JCO Interviews Dr. Richard S. Rutkowski, Dr. Bruce Sanders, and Dr. Roger S. Wolk on Surgical-Orthodontics
JCO How do you evaluate a surgical-orthodontic case?
DR. WOLK We get intraoral and extraoral photographs, tomograms, head films, panoramic and periapical x-rays, and models. The tomograms are valuable to verify TMJ position. Surgery must be planned with normal condyle/fossa relationships in mind. The full face photographs should be taken with lips at rest, together, and in a full smile, to evaluate lip length, mentalis strain, and gummysmile, especially in vertical excess cases.
In addition to the orthodontic evaluation, I do a surgical forecast on all my cases. Often, I will forecast several alternatives. I discuss my findings with the oral surgeon and we agree on which approach to take, before we present the case to the patient.
JCO Is orthodontic treatment usually necessary both before and after surgery?
DR. SANDERS Virtually every case will need presurgical and postsurgical orthodontics, because we attempt to achieve as near an ideal occlusion as possible.
DR. RUTKOWSKI On mandibular corrections, we have a fair amount of orthodontics done before surgery due to the excessive amount of dental compensations present. On the maxillary cases, we generally want to eliminate gross dental interferences. On segmental maxillary osteotomies, the majority of the orthodontics will be done postsurgically.
DR. WOLK Many cases that have been orthodontic failures, such as high angle Class II cases with long face syndrome, present fairly nice alignment in each individual arch. The orthodontist tried to no avail to close the bite and compensate for the skeletal deformity. These are straightforward cases surgically, because the arches are aligned. A minimal amount of orthodontics is required.
Nontreated adult Class IIs generally require a good deal of presurgical intervention, especially if the lower arch is not in good alignment.
Orthodontists have frequently treated a mild Class III prognathism with a good profile by retracting the mandibular incisors. Later, the growth of the mandible overshot the maxilla and the patient required the extraction of two lower bicuspids or a lower incisor, and still remained a Class III skeletal pattern. These are results that can be avoided with proper planning. I have never seen a skeletal Class III treated orthodontically that looked as good as it could have had it been planned Properly and treated surgically as well as orthodontically.
DR. SANDERS Not only is it difficult to reverse your orthodontics but, after two to four years of orthodontic treatment, it is very embarrassing for the orthodontist to try to explain to the patient and parents that all the orthodontics must be reversed and space may have to be opened for bridgework.
DR. WOLK In most Class III surgery cases, the objective is to advance the lower incisors to an uncompensated position from a linguoversion. The negative overjet should approximate the skeletal discrepancy in order to get good skeletal and dental results. A wide band of attached gingiva on the labial of the incisors is necessary if significant advancement is contemplated.
JCO How do you decide, particularly in a borderline situation, that this should be a surgical-orthodontic case?
DR. WOLK Through cephalometric and soft tissue evaluation, as well as through discussion with the patient about his needs and desires.
DR. RUTKOWSKI We have to weigh facial esthetics, supporting structures, occlusion, cooperation, time involved, surgical limitations due to bony anatomy and root structure.
DR. SANDERS Gross dentofacial deformities are rather straightforward. Minimal deformities are more of a problem.
DR. WOLK Once we have established where the deformity is, the orthodontist has to ask himself, "What can I do orthodontically for this patient?" In a maxillary protrusion, there is no question that the orthodontist can retract teeth and change inclinations. He has to ask himself, "Can I move these teeth back into the appropriate position bodily, without tipping, bone loss, or root resorption?"
Severe Class II cases with excessive labial tipping of the upper incisors are much easier to treat than those with upright incisor angulation, because holding anchorage and retracting incisors bodily is a long, tedious task. Root resorption is a factor which must be considered, especially in light of the work of Ten Hoeve and Mulie on palatal cortex anatomy. The length of treatment is also a factor, especially in adults. We have found that an anterior maxillary osteotomy on these cases can reduce presurgical orthodontics to months rather than years. Saving treatment time can be an indication for an anterior maxillary procedure. Orthodontists who deal with adult patients know that it is difficult to move the maxillary anteriors bodily through an extraction site with full anchorage control. Headgear is necessary, and many adults are unwilling or unable to wear headgear long enough to hold anchorage. It requires torque control and intrusive force on the incisors to counteract bite deepening and insure bodily movement. Many adult patients prefer surgery to protracted treatment time and headgear.
JCO Do you consider surgery at any age, or do you generally reserve it for treatment of the adult?
DR. WOLK If we feel that correction is important for the psychological well-being of the patient, we will suggest surgery during adolescence. Adolescence is a highly emotional period, a time when peer acceptance is of paramount importance. Dentofacial deformities may inhibit a child's social acceptance and interfere with school progress.
JCO Are these children who are refusing orthodontic treatment?
DR. RUTKOWSKI Children who are uncooperative in the orthodontic office are frequently candidates for surgery. For example, 13- and 14-year-olds with severe Class II malocclusion may require surgery to achieve an acceptable result, rather than continuing to fight a losing battle with headgear and elastics. Delaying surgery on these youngsters prolongs the inevitable. In the long run, we are ahead if we treat some severe deformities early.
