JCO Interviews Dr. Robert M. Ricketts on Early Treatment, Part 2
DR. BRANDT Now, you have explained about adenoids and breathing problems. Are there any other functional impairments that cause malocclusion in the mixed dentition?
DR. RICKETTS Yes. You can have a crossbite from thumbsucking. Just from the habit of holding the jaw open and sucking in, the maxillary arch will narrow slightly and the mandible will sometimes deflect unilaterally. In studying patients way back in the 1940s, I was beginning to see asymmetries in the mandible as a result of crossbites in cleft palates. At that time we didn't fully understand what could happen. We thought it was perhaps just accidental or coincidental. We didn't connect form and function as important then to the subtle morphology of the condyloid process. Any crossbite malocclusion left unattended runs the risk of developing slight asymmetry in the growth of the mandible and perhaps even more of the maxilla. There is certainly no question that the complete Brodie syndrome, with the upper arch completely overlapping the lower arch, inhibits the development of the lower dentition. Functionally, I'm not certain that it would influence the growth of the mandible that much, but certainly there is a great deal of functional impairment in a case like this.
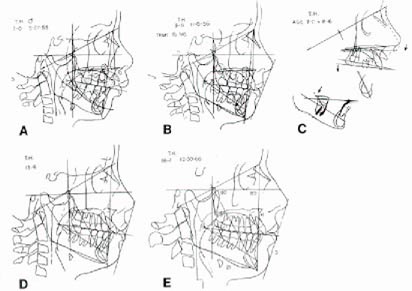
In some instances patients who develop Class II malocclusions are obscured in their amount of Class II because they may be reaching forward with the mandible in a posture to accommodate to the convexity of the face. Actually, if you were to put the condyle back into the fossa, the malocclusion would be even worse. In the situation in which the patient has accommodated by bringing the condyle forward on the eminence, a growth problem may be encountered, but not always. The child patient may alter the growth of the condyle on a functional basis, and the functional impairment can become a growth impairment (Fig. 7). That patient should be diagnosed and the malocclusion reduced so development can occur normally. In my opinion, if the orthodontist ignores it, he is simply not sophisticated in the field today. I reported this in 1965 at the AAO and published it in 1966.
Another type is the Class III. There may be maxillary functional impairment, and theoretically Class III feeds on itself and becomes worsened as a result of the function that is produced by the development of the Class III in the first place.
DR. BRANDT Why can't these be corrected later on instead of doing them early?
DR. RICKETTS They can be corrected later on, but at that time you are again dealing only with the teeth. If you get them early, you have much less of a skeletal dysplasia to treat. In severe cases, you may be subjecting the patient to surgery if you wait.
DR. BRANDT Will a malpositioning due to functional impairment of deciduous teeth which is left alone be repeated in the permanent dentition?
DR. RICKETTS Yes, very frequently. But there are noted exceptions.
DR. BRANDT Does the correction hold in the mature dentition if these items are corrected in the mixed dentition?
DR. RICKETTS Yes, and even improve in the permanent dentition if function is corrected. If you do not correct the whole functional problem, you can expect it to return to a greater or lesser degree later.
DR. BRANDT What do you recommend for a thumbsucking patient with a Class II, Division 1 protrusive malocclusion in a mixed dentition, an open bite, a tongue thrust?
DR. RICKETTS You are describing the case of M.C. which I showed earlier in Part I, and this is a serious situation. My usual recommendations are as follows: first, get adequate full records and study the case in terms of arch length and in terms of an assessment of the nature of the problem. For the history, I like to inquire into the type of thumbsucking the patient is doing, perhaps even talk to the parents in private with regard to their attitude and what the child's home environment is. Then the records are processed; and after the prognosis is made, using the long-range forecast (all of my patients are put through the computer today, which means I get a frontal and lateral assessment with printouts), I get a forecast of the patient's probable growth and a visualization of what the corrected face should look like. This then provides something to use as a feedback to make the decisions.
