JCO Interviews Dr. Robert M. Ricketts on Early Treatment, Part 3
Craniofacial anatomy demonstrated by xerography. (Courtesy Dr. Robert M. Ricketts a33nd Rocky Mountain/Orthodontics.)
DR. BRANDT Are your serial extractions restricted to Class I malocclusions?
DR. RICKETTS No, I may treat a patient who has a Class II malocclusion which is severe in a retrognathic pattern with upper extraction alone. In some of these cases I would serially extract the upper arch and start moving the upper anteriors backward, leaving the molars Class II. I would want to serially extract and enucleate upper first bicuspids early in these instances.
DR. BRANDT Would you consider correcting a Class II malocclusion into Class I and then do some serial extraction if it were still on the mixed dentition?
DR. RICKETTS The case in Figure 17 is an example of that. That is good procedure, but I'm very careful about doing it because often the early treatment may increase arch length and conceivably it may be a second bicuspid extraction, if any. It is surprising how often headgear and preliminary treatment opens space in the arch.
DR. BRANDT When serial extraction has been done and the mandibular incisors unravel, there is frequently a dramatic realignment along with some lingualization of the lower incisors. The root apices of these incisors seem to center themselves within the symphysis without any appliance therapy. Isn't this where they belong since they appear to be in some type of balance and remain stable until the remaining permanent teeth erupt and cause recrowding? Should these teeth ever be moved from this balance?
DR. RICKETTS This sounds plausible. The fact that the teeth would adjust to this position suggests that there is a relationship between the teeth and the so-called ridge. In the past this has been an accepted belief. This may be tenable as long as the patient is in a good incisive relationship, in a normal overjet and overbite relationship, and if the teeth line up in that instance with the normal so-called balance in tongue-lip function. But because they seek alignment and because they would acquire a position simply because of serial extraction and decrease of arch length material, it does not necessarily follow that that is where they should be left. You still have an overbite and an overjet, and a problem of equilibrium between the jaws. I would hesitate to follow the premise of your question on a routine basis. I reject the idea that teeth must necessarily be over the ridge or, because that is where they developed into a state of malocclusion, this is where they belong. I don't believe that. All teeth should be placed reciprocally between the jaws, not over individual ridges, because the teeth function against opposing teeth, not just against the bony base.
DR. BRANDT Now we'll investigate your approach to the various types of malocclusion. What type of appliances are cemented in the mixed dentition and how does this vary from what you do in the permanent teeth?
DR. RICKETTS Most appliances in all types of malocclusions are cemented. I don't even like Crozat removable linguals for young patients; I use the direct quad helix on the upper, the bihelix on the lower, headgear bands, and bumper bands.
I suppose there are cases in which I will use a bite plate; but, again, I don't have confidence in the use of the bite plate. It tends to be a prolonged and ineffective type of appliance. I will admit that there are cases in which a bite plate seems to assist in the development of occlusion and eruption of teeth. But in the mixed dentition, I will usually get on all the permanent molars with attachments and on the lower incisors with the utility arches. I will use the quad helix to widen the arches (Fig. 18).
I may use an activator or a Frankel appliance, but these are tissue-bearing appliances and not so much tooth-bearing appliances. Now you are dealing with a different objective, alteration of growth patterns, alteration of the environment, and directing the eruption of teeth by releasing pressure on one site and putting pressure at the other sites.
DR. BRANDT May I infer from your answer that you don't band everything in sight.
DR. RICKETTS That's right. We don't band it just because it's white.
DR. BRANDT Are there some types of Class I cases that should be treated in the mixed dentition?
DR. RICKETTS Yes, I would say about two-thirds of them. Angle showed the Class I malocclusion to be the most common kind of malocclusion to be found. If we include in the Class I malocclusion those cases which are slightly Class II in outward appearance with rotations of the upper molars forward, but with the mesiolingual cusps of the upper molars still residing in the fossa of the lower molar, we would have more Class I's than we commonly think. This type patient is a good candidate for management in the mixed dentition.
We don't get referrals for very many Class I type malocclusions in the deciduous dentition. We hear the expression so often, "I don't understand what happened. Those little baby teeth were just like little pearls sitting in there all lined up, and look what happened". No space developed, which should occur for the permanent teeth as arches increase in size.
Again, the approaches we use are long-range forecasting, assessment of arch length and tooth material that is available, and putting it all together with the future size and form of the face. It makes sense to correct these in the Class I situation. In no more than one-fourth of the patients do we extract in Class I's if we have a chance to intercept them at the early age.
The techniques are frequently a quad helix on the upper arch (Fig. 18) and a utility arch on the lower arch (Fig. 19). The quad helix will widen the upper arch and make room for the upper lateral incisors. It will widen the hard palate. I didn't say "split", I said "widen" because it tends to widen the nasal cavity at a pace at which bone can fill in, so that you do not see the splitting of the palate. It is an orthopedic appliance if you use it up in the range of 500 grams. It will rotate the molars distally, and it will assist in the arch length in the upper arch by molar rotation, if you adjust it properly.
In the lower arch you can use the bumpering effect of the lower incisor unit against the lower lip and achieve distal action on the lower arch, as you advance the lower incisor slightly to move the molar distally. You can ligate the deciduous teeth outward if necessary, but they often drift buccally on their own. So, you do not need to band the deciduous teeth in either the upper or lower arch. You overtreat about 10 to 15% and retain for future development.