DR SANDERS Especially in retrognathic open bites
DR. WOLK if we treat a Class III at an early age, we operate with the understanding that a secondary growth spurt later in the adolescent years may cause the Class III to recur and surgery may again be necessary. Many girls have completed their active growth by 13-14 and may be operated safely at this age.
JCO How do you judge that?
DR. WOLK Bowden has shown that if the epiphyses of the middle and distal phalanges of the fifth finger are calcified, growth is Complete
JCO How much reduction of orthodontic treatment time do you estimate is involved?
DR. WOLK Proper treatment of a 25-year-old woman with a severe Class II, severe lip strain and sublabial fold, a short vertical dimension, but normal axial inclination requires upper first bicuspid extraction with full anchorage control of the molars to hold them in a Class II posture. It is preferred that no extractions be done in the lower arch. This case would require two and one-half to three years of orthodontic treatment with dedication on the patient's part to wear a head gear enough to hold the molars in their class II position so that the entire anterior segment can be moved bodily without any molar slippage. Often, these cases have pronounced labial inclination of the lower incisors, so Class II elastics Would be contraindicated. It requires anchorage control, slow movement; and a long distance of bodily incisor movement with intrusion, since most of these patients have deep bites and gummy smiles. That is a heavy load for orthodontics to accomplish, apart from the possibility of root resorption.
Now; if we paint the picture surgically for the same hypothetical case, it would require full appliances, alignment of upper and lower arch form, and elimination of rotation or malpositions of the anterior teeth which could interfere with the surgical placement of the maxillary anterior segment. This generally requires six months of orthodontic treatment. Then, surgical intervention could accomplish full maxillary retraction and incisor intrusion up to 5-6mm, which is not possible with standard orthodontic methods. All this can be done surgically in one procedure. A surgeon can control angulation, interdigitation, intrusion, and bodily movement with good visibility and access, provided that the orthodontist guides him in the placement of the segment. The orthodontist then finishes the ditailing phase, closing the remaining space distal to the cuspids, and improving interdigitation. Within a year, that case can be treated with ideal results with the forecasted intrusion, angulation, and retraction of the anterior maxilla.
JCO We are talking about an anterior maxillary segmental osteotomy?
DR. RUTKOWSKI Osteotomy with ostectomy. It is a very simple hour-and-a half to two-hour procedure. Discomfort is generally less Than taking out four impacted wisdom teeth. Swelling is minimal. The hospital stay is usually two and one-half to three days.
DR. SANDERS We extend our team effort into the operating room. After the surgeons have mobilized the maxilla and placed it in a satisfactory position, we like to have the orthodontist come into the operating room and make sure that the segment is positioned to his satisfaction. Than the archwire and/or splint is placed.
DR. WOLK If the orthodontist is not in the operating room to tie in the archwire and to verify that the segment is where he wants it, he is placing that judgment in the hands of the oral surgeon who may not be familiar with possible postsurgical orthodontic problems. But, ultimately it is the orthodontist who has to finish the case. He will also get the blame for poor results.
JCO What are some of the complications of this kind of surgery?
DR. SANDERS Complications following orthognatic surgery are minimal. Complication means that some untoward result will occur if any surgeon, no matter how capable, performs the procedure. For example, mental anesthesia following a sagittal ramus split of the mandible is quiet common. In most cases, it is temporary, a matter of a few weeks to a couple of months, and then the sensation returns. This is a complication that has to be discussed with a patient. A postoperative sequella is something that does not have to occur if the procedure is done well. While there is very little devitalization of teeth reported in these cases, you can get devitalization if you cut through root apices. You can lose segments, if the flaps are torn or ill-designed. These should not occur with a competent oral surgeon, board eligible or board certified.
William Bell in Texas, who has probably done more for the advancement of segmental surgery than any other researcher, has proven that these segments revascularize well and remain viable as long as the flap design is carried out correctly.
DR. WOLK In an anterior maxillary case, if the segment is not moved bodily and intruded to the correct degree, it may be impossible for the bicuspid extraction sites to be closed. The lower incisors will hit the cingulums of the upper incisors and will not allow for closure of the extractions sites or for elimination of the deep bite. If the maxillary segment is mistakenly tipped down as in Class II, Division 2, the orthontist is stuck. We must close extraction sites, torque and intrude the incisors, and upright cuspids. For every degree of tip of the incisors, the cuspids will also tip and need root paralleling. Remember, we are dealing with one segment of six teeth, not just one individual tooth. So, if the segment is tipped down 10º, that would mean uprighting cuspids, intruding incisors, and closing residual spaces. So, it is vital that the oral surgeon understand how difficult it is for an orthodontist to torque teeth and upright roots. It is also vital that the orthodontist know how important it is to place the segments properly and how difficult it is for the surgeon to work in that area. Poor segment placement is a sign of poor communication between orthodontist and surgeon.
JCO What procedures are now used for correction of the prognathic mandible?