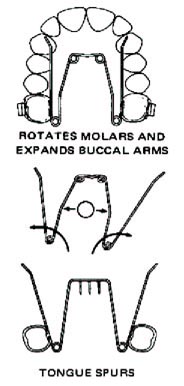
I usually attack the thumbsucking habit right away to overcome that primary obstacle. Today, I would start that patient with what I call the quad helix appliance to which some spurs may be added if necessary (Fig. 8). I can start the rotation of his molars, the widening of the arch, and the Class II correction with that appliance, all at the same time. Then, as a second objective, I would suggest that this patient be treated skeletally. What we would be after now is the gross correction of his jaws--to set the jaws up so that the patient will have the opportunity to express normal development through the mixed dentition.
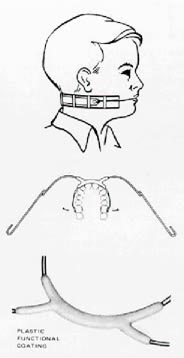
I would use a cervical traction of 500 grams only 14 hours per day (Fig. 9). I would treat the patient for a minimum of a year, and then use the appliance as a retaining device to be worn every other night for another year. In a patient this severe I would probably initiate therapy immediately, because I would be fearful that an accident would fracture the upper incisors. It makes sense to minimize that possibility as much as possible, rather than waiting for a time when I can "get in and out" in a hurry. Also, in a severe case the faster you treat, the faster they relapse later. So, stay with the headgear on them part time to be secure after the correction is obvious.
DR. BRANDT May I just summarize on these items. You would not do anything specific for the tongue thrust at the moment. You would begin to correct the skeletal deformity and you would take some steps for thumbsucking. But as far as the actual stopping of the tongue thrusting, what would you do?
DR. RICKETTS Nothing at first. Certainly not in an open bite Class II skeletal convexity problem. I would make the correction of the malocclusion and get the teeth and the jaws into harmony. I would correct respiratory problems and set the patient up for his own adaptation and compensation. There is an 80% to 90% chance that the tongue will work out on its own. I would then handle the tongue problem if it remained, when I had accomplished anatomical unity. We use a three-step exercise that works quite well.
DR. BRANDT Then you feel that early correction of malpositioned teeth can correct some of these habits?
DR. RICKETTS Not just some of them. I'd say the great majority of them--probably 75%--but that doesn't mean I don't practice physiotherapeutic measures. Let me remind you again: we are also treating the jaw, and the respiratory cavity or the whole nasal capsule, and giving nature a chance!
DR. BRANDT Your teaching of headgear treatment includes many original ideas. I'd like to explore some of these with you. You apply headgear to deciduous molars. When and why?
DR. RICKETTS Yes, I use it on both deciduous and permanent molars. At one time I felt that any orthodontist should be able to place a headgear and understand its management and its objectives. I've done a complete reversal on that. Anyone who is going to use a headgear effectively must be a master orthodontist. That is quite a departure, because many people say, "Well, it's just an early dentition," or "You're still going to have a shot at it later". I don't say that any more.
The proper use of headgear takes an utmost sophistication in the knowledge of what you are trying to do with it. Certainly, I do use a headgear on the upper second deciduous molars. I showed this in Part I. I don't remember ever putting a headgear on the lower deciduous molars. But I do use the lower second deciduous molars a great deal in orthodontic therapy. In fact, we don't use them as much as we should.
But if the upper second deciduous molars are fully formed at the age of three and last until the age of ten, we can put headgear on them just the same as we can put it on the first permanent molars. And we can get the same orthopedic effect as later with the first permanent molars, because the facial bones of the juvenile are more responsive and there is a mandibular growth spurt at that level.
Headgear at about the age of four or five in a Class II malocclusion treats the malocclusion rather rapidly. I had one patient, age four, who completely reduced a severe Class II in a three-month period wearing a headgear 14 hours a day.
