?
DR. BURSTONE Oh, yes. This is a real tooth size discrepancy analysis since a setup is done by the computer. A Bolton analysis, by contrast, is only a screening mechanism.
JCO Are your tooth size means from the same Denver sample?
DR. BURSTONE This is from Moorrees' work.
JCO What points do you digitize?
DR. BURSTONE Points are digitized at the mesial and distal contacts and the tips of the buccal cusps of the lower, and the functional cusps on the upper will be the tips of the lingual cusps. The computer draws the teeth. These are schematic representations of the upper and lower teeth.
The computer calculates the variations from the mean in tooth size. The reason for seeing this on the screen at this time is to find out if there are major tooth size differences. This is used if we want to make a decision on extraction, or to point out a mistake in digitizing. Later, we will actually set up the teeth on the computer to see how they are going to fit.
Now, the first question the computer asks is if the right molar should be moved so that we can determine the geometric midline. There are other determinants of the midline, including what looks good for the face and also if there is any skeletal discrepancy anteriorly. The geometric midline is a point right in the center of the arch if we like the relative positions of the posterior teeth on the right and left sides. The first judgment I want to make in treatment planning is if I think that the two posterior segments are symmetrical to each other.
So, the computer asks if you would like to move one buccal segment back in respect to the other, just to equalize their axial inclination or their position. It will then calculate where the center of the arch is--the geometric midline.
JCO You use a soft tissue point, the median palatal raphe?
DR. BURSTONE That's just an arbitrary point, only used for reference. We definitely do not use it for a treatment midline.
Next, to determine where the midline should be on the patient, we use all our knowledge as an orthodontist. We consider the facial midline based on esthetic considerations, anterior apical base discrepancies, and the geometric midline which we just established.
Now the computer will first of all draw the original malocclusion on which you see certain control points which the orthodontist decides. He decides what the width should be. He digitizes where he wants the lower incisor to be. This is all individualized. All the computer does is make it easy to handle. Now, we have the new arch form constructed. Both the original and final arches are shown on the screen.
JCO Do you have an arch form formula that you have worked out?
DR. BURSTONE Yes. The anterior part of the arch is a segment of a parabola, so it fits a parabola between the points that you select. There are enough control points, so that each arch form is individualized for the patient. When we have decided where to position the midline, the computer stores that decision and it then calculates the arch length inadequacy. Also, the computer graphically shows us where each tooth will be in our individualized arch.
JCO What are the control points that the orthodontist decides in determining arch form?
DR. BURSTONE One is a midline point--how far backward or forward you want the incisor. He also selects the width points where he thinks the tips of the cuspids should be, and the mesiobuccal cusp of the first and second molars.
JCO These are selected by the orthodontist and digitized.
DR. BURSTONE Yes. The clinician must make those decisions. No computer can make them. However, our lateral treatment planning program helps with the decision of where the lower incisor goes.
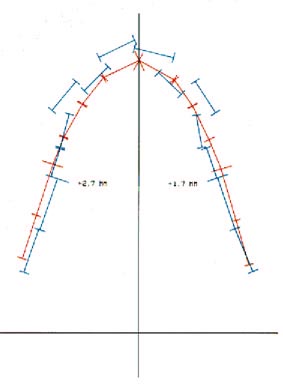
Now, the computer asks if we want to see a hard copy. Normally hard copies are made as a permanent record at the end. The printout is three times life size, so we can see what the relationships are in detail. The longer lines represent the mesials of the first molars (Fig. 5).
The occlusogram plots may look strange if you are not used to looking at them, but you can quickly get used to this representation of the teeth. The original malocclusion is in blue. The final position of the teeth is in red. The arch length inadequacy is the difference between the long red and blue lines at the first molars.
We found out from the computer that we are short on arch length. Now the computer asks what we would like to do about it. Do we want to remove teeth? We can choose to extract and see the "treated case" on the screen. If we don't like the results, we can go back and go through another treatment plot. We can try one with different extractions or nonextraction. A number of different treatment plans can be tried to arrive at the best possible one.
We decided to take out upper first bicuspids. A double check of tooth dimensions on the hard copy shows that the upper bicuspids were over 7mm in width. Therefore, this becomes a reasonable solution. We treated the lower arch on the computer and established the lower arch form. The computer now fits upper arch to lower. We have already instructed the computer to give us a set amount of overjet. We used 1mm for the incisor and for the cuspid. We could have used 2mm for the incisor and 2½mm for the cuspid if we wanted more cuspid rise. In fitting the upper arch to the lower, the computer calculates the arch length inadequacy based on the two arches. Once again, the final decision about what the clinician wants in overjet and overbite is left to him.