DR. SANDERS Most of the procedures done today are osteotomies in the ramus. One of the more standard procedures is an extraoral submandibular approach to the ramus and cortical osteotomy of the ramus. Caldwell's procedure. This is used extensively in the United States and has proved to be a very reliable procedure. Obwegeser's influence in the United States in the last decade has changed our approach a great deal toward the intraoral osteotomy and we try to do it whenever possible. The sagittal split osteotomy is extremely popular in the United States, because it avoids the external scar. It gives a good deal of surface area for healing because of the sagittal approach and it is versatile. Its major disadvantage is that you are in close proximity to the inferior alveolar nerve. Nearly all of the cases postoperatively have transient anesthesia or paresthesia which resolves over a period of weeks to a couple of months. Some surgeons object that it does not give you adequate visualization. We haven't found that to be a factor. It is a reasonably good approach to the management of mandibular prognathism and retrognathism. Another approach is the intraoral vertical or oblique osteotomy. This is a good procedure, but should generally be utilized for minimal movements because stripping of the musculature through this approach is difficult. Those are the basic ways, and it is important for the oral surgeon to be versatile enough to apply these osteotomies where indicated.
JCO Are any of them more stable than any other?
DR. SANDERS If done properly, any of them can be very stable. It is important on large movements to strip the masseters. Otherwise, regression is likely.
JCO Strip them and move them?
DR. WOLK Just strip them and let them reattach at the new position. The choice of procedure seems to be more of a personal bias on the part of the surgeon. In certain parts of the country, the intraoral approach just isn't popular. In our area, the sagittal splits are done routinely.
DR. SANDERS There are limitations to them. The sagittal split osteotomy may be contraindicated in patients who have very small oral cavities with limited openings. It may be contraindicated in the massive move. If the prognathism is going to have to be moved 20mm, you may want to go to an external approach and the vertical osteotomy for more direct visualization.
DR. RUTKOWSKI At times, in the large movements, we may want to recontour the angle of the mandible after it has moved distally. We have also found that in older patients we prefer the extraoral approach, because the sagittal osteotomy may not split correctly due to the brittle nature of the bone. Also, well-concealed scars are not as serious a cosmetic problem for this age group.
JCO Is relapse of a surgical procedure a frequent occurrence?
DR. RUTKOWSKI It is a definite concern and we have to choose the surgical approach that will minimize relapse.
DR. WOLK The maxillary procedures are more predictable because you are not altering the pterygomasseteric sling, although slight shifting of the segments is possible due to shrinkage at the bony interface during healing.
DR. SANDERS If the procedure is done correctly in the maxilla, there should be no regression, because there is no major muscle on the maxilla.
JCO Do you sometimes have failure of the preformed splint to maintain the surgery?
DR. RUTKOWSKI Yes, if the splints are incorrectly made, faulty occlusion may result.
DR. WOLK I can't stress enough the importance of accurate impressions for construction of splints and for model surgery. I have seen splints made on grossly distorted models, which could have ruined the surgical result. A few simple rules will eliminate many problems. Firstly, never take presurgical model impressions with the archwires in place. The alginate can easily lift away from the tray and distort the impression. Always remove the archwires first. If the alginate lifts off the tray, redo the impression. Secondly, when replacing the archwires after the impression, be sure they are passive. If the teeth move after the impressions are taken, the splint will not fit accurately.
DR. SANDERS These splints are not massive. They must be made carefully from accurate impressions to be strong enough to hold the segment in place. We also use interosseous suspension wires from the zygoma for added stability and, in certain cases, bone grafts.
DR. WOLK It is not always necessary to have intermaxillary fixation with anterior maxillary surgery, and this is a relief to the patient. Rather than be wired shut for eight weeks, he may choose to have a three-year orthodontic program. That is why in the surgery cases I may have two or three alternatives and often the patient helps us decide what is best for him. Maybe he has insurance which will pay for the surgery, but not for the orthodontics.
DR. SANDERS As far as regression is concerned, we have the most concern about the retrognathic mandible that requires advancement. Advancements in low angle patients show less relapse than high angle advancements. To minimize relapse, Poulton and Ware have advocated the use of a cervical brace and opening the posterior bite with an acrylic wafer; Steinhouser has advocated a suprahyoid myotomy; others have advocated various exercises, longer maxillary fixation, and overcorrection. A combination of these may be employed to minimize regression in high angle open bite retrognathic cases. Most teams are correcting this deformity by impacting the maxilla and getting a resultant autorotation of the mandible. This has proven to be much more stable; and the resulting shorter vertical face height greatly improves facial harmony.
DR. RUTKOWSKI Impacting the maxilla avoids increasing the posterior face height and stretching the pterygomasseteric sling.
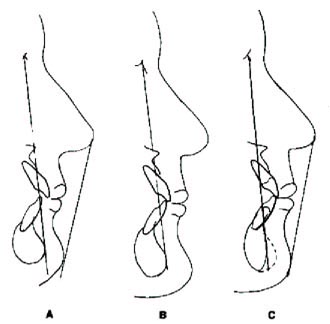
DR. WOLK Epker and his coworkers popularized the maxillary impaction, upward and backward or upward and forward, according to the presurgical plan. The chin rotates forward and decreases lower facial height. Gummy smiles and lip strain are markedly improved. This is a much more stable procedure because muscle attachments are not involved.