DR. BRANDT What do you think happened in that case? Did the mandible unlock and come forward? Did you move everything distally?
DR. RICKETTS The whole upper jaw was moved backward.
DR. BRANDT Is your objective in using a headgear on upper second deciduous molars primarily to reduce a Class II protrusive malocclusion into a Class I condition?
DR. RICKETTS That's right. But again you seem to be thinking and talking teeth, not jaws. If you don't understand how we use a headgear, you may not get the same effects as we claim. To say, "I use extraoral traction," is like saying, "I put bands and archwires on teeth". There is a great deal of sophistication that you must possess to get extraoral traction to do what you want it to do.
DR. BRANDT Would you vary the kind of headgear on a mixed dentition, consistent with the type of growth pattern that the youngster has?
DR. RICKETTS Yes, but I'm not an advocate of extreme high pull off the molars, and I don't know of anyone who was using a high pull headgear before I was. I experimented with facebow high pull headgear in the early '50s, and I just didn't see the things going on that I preferred to see. I didn't have the patient cooperation that I received with the Kloehn headgear, it took longer, and all I seemed to do was to hold the molar at that time.
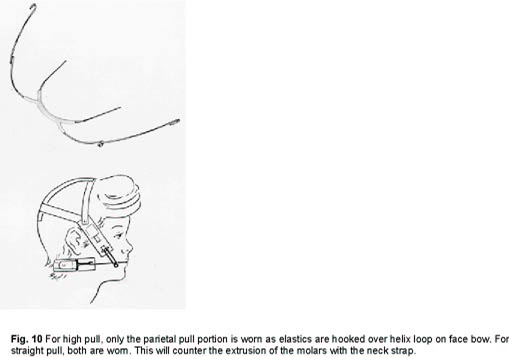
Many orthodontists today are using high pull headgear to prevent mandibular rotation, but in my opinion there are many other factors in treatment which outweigh minor mandibular rotation. These include three-dimensional control of the nasal cavity, control of the occlusal plane, and control of growth. I use high pull off molars in only about 5 percent of my cases. Maybe straight pull is used in 10% (Fig. 10).
The headgear has to be expanded in Class IIs. It also has to be fitted about 1 mm from the incisors so that you can pick up the anterior teeth which are not banded. It has to be worn at the right level at the embrasure of the lips. It has to have the right tension on the neck strap. The facial bow has to be bent up the right way. And, it has to be worn the proper amount of time. If it is overworn, there are damaging factors to take into account. The cervical type should not be worn full time (24 hours per day) in my opinion.
It has to be worn regularly, every day, but it must not be worn too heavily or for more than 14 hours daily to do the job it can do. You have to understand this and you have to be able to trace a headfilm and see what is going on with it.
It is a most difficult thing for me to teach people how you can take the occlusal plane in one direction and the palatal plane in another with a cervical strap and with the Kloehn headgear. It even affects the lower molars and the lower arch rather dramatically (Fig. 11).
DR. BRANDT What effect does headgear on second deciduous molars have upon the unerupted permanent first molars?
DR. RICKETTS It will redirect them to a backward position. It will push them distally and it will push them outward.
DR. BRANDT Do you mean buccally?
DR. RICKETTS Yes. It will take them buccally and distally. If you wear it too severely, too hard, and too long, you will resorb the distal roots of the second deciduous molar, which can result in early loss of those teeth.
DR. BRANDT In this mixed dentition treatment with headgear, can you estimate the potential size of the tuberosity prior to applying headgear? Is it safe to use the heavier orthopedic forces in these instances?