The computer tells us that, in the upper arch, on the left side the buccal segments can come forward 2.7mm and on the right side they can go back 1.7mm, based on the repositioning of the incisors. This becomes a severe anchorage problem. The computer once again asks you if you have any other solutions to try. We don't. The final upper arch fits the final lower.
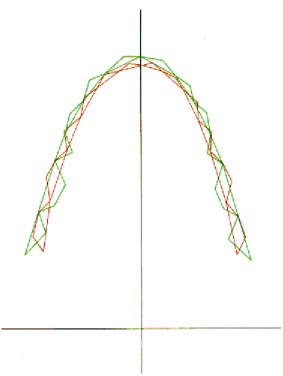
Finally, let us do a computerized wax setup, so to speak (Fig. 6). The red is the lower--central groove, tip of mesiobuccal cusps, tip of distobuccal cusps. The green goes the other way--central groove, mesiolingual cusps, distolingual cusps. Typically, when we set this up with normal overjet, the tip of the mesiobuccal cusp of the first molar will be at the embrasure. So, our patient is a little Class III-ish in the molar region.
We are looking again at where the cusps will fit. The tip of the cuspid would normally go right in the embrasure and this one is pretty close. We can also see how the upper buccal cusps fit with the lower lingual and how the buccolingual widths relate.
JCO Would you please summarize the computer procedures for the occlusogram?
DR. BURSTONE The orthodontist makes the major decisions in our program. He starts with a photograph of his models and determines how far backward or forward he wants the lower incisor to be. He determines what his cuspid and first and second molar widths should be. The dental assistant will then digitize all of the teeth by landmarks on the teeth. The computer will then determine the arch length inadequacy per quadrant. The orthodontist will then decide how he is going to solve the problem--either by extraction or posterior movement of teeth. The computer will then replot the position of the teeth and determine where the posterior segments should be at the end of treatment.
In an extraction case, it will tell us how many millimeters forward the buccal segments can come in each quadrant. The computer also makes calculations along the way that are useful to the orthodontist in arriving at his decision. It measures the mesiodistal diameters of the teeth, compares them to standards, sees if there is a tooth size discrepancy, compares right and left sides for discrepancy. It also gives consideration to the posterior segments and determines where the correct midline should be. Finally, the computer will set the teeth with detailed intercuspation, similar to a wax setup, to see if there are any tooth size discrepancies. At any stage, the orthodontist can cycle back and try another solution.
JCO What is the value in comparing to average tooth sizes?
DR. BURSTONE We really want to know how the teeth fit together. Average tooth size is not the most important factor, because you can have teeth that are uniformly much larger than average and no problem. The comparison between the standard and the individual gives us a way of checking our digitization for big discrepancies. The other way that it is used is that it lets you know the sizes of teeth in case you plan to extract teeth or do some atypical extraction.
JCO Is the margin for error in digitizing less than for other methods of tooth size measurement?
DR. BURSTONE In digitizing, we figure operator error is between ¼mm and ½mm. Most of our devices are accurate to a quarter of a millimeter. I find it far superior to dividers, which have a certain amount of give to them. With a Vernier gauge, it is hard to get exact mesiodistal diameters of teeth. Provided axial inclinations are fairly normal, the use of a photograph is more accurate than other methods of measurement; atypical axial inclinations are compensated for in our system.
JCO How about using a plastic table over the occlusal surface of the model?
DR. BURSTONE I have been teaching occlusograms since 1958 and many of our graduates have elected not to get an occlusogram camera and have used a piece of plastic over the occlusal surface of the model and made tracings manually. I still think it is preferable to use a photographic record, since it eliminates the step of tracing and gives a permanent record.
JCO What is the special camera used to take the occlusal photograph?
DR. BURSTONE The occlusograph uses a view camera with a Polaroid back. By changing the bellows distance, you can make a 1:1 photo. A stage has been made for positioning of the model. All of our models are ground with a V-shaped groove, and they are mounted in centric relation, which is useful for diagnostic purposes. Once the groove is oriented on the stage, we know that the models are in a centric relation relationship. I think the occlusal view is the key to planning. I think you almost learn more about what is going on from this view than from the lateral view. You can see your width problems and your asymmetries.