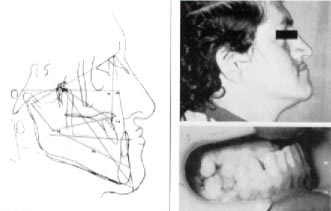
DR. SANDERS Case 1 is a 29-year-old male with a prognathic mandible and extreme overclosure of the lower face height. He also had significant deficiency in the infraorbital region and an acute nasolabial angle.
Case 1: Fig. 1; Fig. 2; Fig. 3; Fig. 4
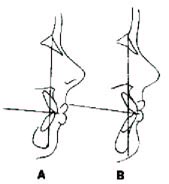
DR. WOLK His lower incisors were supererupted to such a degree that they completely obliterated the maxillary anterior teeth. He also had spacing due to the loss of permanent teeth and a linguoversion of the lower anteriors, which represents an attempt of the incisors to compensate for the skeletal deformity. With this individual, it would be impossible to correct the prognathism by surgical intervention alone. Shortening the mandible to eliminate the skeletal deformity would create an open bite of the posterior teeth, due to the severe curve of Spee. On inspection of his photograph, he appears to have a midface protrusion in addition to the mandibular protrusion. Cephalometrically, his maxilla was slightly retrusive.
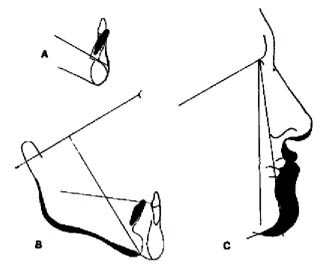
The corpus of the mandible was approximately 12mm excessive. The nasolabial angle was acute, due to the overclosure of his bite. It was necessary to level the curve of Spee in order to provide for good buccal occlusion after surgery. We did a surgical mockup of a mandibular anterior subapical osteotomy. Since edentulous spaces existed in the lower second bicuspid area, we planned to intrude the mandibular anterior segment and to change the angulation of the lower incisors, which were in extreme linguoversion. We wanted to end up with an ideal interincisal angle for good incisal function. The segment was tipped 15º backward in the root area and intruded to level the curve of Spee.
In the forecasting of this case, the first area considered was the positioning of the lower anterior fragment. You cannot plan the degree of prognathic correction without first locating the lower incisor teeth. The lower anterior segment was to be intruded 7mm and the roots tipped lingually approximately 15º, so that the lower incisor to mandibular plane would be within normal range. We don't want lingually tipped lower incisors, because they would reduce the amount of Class III correction that could be accomplished surgically. The farther forward the lower incisors are placed, and the greater the negative overjet, the more Class II correction and facial change we can accomplish.
In treatment, we changed the angulation, intruded the incisors and repositioned the chin. He still had a negative convexity due to the mildly deficient maxilla, but the facial angle is normal at 90º to Frankfort. The forecast defined the surgical objectives.
DR. SANDERS We planned a subapical osteotomy of the mandible through the second premolar region. This necessitated dissecting free the anterior alveolar nerve exiting out of the mental foramena. After the segment was mobilized and repositioned, it was fixed with an archwire. Then, we addressed ourselves to the mandibular prognathism and we performed a bilateral ramus osteotomy on the mandible. After the appropriate reduction was obtained, we placed the patient in intermaxillary fixation. We felt that there was a significant deficiency in the infraorbital and zygomatic regions bilaterally. Therefore, we placed an alloplastic material, Proplast, into the infraorbital and canine fossa regions bilaterally, through incisions in the mucosa adjacent to the pyriform apertures.
The intraoral sagittal split osteotomy we employed is a modification of the Obwegeser-Dalpont technique. It is important not to do a masseteric strip in these cases. It is not necessary and edema is minimized and more adequate vascularity maintained to the proximal segment. Following the sagittal split, the mandible was free to be repositioned. In a prognathic case, a small portion of the proximal segment is cut so that the segments won't overlap.
Postoperatively, you can see a much more harmonious vertical dimension. The chin is less procumbent. The more prominent malar and infraorbital regions make the procumbent nose more harmonious.
DR. WOLK This patient had only two or three months of presurgical orthodontics because his model surgery revealed that the occlusion would be close enough to complete the orthodontics afterward.
The space in the lower arch, which was originally a full tooth width, was reduced approximately in half due to the repositioning of the lower anterior segment. But, the key here is interincisal angle, opening the bite, and good Class I cuspid position. An overlay of the treatment changes superimposed on the symphysis illustrates the intrusion and angulation changes that were predicted. Superimposition on the cranial base illustrates the amount of shortening accomplished in the mandible.
The post-treatment photo shows the remarkable improvement in the nasolabial angle and soft tissue change of the chin. It has been shown that the soft tissue pogonion will move on an approximate one-to-one basis with the hard tissue chin.
JCO Is a retrognathic case more of a problem surgically than a prognathic one?
