Bio-Progressive Therapy, Part 5: Orthopedics in Bio-Progressive Therapy
The different concepts related to dentofacial orthopedics resulting from application of headgears seem to elicit more controversy than any other area of orthodontics, almost to the extent that each individual orthodontist seems to be able to expound at length on the merits of his or her own unique approach . . . all the way from never using headgears to utilization of headgears for all major movements.
As practical clinicians, we tend to think of distal headgear traction as useful for anchorage or as a method of correcting Class II malocclusion. As a guide, we faithfully inspect the occlusion of the upper and lower first molars and, when we have reached that ideal of a Class I occlusion, we discontinue the headgear; or perhaps we have the patient wear the headgear as long as we perceive they can tolerate it, then finish the case with Class II elastics. This seems to be the most expedient approach.
Similar articles from the archive:
There Is a Difference
Any approach to headgear therapy is right if it accomplishes the result we desire for that one individual case. The problem is, we usually don't know where we want to be. There is a vast difference between correcting jaw position and correcting tooth position. We need to think more in terms of a differential treatment of Class II malocclusion. That is, certain increments of the correction should come by virtue of jaw change (i.e. orthopedic alteration) and certain increments by virtue of tooth movement on the denture base (i.e. orthodontic alteration).
It seems that the most logical approach should be to define where we want to be with our headgears before we select the specific headgear type to do the job, because what would be considered absolutely beneficial for one patient could conceivably produce a detrimental response in another case. The Visual Treatment Objective, is the most helpful medium we have for evaluating where we want to be, by demonstrating the methods for reaching that goal. The previous four articles on the Bioprogressive Therapy have set out a method of determining the goals of treatment through the Visual Treatment Objective. In this article we will explore the various methods of reaching our specific orthopedic goals.
A Method of Evaluation
As most significant changes induced by headgear therapy are evaluated by means of progress lateral headfilms, it is important to once again define an approach by which orthopedic and/or orthodontic alteration can be fairly judged.
By definition, orthopedics implies any manipulation that alters the skeletal system and associated motor organs. From the practical standpoint, in the growing child, orthopedic alteration would be any manipulation which would change the normal growth of the dentofacial complex in either direction or amount.
We must have a reasonable method of differentiating between mechanics response (those changes induced by the clinician) and normal growth. We, therefore, must return to the four basic areas of superimposition and must be able to forecast growth in both direction and amount. Although we recognize that no approach is without its flaws, the methods we have presented are both statistically significant and, at the same time, clinically practical.
If we project a certain cephalometric landmark to extend on a certain superimpositional vector at a certain increment per year (given a known statistical margin of error), it is reasonable to expect that gross variances from that expected or normal growth have indeed been elicited by our mechanics. For example, if we know that point A extends outward approximately 1 mm per year on its gnomic vectoral figure, and that point has been altered from 6-8 mm during a year of headgear application, it is reasonable to expect that the difference between the normal, expected or anticipated position of the maxillae, and that actually experienced, was due to an external force. Even including all types of cephalometric error (tracing error, individual growth differences, et cetera), one cannot explain away 5-10 mm of gross movement in that time frame. Only by creating a mental image of where a certain cephalometric landmark should normally be (anticipated growth in both direction and amount) can we develop a feedback mechanism for evaluating responses to mechanical applications.
For the sake of simplicity, it is important to closely evaluate only four basic areas of superimposition. The first two areas of superimposition are to define specific orthopedic change (i.e. a change in growth direction or amount, or both, of basilar bone). The second two areas of superimposition are utilized to define specific tooth movements on the denture base (i.e. orthodontics) (Fig. 1).
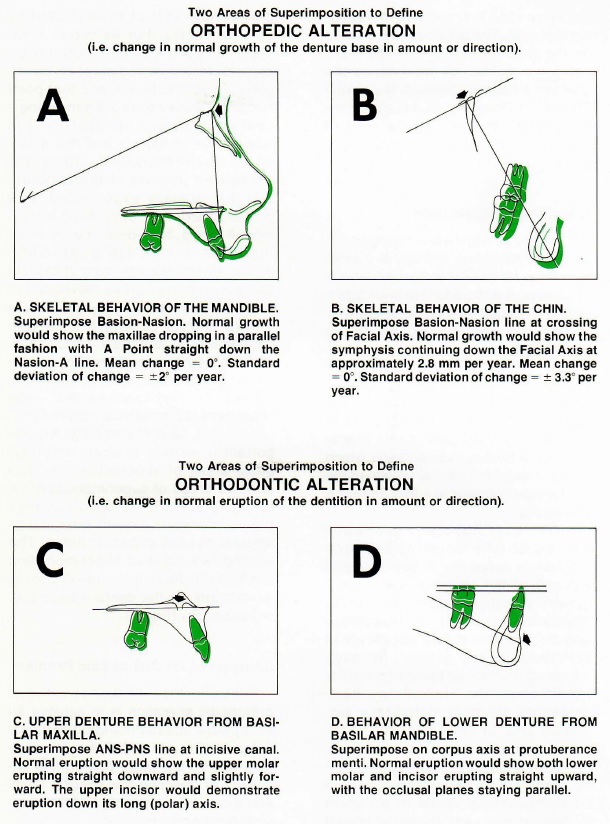
Fig. 1 Four areas of superimposition to define orthopedic and orthodontic change.