JCO Do you think that centric relation is an absolute?
DR. BURSTONE Many of our goals might be hard to defend on scientific grounds, but we can't declare a moratorium in orthodontics until we know all the answers. Many goals like centric relation are reasonable goals until proven otherwise. For treatment planning, we need a reproducible reference position. If our patient slides 3mm forward and 5mm to the left, that is no position on which to do our treatment planning. So, we use centric relation as a reference position. That is particularly true of our lateral head films. How are we going to interpret growth changes if we have no stable reference? Can you imagine attempting growth prediction and including the variation in jaw position?
JCO Do you use the machine to make growth predictions?
DR. BURSTONE Yes. Let's try one. The computer is asking the number of years you would like to predict.
JCO Five.
DR. BURSTONE All right. Let's do a five-year growth prediction. You have two options. You can
use mean growth data or you can modify these because of certain hunches that you may have about the way treatment will be.
JCO Let's use a normal growth program.
DR. BURSTONE We just ask the computer for that and here is the original on the screen and now the growth prediction. We are interested in knowing how much the lower facial height will increase. The computer calculates that for you. Vertical height of lower face (ANS to Menton) originally was 75 and afterward was 83. It has increased 7.8mm.
We are also interested in horizontal change. AB to occlusal plane was originally -2.7 and after it is 5.9. So there is a change of 8.6.
Now the computer asks if you want to do that again. You might want to go out a different number of years. You might want to go to maturity. You might want to vary the type of growth. We have the option of using a percentage of the mean for mandibular growth. We don't have to use the averages. We may feel because of skeletal pattern, morphology, or any hunch we have, that instead of average growth, we may have 125% of the average. We may also feel that we are going to have rotation of the mandible and we can build that in.
With our growth prediction procedure, you see the interactive nature of the computer. It is the orthodontist working with the computer. The orthodontist may think, "Well, I have three types of growth that I might expect. Let's see what each will look like before I make my decision." One of the reasons that minicomputers will be useful in an office is that they increase the options you look at. It is also a design tool for treatment planning and appliance design.
JCO It ought to be particular fun when you come to adding treatment.
DR. BURSTONE I believe that the orthodontist wants to individualize his treatment. We are developing programs that go beyond treatment planning, which help the orthodontist in designing his appliance and using it optimally.
JCO What do you think of the idea of successive films--let's say annual films--to determine a pattern of growth?
DR. BURSTONE When I was back in Indiana, one of our graduate students, using the same Denver growth material, made measurements of growth patterns from year to year on the whole sample from age 5 to 21, and there were no correlations between the amount of growth and the direction of growth from one increment of time to the next. No one has demonstrated any way of interpreting two or three serial x-rays to show direction of growth over a short interval of time. Bjork's suggestion of looking at facial morphology is more helpful.
JCO What value do you ascribe to growth prediction?
DR. BURSTONE I think growth predictions are very useful. The first person to point out the value of growth prediction was Ricketts. Any growth prediction is still better than no growth prediction at all, if it is based on good data. Most growth predictions are based pretty much on averages, but you should be aware of what the variation is. Your patient isn't necessarily going to grow down the
center. If you assume that there will be no variation from your prediction, you are not understanding what you are doing with growth prediction. Determining a developmental age, like my facial age concept, is a big help.
JCO Would you say that for most people pattern extension growth prediction is somewhat useful, because most people could be expected to grow that way?
DR. BURSTONE There is a lot of confusion about the word "pattern", I think. At usual treatment ages, a high percentage of facial development is completed. If you have a 12-year-old, maybe there is only 5-10% of growth yet to come. In that sense, the pattern is set. What can happen in that 10%? But, clinically, we are interested in the difference, because even that 10% can give us a change in jaw relationship of 5,7,10mm which might correct a Class II case. So, we want to predict incremental change and that is not patterned. Bjork, for instance, has shown that the magnitude of jaw growth and the magnitude of jaw rotation can change from one period of time to the next.
JCO But, is not the whole essence of growth prediction to take the pattern that you have and enlarge it by the average expected amount of growth of the various parts in the direction in which they are going?
DR. BURSTONE I think it may depend on how you use your prediction. If you think you use the prediction to see what the face will look like five years after you start treatment, then we could say that an average growth prediction may be pretty good, because the face isn't going to change very much in five years.
JCO Why even do it, if there is not going to be that much change?