DR. SANDERS Mandibular retrusion is a very common deformity. Often in the initial analysis, the patient may not seem to have much facial deformity. But, patients who have a mandibular retrognathia, especially young women, tend to posture themselves forward to look better, which can be deceiving. That is why we advocate the use of laminagraphic x-rays and a careful wax bite to make sure you attain centric relation. Many of these patients report to the orthodontist not for correction of the deformity, but because they have temporomandibular joint pain. We found this is due to chronic forward posturing. When we place them into their true position, they often display a significant dentofacial deformity.
In addition to the mandibular osteotomy for advancement, a chin augmentation may be done, if necessary, using a Silastic implant or with a horizontal osteotomy of the anterior mandible, which we prefer because it is very stable. Removal of excess symphyseal bone in the vertical or horizontal dimension is also easily accomplished. The use of alloplastic material or autogenous bone for the augmentation of the infraorbital and zygomatic regions should also be considered in addition to the osteotomies.
DR. WOLK It isn't difficult to place an implant on the infraorbital ridges intraorally while the skeletal procedure is being done. It is just a matter of a few more minutes.
JCO Has the Silastic been a problem?
DR. SANDERS Yes, it has. It can resorb the bone underlying the implant. This occurs to a certain point and then usually stabilizes. Migration of the implant has been a problem and we recommend fixing the Silastic with interosseous wires. When we can avoid using Silastic chin buttons, we will. We prefer the horizontal osteotomy of the symphysis.
Case 2 shows a reduction of the chin. The individual had a good occlusion, but a procumbent, asymmetrical chin. The chin was approached through an intraoral degloving procedure and an appropriate segment of bone was removed. You can see the more harmonious lower one-third after the chin reduction.
Case 2: Fig. 5; Fig. 6; Fig. 7
Some surgeons advocate the trap door procedure, where a segment of the chin is removed, but the inferior border is maintained, placed superiorly and wired into place. If done alone, either procedure can be performed on an outpatient basis.
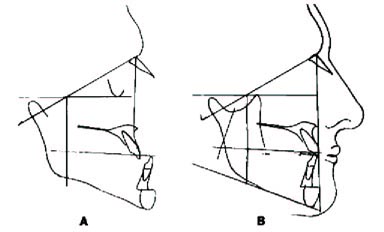
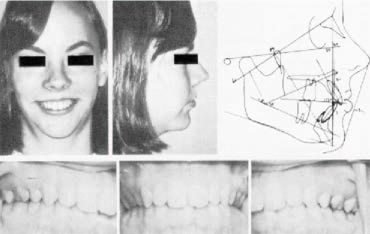
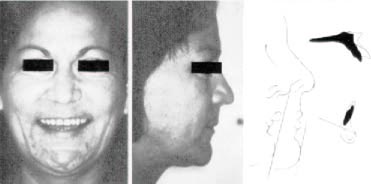
DR. WOLK Case 3 had a severe mentalis strain as well as a sublabial fold, due to the prominence of the upper incisor teeth. The upper lip was normal in length and her nose was of normal width. She had excess vertical eruption of her maxillary anterior teeth. The lip strain results from an attempt to close her lips over the incisors.
Case 3: Fig. 8; Fig. 9; Fig. 10
One of the most important clinical observations in surgical cases, especially in maxillary protrusions and open bites, is the relationship of the resting upper lip to the upper incisal edge. We like to see the upper lip approximately 2-3mm shorter than the incisal edge. If the lip is extremely short and the incisors are overerupted, a gummy smile usually results. Mentalis strain will result, due to excessive stretching of the lips when closing. Another area to examine is the nasolabial angle, which is formed by the columella of the nose as it intersects with the angulation of the upper lip. An angle close to 90º is within normal range. Many patients who have an obtuse nasolabial angle have a turned-up nose. These patients also may have a very streamlined appearance with the chin retrognathic and the nose pointed forward.
DR. RUTKOWSKI If the lips are very tight against the anterior teeth, we can anticipate more soft tissue movement than with loose, flaccid lips. On the average, we may expect a one-to-one ratio of soft tissue to hard tissue movement, but lip tonicity and racial type will create large variations from normal.
DR. WOLK Excluding lower lip and chin, this patient's mid and upper face had good balance. The occlusion was a full Class II with a crossbite of the upper left molar, a severe deep bite, narrow arches, and crowding in both arches. It is the example we alluded to before-- an upright upper incisor and a full Class II molar relationship. Class II cases with a crowded lower arch present difficult treatment decisions, especially if the lower arch cannot be advanced or expanded. Cephalometrically, this patient had a normal maxilla. The mandible was retrognathic, with an 83º facial angle.
We try to treat our skeletal deformities by correcting the abnormal member. In this case, advancing the mandible would have been the proper choice of treatment according to the cephalometric analysis. However, if we advanced the mandible to a normal position, we could anticipate a Class I occlusion with crowding in both arches, which would have necessitated a four-bicuspid extraction treatment prior to surgery. In an adult, this would have involved two and one-half to three years of orthodontic treatment in addition to the surgery. We considered this approach and had no objection to it, except that stability is less predictable in advancing the mandible than in treating the maxilla.