DR. BRANDT What about your bite opening in these instances?
DR. RICKETTS Depression of lower incisors with utility arches is beautiful. If you have a deep bite after the expansion with the quad helix, you can band or bond the upper incisors, place a utility in the upper, and, with the utility lower, the bite is opened by intrusion of anterior teeth.
DR. BRANDT By the intrusion of the maxillary and the mandibular teeth?
DR. RICKETTS Yes, either or both, but you must be mindful to avoid pushing the laterals into the cuspid crypts. The roots of the laterals converge which is favorable. Here is the beauty of the quad helix appliance. If you widen the palate, you have more space to advance the incisors. Usually you don't have to worry about it as much in the lower arch, because the lower incisors are so frequently ahead of the developing permanent cuspids.
DR. BRANDT You have taught that protrusive Class II problems become progressively worse annually?
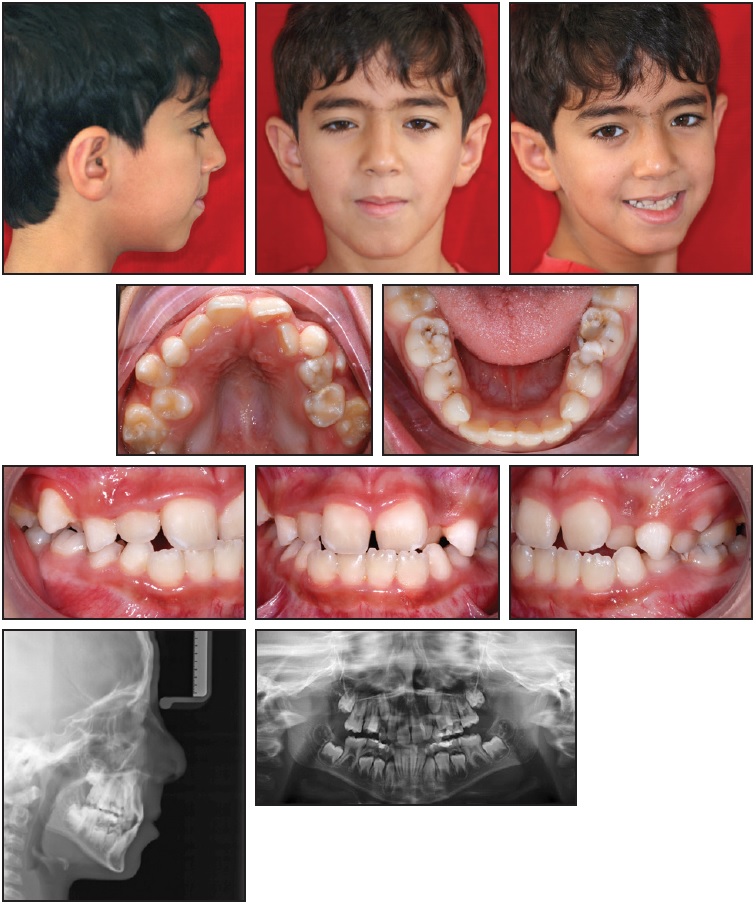
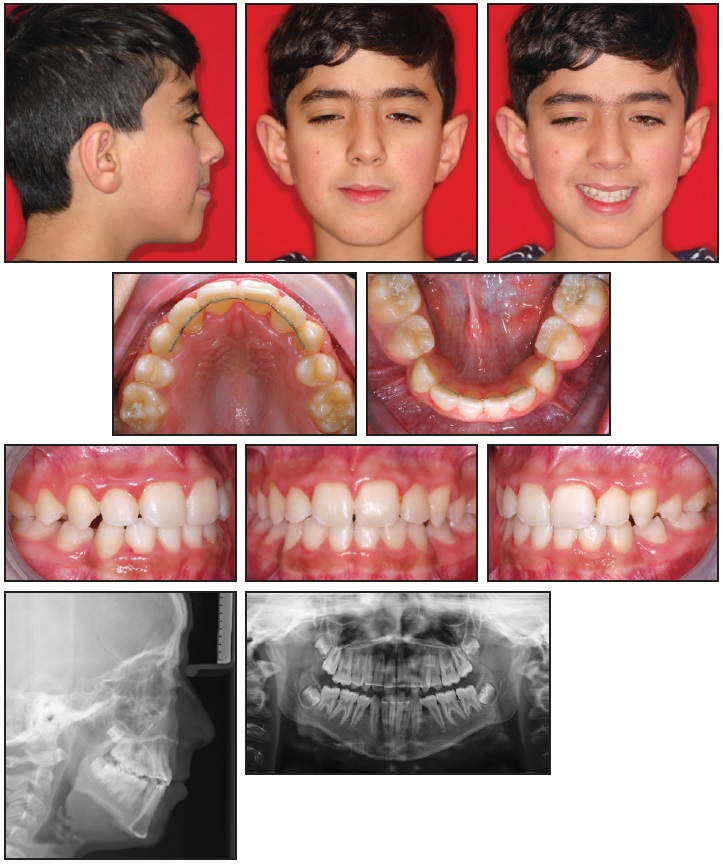
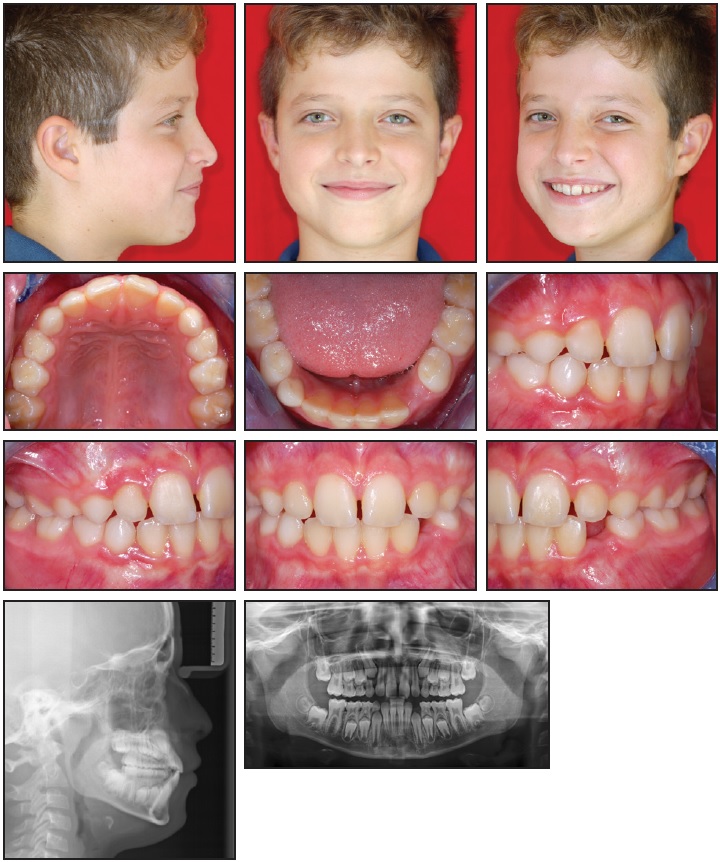
DR. RICKETTS I've taught it because that's what I've found. The patient in Figure 20 is an example. In my research back in Illinois I started in the mixed dentition in cleft palate patients, because of the danger of leaving them to the mutilation from overlay dentures. In my Pacific Palisades practice, many patients were put in observation, but worked up as candidates for treatment; however, I postponed treatment until I could come to that happy day when I could roll up my sleeves, get to work, and do it all at once, just as many orthodontists did at that time. After following hundreds of these patients, I studied them collectively for a report in 1960. Fifty Class I patients who had been observed for a period of three years and fifty Class II patients were studied. These served as controls for comparison of patients that were being treated. I found without treatment the protrusion of the upper incisor (using a measurement of SN-upper incisor angle as you would SNA) was 25 percent worsened in a 30-month period (Fig. 21). That came out to be an eight percent per year increase in malposition of the tooth at that stage of development. These were compared to 50 headgear cases where the incisors not only didn't move forward but were moved effectively backward without ever having been banded! That group further convinced me of the merits of interceptive orthodontics. By waiting, the condition became more severe than it would have been had you intercepted it (Fig. 22).