DR. BURSTONE The way I use growth prediction is different. I am more interested in the incremental change during that time than what the face will look like later, because the total face isn't going to be changing that much. I want to know if the mandible is going to pull out ahead of the maxilla, and by how much. If I have a 7mm Class II case and the mandible is to pull out 5mm with respect to the maxilla, that's what I am interested in. If I have a deep overbite and the distance from ANS to Menton is going to increase 5mm, that's what I want to know.
JCO Perhaps you could bias that to some extent, if you had some intuition about the way this person was going to grow.
DR. BURSTONE I think that the biases probably are intuition at this point. The work of Bjork on the pattern of rotation of the mandible would be part of your bias. There can be knowledge about other members of the family, which might tell you something about increments. Since none of that can really be put on a scientific basis, I think you should call it intuition or art, but it is important that any good computer program have the potential for that intuition. Even with good standards and intuition, part of being a good clinician is to understand that we are not completely predictive, that we must monitor cases carefully, that we must decide on a treatment plan that doesn't put us in a box where we have no other options later in treatment.
JCO Do you first run through a prediction based on the standards and, perhaps, a five-year prediction just laying out an extension, and then modify it if you wanted to, throwing the intuition into a second view of the problem?
DR. BURSTONE One of the advantages of the computer is that it is not time consuming to do both. I could do an average one and then probably do some in which we alter the increments and also try to build some rotation in. A printout or plot will give you some of the variations that could possibly happen in growth and, because all of your options would be reasonable options, it also lets you know why the average by itself might not be the only type of growth pattern the patient could have.
JCO Do you then consider what your treatment options are and whether they are achievable under each of these growth circumstances?
DR. BURSTONE Yes. I like to keep the treatment decision separate from the decision on how the jaws will grow, though they do interrelate. First, I want to know what the bony base relationships will be with growth. Even if it's wrong, it should be your best estimate. Then, when you know where the jawbones are going to be, you can make your decisions about tooth movement and if the treatment options are achievable.
JCO How do you establish the occlusal plane?
DR. BURSTONE I look at the axial inclinations of the posterior teeth and establish what I call a natural plane of occlusion. I also look at the relationship of the lip to the upper incisor to make sure that not too much incisor is showing; and I look at the amount of alveolar process in the upper arch. In the lower arch, I notice the amount of attached gingiva for periodontal considerations. Then I look at the effect of occlusal plane on the AB relationship. The steeper you make the plane, the less AB discrepancy in a Class II case. It may or may not help you, depending on how you look at it. It certainly minimizes the discrepancy. Based on all of those factors, we establish the treatment plane of occlusion. The computer supplies a data base while we make this decision. The next major decision, and the only remaining decision, is how far back we want the anterior teeth on our lateral view.
Following this, the computer draws the positions of the teeth and establishes the occlusal plane. The red line is the skeletal pattern after growth and after rotation of the mandible. Final tooth position is in blue.
JCO You also use the computer to determine forces and select archwires and loop configurations.
DR. BURSTONE Yes. Our use of computers started out as a research tool. We were measuring forces from orthodontic appliances. That developed a great deal of data and it was necessary to use a minicomputer to make it easier to interpret the data. The stereometric development started with our search for a better understanding of forces of orthodontic appliances. If you want to predict the force, you have to know the shape of the appliance. Our wires were bent in all sorts of unusual shapes in three dimensions. We had to record the shape, and that is how we developed our stereometric program.
JCO Are the forces you get in the laboratory transferable to the mouth 1:1? Is there anything about the mouth environment that changes the rules?
DR. BURSTONE There can be variations between calibrations of springs in the laboratory and the forces you get in the mouth due to changes in configuration such as adjustment for patient comfort. But, the most predictable thing about orthodontics is and should be the force system.
Less predictable is the biological response to the force systems. But, a lot of things that are attributed to biological response by the clinician probably are more due to variations in the force system. For example, we talk about teeth that don't move as possible ankylosis. It may be ankylosis of the appliance.
JCO You also use the computer for appliance design?
DR. BURSTONE Once the orthodontist has a treatment plan and knows where he is going in terms of tooth movement in three dimensions, then he can design his mechanics. Let's look at a program for space closure and see how computers can help us in appliance design. The key to any of these programs is flexibility so that the clinician can make his own decisions about what he wants to do.