We then evaluated the possibility of an anterior maxillary osteotomy to correct the overjet, knowing full well that the maxilla was in a normal position. By setting the maxilla back and performing a chin augmentation, we concluded that the difference in soft tissue would not be enough to cause us to choose advancement of the mandible rather than retraction of the maxilla. One additional benefit in treating the case in this way was that the orthodontics could be performed much more quickly by rounding out the upper arch and extracting one lower incisor to allow rounding, leveling and aligning the remaining lower anteriors without advancing them excessively. We judged that this could be performed in about nine months and that the patient would be in and out of surgery in approximately one year. We thought we could improve the mandibular deficiency with a sliding genioplasty. No advantage was found to warrant taking a long term orthodontic course with less predictable surgical results.
DR. SANDERS On these close-call cases, it is important to discuss the deformity with the patient and the parents and to ask them where they think the deformity is. This may help to decide where you are going to correct the deformity. Facial self-image is very important.
DR. RUTKOWSKI From the prediction of the maxillary setback with chin augmentation compared with that for mandibular advancement, we felt either profile would be acceptable in this individual.
DR. WOLK The post-treatment cephalogram illustrates how the augmentation of the chin was successful in reducing the retrognathic appearance of the mandible. We were able to get a pleasing result, even though we intentionally made compromises for the sake of stability and shorter treatment time.
The chin augmentation procedure doesn't affect the teeth at all. There are no vitality problems. It has long range stability, especially with the wedge approach in which a wedge of bone is removed superior to the mental region and the lower section is rotated up with the periosteum and muscle attachments intact.
In treating anterior maxillas, the nose should be evaluated carefully. The nasolabial angle will increase in nearly every case of maxillary retraction. In this case, it opened up approximately 15º as we predicted and also appears to be larger because the maxilla has been retropositioned. So, on patients who have a large nose to start with, it is important to tell them ahead of time that their nose will look larger after the surgery. If poor nasal esthetics is expected, rhinoplasty should be discussed with the patient.
JCO How many rearrangements on the models did you go through before you decided on the final approach to the problem?
DR. WOLK Just two. One forecasting the maxillary osteotomy with extraction of one lower incisor, and the other was the advancement of the mandible after extracting four bicuspids.
DR. RUTKOWSKI In most cases in which we are retracting the anterior maxillary segment, we remove first bicuspids and the ostectomy is done in the extraction sites. By performing cuts on the models, we can see prior to surgery how much bone we want to remove in the extraction site. Wetake these measurements to surgery and, if we are doing a rotation, we may want to take more bone off at the crestal area and less off the apex or vice versa. In this way, we eliminate large bony gaps.
We can also do segmental osteotomies without removing teeth. Sometimes, space exists between the teeth in the area where the cuts are to be made. If not, the orthodontist can open slight spaces between the desired teeth to allow for bony cuts. When cuts are made between teeth without space, the interproximal bone may be damaged and tissue loss may occur.
DR. WOLK That is a very important point for orthodontists. In most cases it is not necessary to remove a tooth to get room for osteotomy cuts. One to two millimeters of space is enough to give
the surgeon access without having to sacrifice teeth.
JCO Is opening the sinus a problem in maxillary surgery?
DR. RUTKOWSKI It has not been a problem. We will often go through the sinus as an approach to finishing a palatal osteotomy.
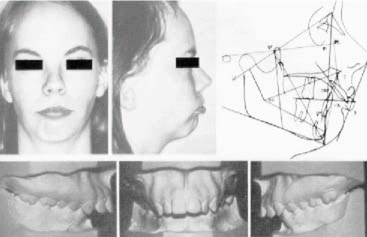
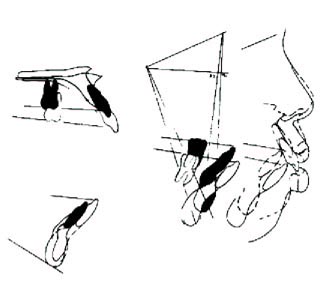
DR. WOLK Case 4 presented with an extreme bimaxillary protrusion, severe gummy smile, and extreme lip strain upon closing the mouth.
Case 4: Fig. 11; Fig. 12; Fig. 13; Fig. 14
In the black community, bimaxillary protrusion is a common occurrence, but mouth strain is a key factor. Many black patients have procumbent lips and incisors, compared to Caucasian cephalometric norms, but they have no mouth strain. This patient's main complaint was the gummy smile. When she smiled, her teeth literally jumped out at you. The upper lip retracted approximately a half-inch above her teeth and back posteriorly, so that a ledge of bone and gum tissue was apparent when she smiled. She had a perfect Class I occlusion, no crowding, no spacing, good root development, good healthy dentition, and good tissue tone. Her problem was cosmetic rather than dental.
The headfilm illustrates the extreme bimaxillary protrusion. The lower incisor is 14mm ahead of the APo line. The maxillary depth is 98º, which indicates approximately one-fourth inch of skeletal protrusion.
JCO What is normal for blacks?
DR. WOLK The lower incisor approximately 5-6mm ahead of the APo plane. Sometimes, I find 6-8mm exists with no strain in the face. So, it is the lip strain that I focus on, more than the protrusion of the incisors.In this case, her chin appears to be excessively retrognathic, because the lip strain and severe protrusion of the maxilla causes flattening of the mentalis muscle. On cephalometric evaluation, the chin position is close to average at 87º. Her skeletal deformity is an extreme protrusion of the maxilla.