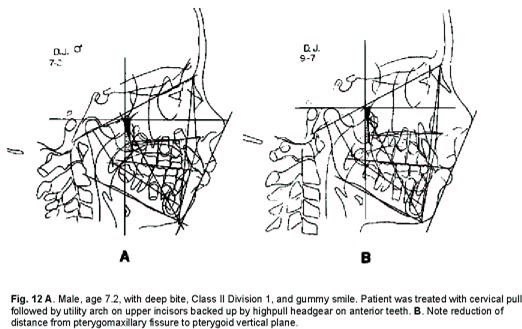
DR. RICKETTS You are suggesting the conclusion that the structures at the tuberosity and the pterygoid plates are immutable structures, and that is not true. One of the observations in the early '50s was that the pterygoid plates and the tuberosity were also altered as a result of headgear therapy (Fig. 12). This is the reason I used the ptery-gopalatine fossa at what I call the pterygoid root vertical rather than the ptery-gomaxillary fissure. Everyone else in the profession uses the fissure, assuming that it is the end of the maxilla. When we began to discover that the fissure was actually bending and changing, at least what was traceable on the head film was changing, we said we couldn't use that because that terminal line was being altered. That is the reason I went back to the posterior margin of the ptery-gopalatine fossa at what I call the root of the pterygoid plate rather than the pterygoid plate bracing at the lower portion of the tuberosity. Particularly in the young individual, we are capable of altering the whole opening, which means the pterygoid plates are capable of remodeling as well. The extent of alteration in that area is 5 to 6mm. But there are still many researchers who have not accepted this. Many orthodontists have been so impeded with the concept of limitations that they reject the whole idea.
DR. BRANDT Are your patients ever directed to wear headgear 24 hours a day? How does it work out? What have you found to be the advantages and disadvantages of full time wearing?
DR. RICKETTS If I have an adult patient for whom I feel obliged to prescribe a headgear, I will use it lighter--about 150 grams--and, if the patient wants to do it, I will have him wear it full time. But then it is a tooth appliance. It is not an orthopedic appliance. So, if I'm going to use a headgear for the purposes of tooth movement and I'm not attempting orthopedics with it, I will permit the patient to wear it full time because I want movement in a continuous manner in that particular instance. Also, if the direction is high pull off the molars, I will keep the force more constant (or about 20 hours) to prevent eruption after the initial upper molar intrusion.
DR. BRANDT Let's identify pressure factors.
DR. RICKETTS Fifty (50) grams is light. One-hundred fifty (150) grams is considered intermediate force. Five hundred (500) grams is for orthopedic treatment. That is about a pound. You don't have the two, three, four and five pounds of force a side. It is 500 grams a side, which means that you have 1000 grams total on the back of the neck.
DR. BRANDT Do you direct extraoral traction against mandibular molars?
DR. RICKETTS At one time I did.
DR. BRANDT Was this done in the mixed dentition?
DR. RICKETTS Yes.
DR. BRANDT Do you do it now?
DR. RICKETTS No. I no longer use headgear against the lower molars at all, but I will occasionally use a high pull anterior against the lower incisors, as Calvin Case once showed.
DR. BRANDT If you don't use mandibular extraoral forces now, what do you do in the mandibular arch?
DR. RICKETTS If it is one of those situations in which I want to move the molar distally, I will use a bumper or a plumping device, and employ lower lip force to move the lower molar backward.
DR. BRANDT What is a plumping device?
DR. RICKETTS It is a shield against the lower lip, or a lip bumper, which is advanced in the sulcus area down low, not up in the fleshy part of the lip but down in the vestibular area where there is a tightness of the lip. (Fig. 13). It has been shown that we can move the lower molars distally if it is left in full time. You can create arch length and you can counter the tension effect of the lips, away from the lower arch. You can get a great deal of arch length simply by the use of a bumper over a period of time.
DR. BRANDT Do you do this on mandibular deciduous second molars?
DR. RICKETTS Yes, either on second deciduous molars or first permanent molars.
DR. BRANDT Have you found that after you have used these lip bumpers to relieve the lip tension (which seems to give you more room for mandibular incisors) that when the lip bumper is discarded, there is no relapse or does the lip tension tend to recrowd the lower teeth?