Let us suppose that we want to use a vertical loop of the simplest design, even though that might not be the preferred choice for space closure. The principle is that loop height should be as long as possible to lower the load-deflection rate and to afford better root movement. We are limited by the mucobuccal fold. The computer asks how high you want the loop to be. The usual range in height of the loop is from 4-10mm. Let's input say 8mm. Now the computer asks what is the distance between the bicuspid and cuspid brackets. It can be from 5-21 mm. We input 14mm. Loop diameter is not a critical variable. We input 1mm.
Most orthodontists would probably put the loop mesial next to the cuspid bracket. If you do, you get a side effect, an eruptive force on the cuspid. Let's put is 2mm off center. The computer asks how much force we want to use to translate the cuspid back. We input 175 grams. We have just input the yield strength of the wire and how much of a safety factor we want for permanent deformation.
JCO The computer will select the size of the wire?
DR. BURSTONE The computer is going to select the size of the wire. That's almost been the fallacy of the orthodontics of the past. Decision on the size of the wire should be on the basis of all of these factors. The computer is going to figure out what cross section to use. We want the wire that gives us the most constant force without permanently deforming.
Note on the screen the computer says that the best round wire section is .016 if that is how much force you want, but it also tells us that if the horizontal force is 175 grams, the vertical force is roughly 25 grams. So, you are going to have force erupting the cuspid of 25 grams, which may not be what you want. It tells us that the moment at the cuspid is 635 gram millimeters and on the posterior is -286, which means that the buccal segments are going to dump in. If we were going to use this wire, we would need a tipback posteriorly.
The force deflection rate is 118 gm mm. That means that you have to activate the loop 1.5mm to get 175 grams. The computer also tells us that one of the weaknesses of this loop system is that the force is going to be dissipated pretty rapidly. Typically, if you wanted to translate the tooth bodily, you would need a moment to force ratio anteriorly at least 10 to 1. This is 3.6. Therefore, the cuspids are going to tip and the posterior segment is going to tip in badly. Knowing that, you can interact with the computer to improve your design.
If you decided to use a square cross section, the computer tells you that .014 X .014 would be the wire of choice. Again, the computer tells you the whole force system. It is a design tool.
If you wanted to use rectangular wire, the best flat section is .012 X .028. That would give you the best properties for this type of tooth movement. The clinician is still making the final decision. If that is what he thinks he wants to do and that is what comes out of the computer, he can use the wire and the activations recommended by the computer. Hopefully, he should know better than to use a simple loop like this for this purpose.
JCO He could change the loop system and see the effect of that.
DR. BURSTONE That is correct.
JCO In your laboratory, you are testing the forces produced by retraction springs and putting the forces and torques on the computer.
DR. BURSTONE Yes. We are calibrating prefabricated springs. You have forces and torques on either end of a retraction spring. Our data for these goes directly into the computer. Starting with 1mm activation, we can measure and record the forces and torques on either end of the springs at various activations. This is where the data comes from for the design of prefabricated springs. Wedesign these springs so they have the proper torques to control the axial inclinations of both the posterior and the anterior teeth.
JCO One of the things that is said about the "by the numbers" diagnostic routine is that, given those numbers and the parameters that the orthodontist may include for various characteristics--how far forward he would consider moving a lower anterior, how far distally he thinks he can move a molar,how much expansion suits him in the cuspid, bicuspid and molar areas--given that, the orthodontist would always make the same diagnostic decision. This is compared to the more common experience in which the orthodontist could diagnose the same case differently on different days, and different orthodontists might diagnose the case differently.
DR. BURSTONE To me, stereotyped treatment is wrong, and this would be a misuse of the computer. If you have a science in which all the parameters are known, then you can input the information and always get the same answer coming out. But, in orthodontics, we have partly an art and partly a science. There are very many parameters that are not part of any computer program, including ours. So, we need some judgment decisions by the orthodontist. If I had to put some number on it, I would say 20% science and 80% judgmental. If it is 80% judgmental, then maybe an orthodontist will get a different treatment plan from day to day. There is more to treatment planning than a few parameters. The fewer parameters you build into your program, the easier it is to come up with the same answer. But, if I start considering such factors as stability, tongue posture, swallowing patterns, the thought process is not always going to be the same. That's why the final
decision always has to be made by the orthodontist. I think he wants to use his knowledge and he only wants the computer to help him a little. He doesn't want the computer to do the whole job for him.
JCO A corollary to that other point of view about computers is that the computer can be used to set standards of quality.