DR. BRANDT What about Class I cases? Do they get worse annually too?
DR. RICKETTS If you have a Class I patient in which the mandible is growing forward and the patient is becoming a strong prognathic pattern in the growth of the chin, the mandible will be growing, in effect, faster than the maxilla. This means that the compensation for the teeth in the upper arch may take place by forward or outward migration of the upper arch, and crowding will lessen. In those instances the orthodontist does not need to be overly concerned about a minor blocked out upper lateral, because these kinds will self-correct. This is a part of the diagnosis and prognosis. Arch length in the lower arch, however, usually has to be attended to in that situation (Fig. 23). Minor crowdings in the lower arch will become minimized in the good growth situation, because the molar will perhaps drift forward less as the molars lock in good Class I.
DR. BRANDT Do you use Class II elastics in mixed dentition treatment?
DR. RICKETTS Oh yes, I use them frequently. And it is ironic, again, that the lower permanent first molars offer excellent anchorage in the seven-to nine-year old. If it can be set up for cortical anchorage, it will actually display greater resistance and more anchorage at that age than it will at the 12-year-old level. The reason for it is that the distribution of the external oblique ridge and the buccal plate is twice to three times as thick at that particular time as it is later, when you are dealing with alveolar process only. At the early stage, where it is located, the molar can be locked behind the thick external cortical bone. So, intermaxillary traction in the mixed dentition is a great deal more favorable than it is in the permanent dentition, unless you go back and get the second molar at the later stage and do the same thing with it.
DR. BRANDT You are not concerned about only using light Class II elastics?
DR. RICKETTS Some orthopedic action is possible with elastics when the combined force approaches 400 to 500 grams. I have seen Class II cases in the mixed dentition in which I used intermaxillary traction and moved the whole maxilla back more than desirable (Fig. 24).
DR. BRANDT Do you ever impact the maxillary or mandibular second molars by the use of intermaxillary elastics?