Analysis of An Orthopedic Problem
Inasmuch as a major objective of orthopedic alteration is to achieve an acceptable maxillomandibular facial balance (i.e. to relate the maxillae favorably to the facial plane), it is important to describe the specific facial and dental characteristics of the classical orthopedic problem.
Bimler partially described the classical, severe convexity problem as a microrhino dysplasia (Negative factor four). In a sampling of over 234 Class II malocclusions, over 60 percent of the cases with high convexity (+6 mm or more) demonstrated most of the characteristics of microrhino dysplasia. Since the preponderance of Class II malocclusions (and the cases we typically treat with headgears) show these characteristics, it is important to define them and theorize as to their origin and implication.
Normally the palatal line is parallel to, or is canted slightly downward to Frankfort Horizontal line. The microrhino dysplasia has an upward, outward tip of the palatal line with Anterior Nasal Spine (ANS) tipped toward Frankfort Horizontal (FH) at least 4° or more. The upward, outward tip of the palate lends itself to severe maxillary protrusion. Depending upon the age of the individual, a convexity of 6 mm or more is indicative of an abnormal maxillomandibular pose. The upward cant to the palate is accompanied by a short vertical height to the nose, an upward cant to the nares and a disproportionately small upper face compared to lower face height (Fig. 2). Esthetically, the flared and upward tilted nares reveal an unpleasing nose posture along with an obtuse nasolabial angle.
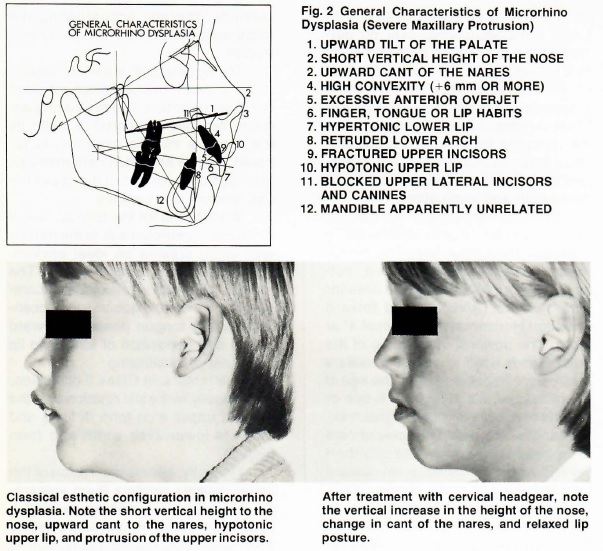
The long, drawn-out maxillary dentition, tapered progressively toward the midline, allows sufficient overjet so that, in resting posture, the lip is carried underneath the upper incisor teeth. Upon swallowing, the patient thrusts the tongue forward to meet the hyperactive lower lip, creates the seal to swallow and, in effect, continues a functional syndrome which often is initiated by the finger, aggravated by the tongue, and perpetuated by the lip. These pressures, directed in a superior direction by the functional aberration of the finger, tongue and lip, retard the vertical drop of the anterior maxillae, thereby accentuating the microrhino dysplasia or maxillary protrusion .
The hyperactive lower lip, resting in the anterior overjet, often retrudes the lower dentition. The protruding anterior maxillae, restricted in width by the caninus muscle complex, is tapered, narrow and often demonstrates blockage or impaction of the upper lateral incisors and canines.
Vault space for the tongue, which is severely restricted due to the narrow arch form, creates an ideal environment for anterior tongue thrust. The narrow, constricted maxillae, accompanied by a narrow nasal vault, accentuate a low tongue position, forward thrust, and apposition of tongue to lip in the act of swallowing.
The molars, in Class II occlusion, are typically in mesial rotation and the tapered upper arch form defines and restricts lower arch width and form (Fig. 3).
Typically, severe protrusion of the upper incisors renders them vulnerable to fracture, as well as causing a hypotonic upper lip (which often is short and thick, labiolingually, due to swollen sebaceous glands), and a functional lip aberration which further promotes the abnormal maxillomandibular relationship.