DR. RICKETTS I read into your question the assumption that the lower incisors are coming forward with the lip. That is not usually true. This is the irony of it. When I first started using these lip bumpers, I did it for the express purpose of unraveling the lower incisors by virtue of permitting them to come forward with the release of the lip tension. That is not usually what was found. The molars went backward and bicuspids widened, but the lower incisor essentially didn't change its anterior-posterior position. That was completely surprising! Once in a while you may be able to see a patient in which the lower anterior teeth tip forward, but by and large what really takes place is that the molars and the bicuspids are altering a great deal more than the incisors are changing.
DR. BRANDT Have you used lip bumpers in the mature dentition?
DR. RICKETTS Yes.
DR. BRANDT Has there been a favorable response when there are no deciduous teeth left on the mandibular arch?
DR. RICKETTS Yes. The difference is, however, that these are slow and insidious changes. If you are after a lot of tooth movement in a hurry, a lip bumper is not the appliance. But if you can be patient and take your time, these changes do take place over a period of time. It is a slow, subtle inhibiting effect that takes place. A lot of people get in a hurry and start putting Class III elastics on them, and I think this is a mistake. One important application of lip bumpers in adults is for the case with thinning of the gingiva and stripping.
DR. BRANDT Have you, then, redirected what might have become an obvious extraction case into a nonextraction case by judicious application of lip bumpers?
DR. RICKETTS That's right. Let me take this one step further. I use lip bumpers in young cases in which there are early recessions, a number of cleftings or runners on the lower incisors. It helps to hold the lip away from these developing teeth. I convert that patient from a stripping in a thin labial attachment into gingiva which becomes hypertrophied, even in the child. A re-growth of the free margin of the gingiva occurs with the release of the pressure atrophy that had been there to begin with! I had an adult patient who started to develop stripping on the six lower anterior teeth. She was a dental assistant, working for a very sophisticated periodontist, and he sent the patient to me and asked, "What can you do about it". He was getting ready to operate on the patient and bring flaps up to cover the labial of the lower incisor. I said I would put a lip bumper on and develop this dentition backward. I took photographs before and after showing that we converted the gingiva from recession to hypertrophy all the way around the lower anteriors.
DR. BRANDT Are there any other procedures that you use to treat shortened arch length?
DR. RICKETTS The Jarabak group, I understand, still uses headgear on the lower arch. I discarded that when I found that I could take a lip bumper and subtly, over a period of time, do an even better job because a lip bumper will not tip the molars distally. The bumper tends to hold them upright because the countering effect of the forces of occlusion tend to offset the upward and backward movement from the lip, so that the bumper tends to take molars straight backward.
But the unfortunate part about lip bumpers is that you can't treat overbite or supraerupted lower incisors with them. You have no purchase on the anterior teeth, so while you can move the molars or certainly at worst check mesial drift, there is still a deep bite. I don't use lip bumpers extensively since we discovered that, with the utility arch, we could intrude these teeth and in the act of intruding them also move the molars distally (Fig. 14). The molars go distally as you have used the incisor intruding force to tip them backward. But as you start to advance the lower incisors, it becomes a secondary force to the distal movement. You are pitting the molar teeth against the lip, which was in effect bumpering, but now using the medium of the anterior teeth with an archwire rather than an artificial device. We began to recognize that attempts to advance the lower incisors in some of these patients didn't result in incisor movement forward but in molar movement distally. When we discovered that (and we have cases in the mixed dentition with a tendency for runners on them), we used a series of T-loops or boot loops across the lower incisors' area to protect the gingiva from the pressure of the lip (Fig. 15). Now we can get the tissue hypertrophy, intrude the teeth, move the incisors downward and forward, and at the same time move the molars distally. We create arch length by using the utility and putting it out to the buccal.
With the utility arch, the curve of Spee is taken care of, the depth of the bite is corrected, and I can't see anything but good happening, except in those cases in which the molar has moved so far back that you crowded the second molar. That is a risk that you run with this approach to any early therapy on the lower arch.