DR. RICKETTS Not the mandibular molars with Class II elastics because you are moving the teeth forward on the mandible. Some orthodontists are afraid of using intermaxillary traction and they will use a utility arch on the lower and a headgear on the upper arch in all Class II cases in the mixed dentition. It means they are driving the maxilla backward and tipping the lower molars distally an inordinate amount and not canceling out the tipping with intermaxillary pull. I would say that in those cases, orthodontists are setting everything too far distally in the mixed dentition.
In the upper arch, very frequently you will see after Class II correction that the upper third molar, second molar, and first molar will all be on an even plane stacked up vertically, and then it becomes a matter of long-range prognosis of the growth of the chin and of the development of the face to see if ever there will be room. I have seen cases of almost that condition in which growth was enough to let the whole thing swing out. If that is the situation you have to look forward to, somewhere later you will either have to take out an upper second molar or an upper third molar early, and you have restricted space in the back of the mouth. That is a part of the diagnosis, that is a part of the prognosis, that is a part of your risk in attending to the dentition up forward related to what you are doing in the back of the mouth. Make no mistake about it, that is a part of your problem.
DR. BRANDT You alluded to the fact that when you move the lower molars forward you are not apt to impact the lower second molar. Some feel that Class II elastics used in mixed dentition or early treatment will move the lower first molars mesially, and the second molars as they erupt, instead of erupting alongside of the first molar, will erupt in a horizontal position and tend to be locked out or blocked out.
DR. RICKETTS This can be true. And we see this in extraction cases. Move the lower first molar too rapidly, and the second lower molar will follow and tip forward and become impacted.
Conversely, if you move the lower first molar backward in certain individuals, you have actually prevented an impaction because the second molar then will be tipped distally as it is guided upward by the first. In effect, the second is uprighted by the distal movement of the first molar (Fig. 25).
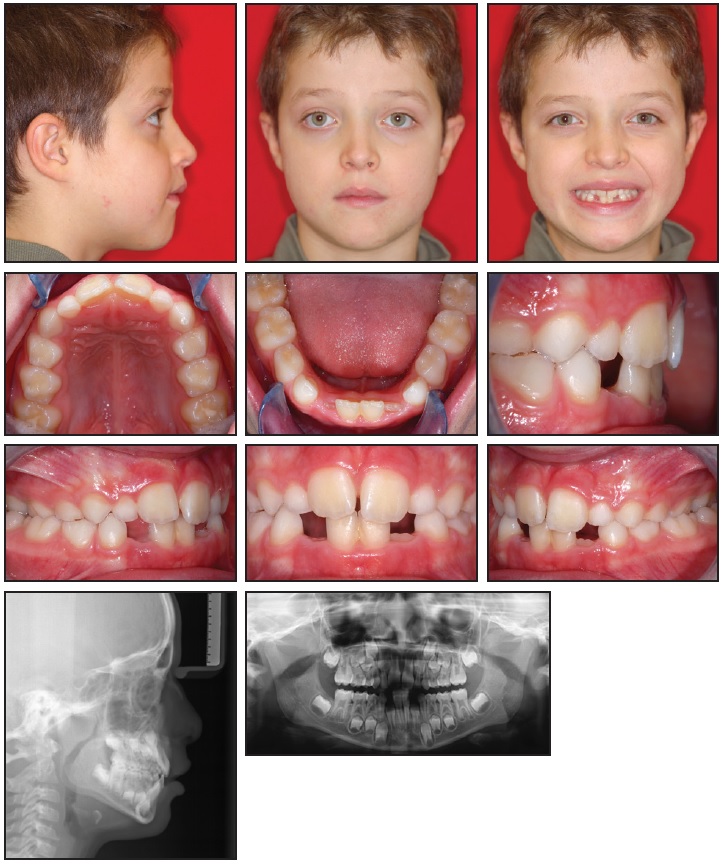
DR. BRANDT If a five-year-old presents with Class III incisors and Class III molars along with cephalometric evidence of a mandibular prognathism that is developing, what do you do?
DR. RICKETTS I usually treat them. There are several factors we look for in the prognosis of the Class III. These are (1) a long corpus, a long body of the mandible from Xi point to PM, (2) a forward position of the Xi point, (3) a short distance from the pterygoid vertical to porion, (4) a short anterior cranial base, (5) an obtuse gonial angle, (6) a short ramus height, and (7) an obtuse cranial deflection. Now, when you get all of these in conjunction with each other, you have a probability that you are dealing with a prognathic mandibular behavior (Fig. 26). On some occasions, I have treated patients who had all of these characteristics in the deciduous and in the mixed dentition with vigorous Class III elastics. And the mandible has opened to achieve the upper arch advancement over the lower. I found in a few instances that I didn't have to treat the permanent dentition. There possibly has been some input into that patient that has prevented the Class III from feeding on itself. Leave those patients unattended and they tend to develop progressive overclosure, and the condyle seems to just keep growing to compensate for the overclosure. There are, of course, genetic Class IIIs which don't have a chance. If you do make the prognosis somewhat later or in the late mixed dentition, it may be an obvious Class III. The anterior teeth cannot contact the lower arch. Many may be delayed for surgery later, which is quite effective and stable.
DR. BRANDT At some point will you recommend surgery?
DR. RICKETTS I think we don't need to wait as long as we sometimes assume we must to do surgery. We could do it, particularly in females, at the age of 14.