DR. BURSTONE Part of this can also be a misuse of the computer. Somehow, if a computer comes up with a plot or information, many orthodontists are more apt to believe that than if someone drew it by hand. But the thinking process is the same as without a computer. If we use computers, we should always be aware of the assumptions behind how the computer arrived at the conclusion. That's another reason why I like to put the orthodontist in the driver's seat and make him make his own decisions. I don't want to tell him that his cuspid width should always be 52.3mm. Just because the computer said it, he might believe it. If he is deciding this himself, he is not going to come up with conclusions which may not be valid.
In line with what you suggested about setting standards of quality with a computer, the danger is that people are quick to accept what the computer says somehow, because it is not human. It dominates people to an extent, especially the older generation who never worked with it. On the other hand, computers can set the standard for quality workups and treatment planning by making them universally more comprehensive.
JCO The way you are suggesting using the computer is not as a straight jacket, but as a working tool.
DR. BURSTONE It can help raise standards in orthodontics, because it can give you knowledge that will help treat more completely and more rapidly. But, one should not believe that the computer knows more than the people who programmed it. The key phrase about our program is that it is an interactive approach to computer use. The orthodontist interacts with it. Computers can do things for the orthodontist that he would hesitate to do himself by hand. It can draw pictures, and make rapid calculations. I can also give him a data base when he needs it. But the decision making can never be done by the computer. If we honestly think that computers can do the treatment planning, then we think that general practitioners can do orthodontics, because the mechanical parts of orthodontics are more easily taught. What makes an orthodontist is his knowledge and his ability to do treatment planning. I think in the future, the best orthodontists will be those who can do the most careful treatment planning and are most creative. Knowing what you are dealing with can help you in your treatment plan, but there are no numbers in cephalometrics, be they means or standard deviations, to do that.
JCO Do you also make use of the computer for progress reporting and post-treatment evaluation?
DR. BURSTONE One of the valuable applications of the computer is for reanalysis, monitoring progress of the case during treatment and in the retention and post-retention period. We envision computers being able to demonstrate a three-dimensional representation of what happens with growth and development and with treatment.
JCO Three-dimensional cephalometry and cast analysis would be a great advance.
DR. BURSTONE We have developed some new stereometric techniques which allow randomphotographs of study casts or intraoral photographs to be analyzed in such a way as to enable the computer to calculate the position of teeth from them, and the position of bones from x-rays, in three-dimensional space.
JCO Is that a usable clinical tool?
DR. BURSTONE We are currently using this primarily as a research tool. Eventually we should develop it as a clinical tool.
JCO Do you have a way to monitor response?
DR. BURSTONE There are many different types of estimates we can make in orthodontics. We talked about growth estimates and tooth and jaw position estimates. Every clinician makes an estimate of what he expects to happen with his appliance from one visit to the next. In a sense, we are all bioengineers. All of us will look at the patient when he returns, and we would like what we see to be predictable. A good part of orthodontics may not be that predictable. One of the reasons is that force systems and the biologic response are not well understood. Cooperation and growth are not completely predictable. What makes a fine clinician is his ability to be more able to look in the mouth and monitor undesirable side effects and correct for them. The ultimate goal is to minimize the discrepancy between what you anticipate will happen and what really happens. I think most of that discrepancy is at the appliance level now. Maybe, when we have better appliances, more of it will be at the biological level. By integrating the clinical evaluation of progress with progress headfilms and models, computers should go a long way in monitoring where the orthodontist is at any stage of treatment, so that his plan can be updated.
JCO It looks as if orthodontists are going to be able to do a lot more thinking about their cases, and that should not only be good, but welcome.
DR. BURSTONE This is where I think that computers are going to be helpful to orthodontists. Computers will free them from the details and allow them to do what they were trained to do and that is to think.
JCO This could permit orthodontists to operate on a plane a lot higher than bending wires. We already have assistants who can bend wires very well.
DR. BURSTONE Not too long ago, the best orthodontists were the ones who were technically superior with appliance fabrication. The best hands. Orthodontics has changed with bonding and prefabrication, and the computer will change it further. The orthodontist will not be spending his time on mechanical things. In computer terms, orthodontics will be more of a software than a hardware profession.
JCO The work should certainly be even more interesting and exciting for orthodontists.
DR. BURSTONE That's right. I think the exciting things in orthodontics are in treatment planning and appliance design. Optimizing treatment is what differentiates the orthodontist from the technically proficient auxiliary. When the time necessary to do these things becomes less of a factor, then I think that the quality of orthodontics will increase. Most of the troubles we get into are usually problems of poor planning.