DR. BRANDT Is the blocking out of the lower second mandibular molar a frequent complication with this type of approach?
DR. RICKETTS In about 1 out of 12 cases you may crowd the second molar an inordinate amount. In three or four patients I have had to go in and take out second molars that were trapped. This is what led me to the early removal of lower third molar buds.
DR. BRANDT Do you recommend varying the direction of traction based upon the type of growth pattern for the individual patient?
DR. RICKETTS Yes, but when I talk about vertical growth patterns, I'm talking about Class II correction. Perhaps you should not be trying to treat the patient with a vertical pattern by distal movement of the upper molars in the first place. This is where I think some people get into trouble. These patients should have bicuspid extraction or extraction in the upper arch only. This is the situation which led some orthodontists away from Kloehn headgear. They tried to treat all Class IIs in the early dentition without a decision as to which of them were good prospects for success. If the patient was Class II in the mixed dentition, he got a headgear. Without expert prognosis, trouble occurred with crowding the distal of the upper arch, and ultimately heavy continuous force led to excessive mandibular rotation.
Now, if we diagnose a patient and are reasonably sure of a long facial pattern developing, I will not treat that patient by distal movement of the upper molars. I will either serially extract the upper arch or I will simply delay treatment until all four bicuspids can be removed in that patient. Then I can treat it by bringing the lower molar forward, under that upper molar, rather than by trying to wedge that second molar backward. That is one of the beauties of doing a growth forecast and setting up the case more completely. It will keep you away from these problems. Growth pattern is only a part of the problem, however, as force, pain threshold, time worn, breathing, muscle patterns, and other factors such as expansion are also of great concern.
DR. BRANDT Is it logical to change the force vectors on the headgear in accordance with the total malocclusion? By that I mean the teeth, the cephalometric pattern and the facial contours.
DR. RICKETTS Yes, in very young patients even 150 grams may give some orthopedic force. In a very young patient (preventative) you may get a certain amount of skeletal change with any type of headgear. But the difference tends to be 500 grams if you want the bones to move, and if you want the teeth to move you have to use lighter forces because of the production of ischemia, sclerosis, or cell-free hyalinized areas around teeth from heavy force.
DR. BRANDT Are combinations of high pull and cervical headgear used together? If so, when and why?
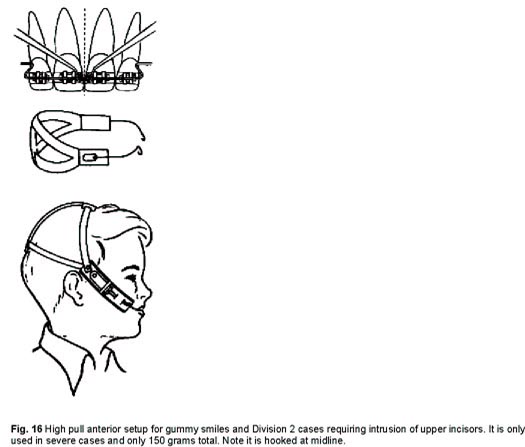
DR. RICKETTS I use six different types or combinations of extraoral traction. The first and most common is the typical Kloehn type with the neck strap (Fig. 9). Another is the high pull off the molars which would be a directional headgear to intrude the molars as they are moved backward (Fig. 10). A third is a high pull off the anterior teeth at the midline (Fig. 16). The fourth is a straight pull used with a combination of the Kloehn and the high pull to prevent upper molar extrusion. The fifth is a combination of Kloehn headgear with a high pull anterior in which I want to reduce the Class II and deliberately intrude the upper incisor teeth or back up an upper utility arch.
If I use a high pull headgear on the anterior teeth, it is very light because I do not want to inhibit the vertical growth of the nose or the growth of the nasal cavity by a restricting force up any more than I would want to make a patient a thumbsucker to push them up. You can use a combination of force against a regular Kloehn.