DR. BRANDT Can you change or reverse the trend into more normal growth patterns? How, and how long does this treatment take?
DR. RICKETTS In some individuals this seems to have been demonstrated to be done by an activator-type appliance. I remember seeing a patient with Dr. Woodside in Toronto in which a Class III malocclusion that would have been surgical was avoided. Over a period of time that mandible had become what I would term a Class I mandible instead of its original type. Now, at that time, he didn't take credit for the activator making the correction. My intuitive sense said that it had, because I certainly would not have predicted that face to develop as it did.
Unfortunately, I don't see many Class IIIs. In my first thousand cases only about 1.6 percent were Class IIIs. I do see surgical Class IIIs and a few earlier cases in the Oriental population, but not many routine Class III malocclusions at the pubertal stage.
DR. BRANDT You talked before about vigorous use of Class III elastics for that five-year-old patient. Just to enlarge on that, if you do early treatment are you prepared to apply orthodontic or orthopedic forces? With which appliance? And can you define how much pressure you use?
DR. RICKETTS For the deciduous Class III, I put bands on all four first molars and then I go back to the old E-arch technique of Angle. I use a .016 X .022 rectangular wire and I will bend hooks on the wire and ligate the anterior teeth directly to the wire in both arches, using ligatures around the necks of the deciduous teeth. Their crown shape lends them very easily to ligation. Then I will use Class III elastics with 250 grams on a side, to produce 500 grams of total force on the maxilla. I have the patients wear those all of the time, except when they are eating. If they begin to extrude the lower anterior teeth too much, I will give them rest periods. And, I take them into a quarter of an inch overjet!
That procedure does more and is more effective in my hands than putting on a chin cup. A lot of people prefer to use a chin cup, and I tried them years ago. But the foregoing constitutes my technique now for early Class III treatment. In the mixed dentition, I do the same kind of treatment, maybe with some anterior teeth banded. Again, the problem is the extrusion of the lower incisors due to that heavy pull, and you have to be aware of and protect against that.
DR. BRANDT I want to talk about functional appliances in early treatment. Is there a place for functional appliances in early treatment? For Class II malocclusions only? What types are you prescribing?
DR. RICKETTS Of course there is a place for functional appliances. The question might be, "If they have a place, why don't we use them all the time?" And the answer to that is that they just don't seem to be as trustworthy and as certain and as efficient and as routinely beneficial as the fixed appliances that I am using.
DR. BRANDT Do they get better responses in certain types of growth patterns? For example, a high angle case might not respond as well to a functional appliance as a low angle case.
DR. RICKETTS They get the same response in both cases. The difference seems to be in what the patient does when the appliance is removed. If the facial pattern is not consistent with the behavior that has been induced by the activator, then the patient will tend to return to his previous state. In others, the growth pattern will overtake the change that was produced by the functional appliance, and this is the reason that people say the activator tends to work well in patients that have good growth patterns.
DR. BRANDT Are orthodontists limited by certain anatomical barriers in how far we can move teeth? Does this apply equally to the mixed dentition, so that we should study the cephalometric x-ray carefully with regard to the symphysis and the maxillary alveolar housing in the mixed dentition as well as in the mature dentition, and plan treatment in accordance with such limitations?
DR. RICKETTS I emphatically believe that long-range forecasting (of the patient's ultimate size and shape of his jaws) and orthopedic possibilities to alter structure are what you should assess, rather than the limitations of the anatomy that you see at the present time, particularly in the mixed dentition. This means that you have to treat the patient now in accordance with what he will be in the future, and this means sophisticated use of cephalometrics.
DR. BRANDT Let me carry that question a little further. If we see a cephalometric headplate of an eight or nine-year-old youngster with a narrow symphysis, can we predict that symphysis will enlarge a certain number of millimeters by the time the patient is 12 or 13?
DR. RICKETTS No. In the female, the symphysis does not change after age 5 essentially at all. See both Figures 20 and 22. But, the symphysis is not what is holding the teeth. It is the alveolar process that is holding the teeth, and the alveolar process can change and follow Wolff's law of adaptation. The alveolar process, particularly in young individuals, goes with the teeth. The alveolar process doesn't develop unless the tooth is there. The symphysis will get thicker in the male, but not usually in the female. It changes in form due to changes in angulation with the arcial growth of the mandible.
DR. BRANDT Would that mean that we could never move teeth through the labial plate or the lingual cortical plate?
DR. RICKETTS They can be moved with light pressure, and slow adaptation can occur. Over a period of time, there will be an adaptation of the alveolus to correct movement in upper and lower arches and with the establishment of normal equilibrium.
DR. BRANDT Are you interested in aligning the mandibular incisors in a favorable relation to the APo line?
DR. RICKETTS Yes. There is beauty in the use of the APo plane. But not on the APo plane; 1 to 2mm ahead of it at a mean of some 22 degrees. The clinical deviation puts the incisor from -1 to 0 up to +3 or even 4mm (Fig. 27). It was confirmed in our 1960 study that the APo plane served as the most useful guide for the determination of the f lower incisor, for skeletal types, and for age as well. The lower incisors tend to follow the behavior of the APo plane in growth for all types and all ages except in extremes of labiolingual flaccidity or tension. This means that if you set the lower incisors to the APo plane at any age, keeping in mind that you also correct skeletal problems, you have eliminated the effects of the skeletal dysplasia. Once you have a normal APo and have arranged the teeth to that, you have the best chance of stability from what we have learned.