DR. RUTKOWSKI We call this a total maxillary alveolar hyperplasia, with an extreme vertical distance between the floor of the nose and the occlusal surfaces of the teeth.
DR. WOLK To reduce the excessive lower facial height and improve her facial balance, we felt that autorotation of the mandible would shorten the lower face height and bring her chin forward. To retroposition the maxilla enough to eliminate the gummy smile and mentalis strain, it is necessary to move the mandibular incisors back. If the patient had a Class II relationship, we could position the maxilla posteriorly into a Class I relationship. But, in this Class I bimaxillary protrusion, we started out with a good overbite/overjet relationship and wanted to move her maxilla back 8mm. We would obviously have an anterior crossbite if we didn't also distalize the mandibular incisors. Two lower bicuspids were extracted to provide the room. So, in addition to the total maxillary alveolar procedure, we did a mandibular anterior segmental procedure.
DR. RUTKOWSKI For the total maxillary procedure, we do not necessarily move the entire palate, unless it is shallow. In this case, the palate was left intact. The osteotomy was performed in a horseshoe fashion with horizontal cuts made above the root apices. The maxillary arch was separated into two halves in order to constrict the width of the arch when the maxilla was distalized.
Otherwise, a buccal crossbite would result.
DR. SANDERS We judged clinically that 8mm of intrusion of the maxillary incisors by impaction of the maxillary anterior segment would eliminate the gummy smile. However, if this were done solely as an anterior segmental procedure, it would have created an 8mm step between the cuspid and bicuspid. So, a total maxillary procedure was necessary and the surgery was performed in this manner. First the mandibular osteotomy was done and an acrylic splint was placed to stabilize that segment. Then the maxillary procedure was done and a maxillary splint was keyed to the mandibular splint. It is very important that the splints be constructed from models mounted on an adjustable articulator, such as a Whip-Mix, to insure proper indexing in centric relation.
JCO Was all the surgery performed in one day?
DR. RUTKOWSKI Yes.
JCO How long a procedure was it?
DR. RUTKOWSKI Six and one-half hours. In moving the maxilla upward and backward there is a lot of bone to be removed distal and superior to the tuberosity area. Access is limited and it is very tedious. The bone must be removed slowly in order to maintain good bony contact.
DR. WOLK Looking at her posttreatment cephalometric x-ray, it is apparent that we retracted the maxilla to a normal position with reference to the cranial base.
The mandible autorotated, lower face height was shortened and pogonion moved forward to a compatible relation with the maxilla. The patient now has more harmonious facial proportions.
She still has a bidental protrusion, but the lip strain is the key in this case and not the incisor to APo measurement.
To summarize the treatment changes that were performed for her, the lower incisors were brought back according to plan, the upper incisors were lifted and retracted.
When the mandible autorotates, the mandibular occlusal plane swings up. Therefore, there is less intrusion in the posterior region than in the anterior region. Therefore, the maxillary anteriors are lifted slightly more than the posterior in impaction cases in order to achieve interdigitation.
Notice that her teeth are now centered in her smile line. She has normal lip closure with very little strain; and the retrognathic appearance has been eliminated. She has a smile that she can be proud of.
The remaining orthodontic treatment will close a few spaces where the surgery cuts were made and finalize her occlusion.
DR. SANDERS The opposite situation to this, maxillary retrusion, is a problem we encounter secondary to a developmental or congenital deformity. The resultant facial appearance is a pseudo-prognathism with a procumbent looking mandible, possibly a procumbent nose, a deep nasolabial angle, deficient or hypoplastic orbital and zygomatic regions, and a Class III malocclusion.
This can be corrected in the maxilla through various osteotomies, the most common being the LeFort I osteotomy for advancement of the maxilla. If the zygomatic and infraorbital region is hypoplastic, a combined LeFort I osteotomy and onlay of autogenous bone in the zygomatic region may be performed. Alternatives to this can be the LeFort II or III osteotomies that have been popularized in this country by Bruce Epker. Sometimes, these surgeries are done for occlusal corrections, without the presence of the facial signs.
The LeFort I osteotomy involves bilateral cuts through the lateral maxillary wall and the lateral wall of the nose, completely freeing the anterior nasal spine and vomer from the maxilla; and the pterygoid plates of the sphenoid bone are freed from the posterior portion of the tuberosity, using an osteotome. In addition to the maxillary advancement, autogenous bone grafts between the pterygoid plates and the tuberosity have been recommended and, if necessary autogenous grafts to the infraorbital and zygomatic regions. Securing the autogenous bone is a brief, nontraumatic procedure performed just prior to the maxillofacial surgery, requiring only a small incision over the iliac crest.
The maxilla is advanced and placed into proper occlusion. Interosseous and circumzygomatic wires are used or infraorbital suspension wires are brought down to the mandibular archwire. These procedures are done mainly for occlusal changes, but can also be done along with augmentation grafts or higher osteotomies, such as LeFort II or III, to correct severe facial and orbital deformities.