The sixth is the face mask or reverse headgear for Class III with a deficient maxilla. Even a seventh could be included, the chin cup for Class III also.
DR. BRANDT Are you suggesting that intruding of upper anterior segments can inhibit nasal growth?
DR. RICKETTS Yes, I think vigorous pull headgear on the incisors (over 200 grams) can inhibit the dropping of the nasal cavity in front, leaving the facial height to be expressed in the denture area and making more lip strain for closing the mouth and, ironically, defeating the treatment of a gummy smile which it was intended to do.
DR. BRANDT Are we limited to that by the anatomy of the palatal plane, the ANS-PNS line? If you looked at a cephalometric film and saw that you had 5mm of room between the tip of the incisor and the ANS-PNS line, and if you went up that 5mm, could this conceivably have an effect upon the dropping of the nose?
DR. RICKETTS Yes, with extraoral force, and I have also seen the roots of the upper incisors moved through the floor of the nose. But, again, if it is an older patient, you are not going to get that skeletal effect. I don't think I can take a palate and move it up in front easily, but I think I can take a palate and inhibit its growth while everything else is growing, which means that we have increased denture height.
In Class II situations, at least in the problem cases we have been discussing, you are usually dealing with excessive vertical height in front. In those instances you want to avoid the inhibiting effect. What you are after is to reduce the denture height so that you reduce lip strain which takes the tension off the denture and permits you to treat the patient without extraction and without a gummy smile.
I think this is an issue which should be clarified in your journal because some of the literature claims that Kloehn headgear causes gummy smiles. If you use it the way I use it, it is just the opposite. It corrects gummy smiles.
It is unfortunate that this error ever found its way into the literature because it is still there and still in the minds of many orthodontists. It was an error that it was ever allowed to be published. It's not the Kloehn headgear per se, but the manner in which some applied it. It's like saying that all bands or attachments are bad because some people have root resorption.
DR. BRANDT I have a few questions on serial extraction. Can arch length deficiencies always be detected in mixed dentition?
DR. RICKETTS I never say "always" about anything, but, yes, arch length problems are identifiable in the mixed dentition, or even in the deciduous dentition.
DR. BRANDT Are you able to tell for certain that there will never be enough room for the permanent teeth? How would you establish this?
DR. RICKETTS This is the key to our whole interview. This kind of sophistication in terms of arch length, particularly in the lower arch, is the real substance of early diagnosis and prognosis. It includes the knowledge of the eruption of teeth, the knowledge of the growth of the mandible, the mechanisms of the growth of the mandible, the environmental influences, the growth pattern of the face, the alteration of the maxilla, the tension of the lips, and the behavior of the tongue. To answer that question is to understand today what orthodontics is all about.
I cannot answer your question without including the concepts of mandibular arcial growth, eruption of the teeth in the lower arch, the inhibiting and limiting effects of the tension of the lips working through the forces of occlusion of the upper arch, orthopedic effects, and environmental changes that can be induced in a given patient.
DR. BRANDT Can an orthodontist plan on developing more room for the oncoming dentition that is crowded in its early development?
DR. RICKETTS Absolutely.
DR. BRANDT Are there circumstances that would lead you to initiate serial extraction?
DR. RICKETTS Yes, if I have a patient who has a straight, retrognathic profile with a small mandible and the forecast suggests he is not going to have a big enough table to hold all the marbles, I will then initiate serial extraction. I might even enucleate the bicuspids early, depending upon the pattern of eruption of the permanent teeth. In many instances, if you are going to serially extract, there also should be an accompanying enucleation. For instance, it is a very difficult situation if you want to take out first bicuspids in a patient and the canines are coming up first. That is not uncommon in the lower arch. Serial extraction in that particular instance will not change the pattern of eruption of the canines and first bicuspids.
(CONTINUED IN NEXT ISSUE)