DR. BRANDT Can you intrude maxillary and mandibular incisors during the mixed dentition with stable results? What keeps them there? Why don't they re-erupt?
DR. RICKETTS Because they need to be intruded; the fact seems to be that they are overerupted. This means that they should be returned to their rightful position. It is ludicrous questioning their re-eruption as many have done. What holds any occlusion in normal relationship? Why don't all cases normally go into deep bites? The answer is correct function.
So, if you intrude the lower incisors or the upper incisors or both, and put them in normal function with normal interincisal relationship (around 125 degrees), and normal labiolingual equilibrium and correct habits, then why should they relapse? (Fig. 28).
Some investigators observe that measuring from the symphysis will show an intruded lower incisor to be back up to its previous level again in five years. Well, why wouldn't it be? The patient is still growing and still developing. If the incisor didn't continue to erupt, the patient would develop an open bite, because the whole occlusal plane elevates.
The real question should be whether it relapses into deep bite or not. You might ask, "Why was it necessary to intrude it if it is just going to return? Why don't you just let the posterior teeth erupt? Now, if you want to treat a patient for five years, that's fine. The patient doesn't want to be treated for five years, but it would take that just to hold the incisors and let the posterior growth account for the deep bite. That doesn't make sense.
You could also treat deep bites by mandibular opening rotation, but then you run the real risk of the patient relapsing to a deep bite again and producing condyle damage. Some who have rejected the idea of incisor intrusion have gotten so thoroughly committed to the idea that it couldn't be done, or that it is a bad concept, I am afraid they find it hard to change their opinion gracefully now even when presented with clinical facts and statistical proof, as Chamberlain has shown.
DR. BRANDT When you do intrude upper and lower incisors, can you actually see a shortening of the clinical crown?
DR. RICKETTS Yes, frequently, but not always.
DR. BRANDT Do you notice any reaction around the gingiva?
DR. RICKETTS You may or may not see hypertrophied gingiva at the beginning; but if it is held down for a length of time, you see gradual adaptation.
DR. BRANDT How often do you attempt torque in early treatment? If you do, what are your mechanics like?
DR. RICKETTS In the lower incisor, a straight arch with a straight bracket tends to put the tooth into an ideal normal position. A straight bracket located on the face of the tooth will average 16 degrees from the long axis of the tooth and that's about correct (Fig. 29). In the upper incisors, we use an automatic torque bracket in all cases with 22 degrees on the central and 14 degrees on the lateral. This produces an interincisal angle of 125 degrees which is about ideal, particularly in the young patient.
DR. BRANDT Do you find any problem in torquing with respect to the rootapex and the lingual palatal cortex?
DR. RICKETTS This is another beauty of early treatment. At that time the height of the tooth is at a level where you have a lot of the meaty portion of the alveolus to work with (Please note early condition of JB in Fig. 20). If you wait until the patient is grown and then take the incisor backward, you run into the lingual cortical plate. We try to intrude before we retract the incisors, or else you just move the tooth right through the plate. Sometimes, you are obliged to do that because the plate has adapted to the original protrusive maxillary incisors.
DR. BRANDT Does overcorrection have a part in your treatment in the early dentition?
DR. RICKETTS I tend to overcorrect in practically all cases, but the growth pattern is taken into account. I overcorrect in the adult more than I do in the child. In the child you have future growth to consider. I have treated Class IIs that ended up mild Class IIIs. If you are not careful in overtreating a Class II that has a good forward growth pattern, maybe the eruption and development of the upper teeth will not keep pace with the growth of the mandible in the future, and you will end up with an end-to-end bite after you have treated it for Class II. You have to be wary of this, particularly in males with excellent growth patterns. These are cases in which headgear therapy should not be used. You should use more intermaxillary traction than headgear therapy for those patients to prevent orthopedic change, but still you must overtreat them.
DR. BRANDT Is expansion in the intercanine width in the maxillary and mandibular dentition something to be concerned about in early treatment?
DR. RICKETTS I think we should clarify what is meant by expansion. Expansion has been associated with an increase in intercanine width. That is one of the most unfortunate concepts that has crept into orthodontics. I suppose it goes back to Hayes Nance in 1947 and to Tweed in the '40s and '50s. Our findings are that we do not expand canines permanently, except in those canines which we take up to the normal intercanine width.
If we make artificial arch forms and get them out into a square arch form that was the old traditional edgewise arch, we can expect them to come back. Let me introduce another idea here. In the arch form that we developed as a result of the early edgewise experience, instead of putting in a canine eminence, I put in a canine depression (Fig. 30). This meant that I did not have an increase in intercanine width to the same degree. It was 2 to 3mm less than the old traditional arch width at the canines. We found in a sample of 104 cases out of retention 7 years that there was no change in intercanine width on average. We did not increase it on average, nor did it relapse on average. If you didn't over-increase it, it didn't decrease after treatment.