The state of the art today in surgery and anesthesia permits performing combined maxillary and mandibular osteotomies and onlay grafts with ease and efficiency. This is done particularly at large medical centers where teams of oral surgeons work together with orthodontists. The procedures require nasal and tracheal intubation. If a lot of blood loss is anticipated, hypotensive anesthesia can be used to minimize it. We also commonly use corticosteroids intravenously to minimize facial edema and thus reduce morbidity and respiratory embarrassment.
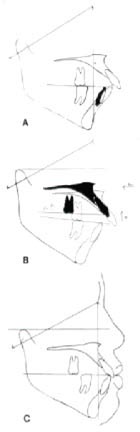
DR. WOLK Case 5 is a woman in her mid-thirties with a severe Class II deep bite malocclusion.
Case 5: Fig. 15; Fig. 16; Fig. 17; Fig. 18
She had a wide oval face; a long upper lip with no apparent lip strain; a deep horizontal groove superior to her chin, which is typical in many deep bite brachyfacial patterns; overclosed vertical dimension; a prominent chin button; and a dished-in profile. Retracting the maxillary anterior teeth to a normal position would exaggerate the dished-in profile. She also had an extremely long upper lip, hiding her upper teeth at rest.
She is the opposite of the patient for whom we wanted to intrude the maxillary anterior teeth. If anything, we would want to extrude her upper incisors, but the deep bite complicates the problem. Thus, it is necessary to intrude the lower incisors to provide clearance to retract the maxillary incisors without intruding them.
Dentally, there was spacing of the anterior teeth, severe deep bite, impingement of the lower incisors on the palatal tissue, severe rotation of the bicuspid, and a missing upper second molar. The patient had bridgework bilaterally in the mandibular posterior region, creating difficulty in fitting appliances. We used ligature wires around the solder joints to help stabilize the archwire. Appliances were placed to attempt to intrude the lower incisors, but it was apparent after several months that surgical intervention would be necessary to achieve enough intrusion of the mandibular anterior teeth to provide clearance for the surgical retraction of the maxillary anterior teeth.
We created approximately 2mm of space distal to the cuspid teeth to facilitate the vertical surgical cuts. We wanted to avoid sacrificing lower first bicuspids and a subsequent need for bridgework. Model surgery was performed to mobilize the mandibular anterior teeth, and plaster was removed inferiorly to enable the lower incisors to be intruded to the level of the occlusal plane.
Because the maxillary second bicuspids were unusually shaped, we decided to remove them rather than the first bicuspids, even though access is slightly more difficult. Sometimes, the surgical requirements would overrule that decision. A midline cut was necessary in order to widen the bicuspid region to conform to the width in the first molar region, and avoid a large width discrepancy between the surgerized segment and the remaining segment.
Intruding the mandibular anterior teeth surgically via a mandibular subapical osteotomy was necessary. The alternatives for treating the anteroposterior discrepancy were either maxillary anterior osteotomy to retract the anterior teeth or mandibular advancement. So, two forecasts were done and we evaluated the soft tissue results. We preferred the maxillary procedure. The questionable stability of mandibular advancement was a factor in our decision, although a genioplasty along with the advancement would have produced similar soft tissue results.
The mandibular anterior teeth were intruded the prescribed amount to enable us to open the bite. The maxillary anterior teeth were retracted to normal position, although A point became deficient cephalometrically. Fortunately, her upper lip thickened and did not change. Notice the rounding out of the soft tissue contours of the lip, nose, and chin as well as the intrusion of the lower anteriors.
The decision on whether to intrude the maxillary or the mandibular teeth must rest on the relationship of the upper incisors to the lip during rest and smiling. This patient now has a nice smile, even though her teeth are small. Her soft tissue contours have improved, especially the labial mental fold.
JCO Have you tried bonded attachments instead of bands in surgical-orthodontic cases?
DR. WOLK Most oral surgeons prefer bands to bonded brackets, because the force in ligation is far greater than in orthodontic wiring and they want to avoid loose brackets on the operating table and afterward, which may affect the stability of fixation.
DR. SANDERS If bonded brackets are on, we insist they be changed. Nothing is more frustrating than to have brackets pop off toward the end of the surgical procedure, when you are getting things into place and are a little tired. It has happened to me and I would rather avoid that problem.
JCO Are you doing more and more surgical-orthodontic cases?
DR. SANDERS Yes, and we are getting more and more orthodontists involved. I represent a medical center which has traditionally had these kinds of cases, but Rick represents the private sector and it is becoming a more importat aspect of private oral surgery practice. I don't think we have even touched the surface of it.
Everyone likes to use the word conservative. To me to treat a severe Class II or Class III deformity orthodontically alone is not conservative. A conservative approach to that type of severe deformity is to define the orthodontic and surgical therapy. I don't think surgery automatically means radical and nonsurgery means conservative.
DR. WOLK I am surprised to find orthodontists who have never had the experience of an orthognathic case. The patients need to be made aware of the treatment that we are able to render. We orthodontists should not be afraid to suggest surgery, if we feel it would be in the patient's best interest. Many orthodontists have looked upon surgery as a last resort. That is no longer true.