The next erroneous assumption was that because intercanine width was difficult to increase, expansion or arch length increase was impossible elsewhere. This is totally and absolutely wrong. To assume that you can't expand molar and bicuspid width or that you can't create arch length in the anterior-posterior dimension is incorrect. You can successfully increase bicuspid width. In the transition of mixed to permanent dentition with the correction of the malocclusion and a change of the environment, we've seen lower first bicuspids come in up to 7mm wider than the deciduous teeth which they replaced!
DR. BRANDT Is your quad helix appliance effective in creating more room in the developing dentition?
DR. RICKETTS Yes, but perhaps the headgear is the most effective over the long period, because it is operating in all three planes of space. That's difficult for some to envision.
DR. BRANDT In one of your previous answers I got the feeling that what we can do with a malocclusion depends pretty much on what we can accomplish in the mandible.
DR. RICKETTS It is guided by the mandibular behavior to start with. That is true.
DR. BRANDT So if you gain a considerable amount of arch length in the maxilla, would you agree that steps must be taken in the mandible concurrently to gain more arch space there?
DR. RICKETTS This goes back to an observation I made the first time I visited Dr. Kloehn in 1950 or 1951 in Appleton, Wisconsin. He showed case after case in which headgear was used on the maxillary arch, but I was looking for collateral alterations in the lower arch. I was already aware of the accomplishments in the maxillary arch. From observing Dr. Kloehn's cases, I came away with the hypothesis that for every 5mm of width increase in the upper arch there was a 3mm increase in the width of the lower arch. This means that the function of the inclined planes of occlusion was having a dual effect. This meant that, automatically, therapy on the upper arch would influence the development of the lower arch, if you knew how to do it.
To reiterate what I said before, to make the headgear work you have to be a master, you have to understand all of the factors that are taking place. Not only were the lower molars widened, but they were also being inhibited from eruption or actually being intruded. As I understand it today, you can intrude the lower molar by virtue of Kloehn headgear on the upper arch. That is why I am against putting bite plates on at the same time as Kloehn headgear. I don't want bite plates to open the bite, which would further permit the extrusion of the upper molar and take away from the inclined plane action and that reciprocal effect of the headgear in the upper.
DR. BRANDT How does the quad helix compare with rapid palatal expansion appliances?
DR. RICKETTS Very favorably. The jackscrew appliance in the upper arch, with the two to three week split of the palate, unquestionably separates the two halves of the maxilla. The appliance is fixed, and it directly expands these teeth laterally, but the molars remain in their rotated positions of malocclusion. Most frequently, the upper molar is rotated forward and the jackscrew appliance leaves these teeth in their abnormal rotated state. It is a dirty appliance, difficult to make and difficult to insert, and it takes a laboratory procedure. Also, it has to be maintained in place for a long period for the bone to "fill in". The bone that is replaced has been shown to be very loose and spongy and not very stable. So, there is a real chance of relapse due to the character of the bone. That doesn't mean that it doesn't work and that it doesn't have a place. The maxillary suture appliance goes back to 1910. It was reawakened and popularized by Haas, Wertz, and others.
As a matter of evolution of the quad helix, at Illinois I was using the old W appliance, a modification of the old Coffin spring, for the treatment of cleft palates. I was seeing maxillary alterations with this appliance. Early in my career I took frontal films on a number of patients for whom I used these W appliances on crossbites, as well as on patients that had headgear therapy. I traced the frontal headfilms to see the immediate and long-range effects. I saw many favorable changes we were looking for with palatal splits. I began to see new lamina dura, areas of new bone laid down right in the midpalatine sutures, and I began to see the opening of the nasal cavity with the expansion. This was with the W appliance, but we saw the same thing happening as a result of headgear therapy, when it was progressively widened (Fig. 31). So, with these observations, I developed the quad helix appliance. I put four loops in it, so that it had a range. The beauty of the quad helix appliance is that it can also rotate the teeth as the arch expands. They end up in their natural positions and it's all done at one time. You have to overtreat with it, but the buccal teeth will gradually upright (Fig. 32). And you have to be certain that in the beginning you use enough force on it. You have to expand it half an inch at least to put 500 grams of force on the teeth. Now you will get an orthopedic effect out of it.
An additional beauty is that you can do intraoral adjustments with it. It is a direct appliance, made right at the chair. You make two bands for it. You can place it in one sitting. And the appliance can act for six months before it is removed.
DR. BRANDT In the mixed dentition therapy, do you apply the same principles of cortical anchorage, thrusting the roots against the cortical bone, as you do in the adult dentition?
DR. RICKETTS Yes. I would say that I first noticed it in the mixed dentition.
DR. BRANDT Have you ever detected any root resorption or root damage that might be caused by too early appliance therapy?
DR. RICKETTS I n one case I saw the distobuccal root of an upper molar resorb when it was pushed backward into the developing crypt of a second molar.
DR. BRANDT What malocclusions do you not treat early?
DR. RICKETTS I don't treat Class III's that I feel are going to be surgical. Nor do I treat the Class I that I think has a chance of growing out of the problem or in which I don't think I have enough to gain at the time.
DR. BRANDT Are most early treatment cases two-phase and is there a dividing point where the first stage stops? And how long is the interval between stages in a two-phase treatment?
DR. RICKETTS This is one of the major problems in mixed dentition therapy. I recently reviewed the literature on early treatment, and Angle was a strong proponent of mixed dentition therapy. I don't think that is common knowledge. In 1924 he developed an appliance between the ribbon and the edgewise for the express purpose of early treatment. He called it a baby ribbon. He developed that appliance with Spencer Atkinson, and from that work Atkinson went on to develop the Universal appliance and Angle went on to develop the edgewise.
Angle was a strong advocate of early treatment. He wrote, "it would be regrettable if anyone would take mixed dentition as an opportunity to start a patient and prolong his treatment over an unnecessary length of time". At that time, orthodontists were charging on a monthly basis, and since the appliances would be in place through the whole development of the dentition (5 or 6 years), the patient would be paying all that time. This is what turned many orthodontists and patients off early treatment, particularly in the caries prone ages, because in those days caries was a problem.
Angle at that time said the correction should be for function, for the elimination of all the detrimental influences on the denture. He implied that the orthodontist should then withdraw, to let growth and eruption take over and later come back with finishing appliances. But that is hard to do. It is hard for the orthodontist to discipline himself, with the uncertainties involved, to take everything off and let the patient go. Angle did put retainers in to get out of the first phase of treatment, and I advocate that, too. I advocate treating these cases vigorously to get them into a stage where they have a chance for their own development, and I use a simple Hawley retainer (or modified Hawley because you don't have the permanent canines), and then get out.
Then we give the patient a rest; and when they come back, they haven't been worn out. It is not a matter of retreatment. There is a tendency to downgrade early treatment by saying, "You've got to retreat it. You've got to put all the bands back on again". They make it sound as if it is a terribly traumatic, useless experience and that primary treatment was a mistake. However, if the case has to be retreated, you didn't treat it correctly in the first place. Your later treatment is "finishing" treatment, not "retreatment". You should also remember that for 20 to 25% of patients started early, it's difficult to justify secondary treatment (Fig. 33).
DR. BRANDT Are headgears ever worn over the interim period as retainers?
DR. RICKETTS It takes me about a year to treat a patient with a headgear. The full step Class II should be reduced completely in a year when the headgear is worn only 14 hours each 24-hour period. After that, I use the headgear every other night or every third night as a retainer for about the same period that the patient wore it to make the correction. So, we do not just stop the headgear when the teeth are in Class I. It is important to make sure that the upper molar is uprighted and not tipped, that it is in its locked position behind the lower molar, and that the occlusion has reached a point of stable interlocking. Then you can rest assured that the case will be stable. This usually means progressive release, and that is part of our Bioprogressive Therapy as well.
DR. BRANDT Does this create problems in patient cooperation-- the continuation and completion of treatment, the cost problems, tired patients, etc.?
DR. RICKETTS I have a whole list of the major pitfalls of interceptive philosophy which I use in my lectures, and you have mentioned a few of them. However, I would like to make a further comment. Many orthodontists seem to have the opinion that if they wait until all the permanent teeth are present, they are going to be able to get the patient completed routinely in one and one-half to two years and the results will be stable with all esthetic optimums reached. I don't think they can do it!
I have found that when I wait for permanent teeth, sometimes the malocclusion has grown more difficult to treat; and if I run into a patient who is noncooperative at that particular stage, it is a mess. Had I started these patients earlier, when they were under the guidance and direction of their parents, better success might have been possible. Some of the worst disappointments and greatest problems in management that I have experienced have been in 12- to 14-year-old girls who become defiant of parental guidance. You can't even get them in for their appointments, let alone receive cooperation in their treatment. So, I believe this is another factor that has to be taken into consideration with regard to treatment timing. What are going to be the consequences of waiting and are all of our assumptions actually correct for later corrective therapy?
DR. BRANDT Let's discuss what you are trying to accomplish by early intervention and early treatment. What can you hope to do for the child by starting treatment in the mixed dentition that you cannot accomplish as easily, perhaps, in adult dentition?
DR. RICKETTS A very clear distinction should be made between the goals and objectives of early treatment versus later treatment. A distinct objective of late treatment in the permanent dentition is occlusal perfection. If you do not have the permanent teeth to deal with, obviously that cannot be among the objectives at an early age. On the other hand, we have opportunities in the mixed and deciduous dentition ages to make skeletal changes and to utilize growth and to intercept habit patterns and functional patterns that we will not have at a later stage.
We should make a very clear distinction between the concept of setting up the jaws at the young level rather than setting up teeth at the late level. Let me repeat, "Think jaws and the total patient, don't think teeth". Think in terms of setting up the relationship of the maxilla to the mandible in its harmonious relationship. Think secondly of producing factors that will induce a normal function of the tongue and the lips, so that the patient is now given every chance for development of an occlusion as nearly perfect as possible. Then the permanent stage is left for refinement and finishing, rather than for the gross treatment of malocclusion. The tissues will show the difference between the two concepts and the stability will also be more than gratifying when comparisons are made.
I think, in conclusion, that any seasoned orthodontist recognizes he uses different procedures for his mature adult patients. Analyze these differences and you can see the advantages of early intervention. Certainly it can save teeth and at the same time produce esthetics of the jaws as well as the teeth, accomplish optimal function before it's too late, and achieve remarkable stability. The orthodontist must be masterful in his knowledge of growth and development; he then has the opportunity to get the best results from the least effort.