The most important characteristic of microrhino dysplasia, however, is that it is apparently unrelated to facial growth type. The severe maxillary protrusion characteristics are just as evident in Class II brachyfacial types (strong mandibular growth postures) as in Class II dolichofacial types (weak mandibular growth postures). It is this last characteristic that allows us to select the proper headgear to resolve maxillary protrusions in different growth patterns, as defined by mandibular growth turgor. Although midface growth profiles may appear identical cephalometrically, it is the lower face that usually dictates muscular response to headgear application and, therefore, dictates the type of headgear selected. (This point will be further elucidated and clarified.)
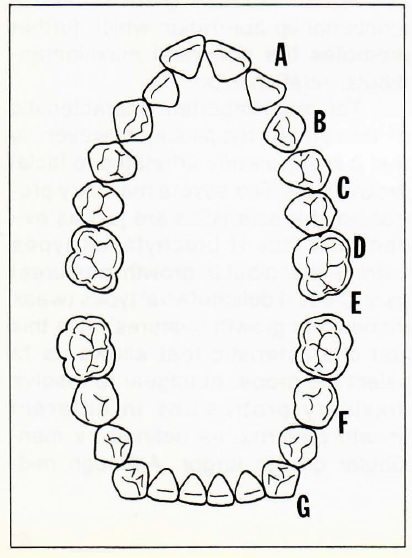
Fig. 3 Arch form characteristics in the microrhino dysplasia demonstrate (A) protrusion and tapering of the anterior arch form that quite often blocks eruption of the upper lateral incisors. The upper cuspid width (B) is narrow and confined by the caninus muscle. Arch widths across the upper bicuspids (C) and upper molars (D) are also narrow in response to their mesial position over the lower arch. The upper molars (E) are in mesial rotation. The lower bicuspids (F) are quite often lingually inclined and the anterior mandibular arch form is flattened (G) with the lower incisors positioned lingual to the lower canines.
Classical Responses With Differential Headgear Therapy
In order to develop an understanding of what reasonably can be expected from the application of
different headgears in different facial types, it is important that a demonstration of classical response to differential mechanics be presented and evaluated.
It is understood that the responses manifested may be excessive (or, in some cases, even undesirable) -- but it is felt that, to a varying degree, these responses are demonstrable in routine clinical cases undergoing similar therapy. By defining, evaluating, and relating the facial type, specific mechanics and treatment responses, it is probable that the clinician will be capable of selecting the proper type headgear, can utilize mechanical application, and expect predictable results.
Due to the wide variations in headgear application (and types), this article will deal with face bow therapy only, with major emphasis on the cervical headgear. It is acknowledged that cervical or combination (directional) face bow therapy are not the only mediums of achieving orthopedic alteration; they are, however, universally recognized forms of headgear application and thus lend themselves to a discussion of the classical responses attained by their use.
Generalized Orthopedic Response With Cervical Headgear Alone
Although the general orthopedic response in the mandible is highly variable, depending upon facial growth type, the maxillae invariably respond in a highly predictable way to a line of force directed at the level of, or below, the rotational center of the maxillae.
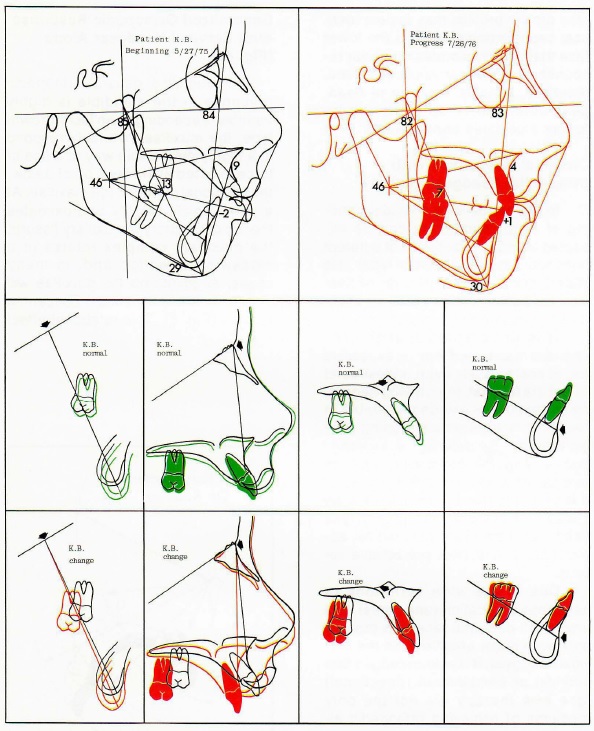
Fig. 4 Cephalometric appraisal of cervical headgear only - 900 grams, 12-14 hours per day for 14 months. Class II division 1 open bite with severe maxillary protrusion, mild microrhino dysplasia and mesofacial growth pattern. Superimposition reveals a mild rotation of the facial axis (negative mandibular rotation) and a considerable orthopedic rotation of the maxillae. The soft tissue nose was seen to cross over at the bridge, lengthen vertically, and change the cant of the nares. Superimposition for the maxillary teeth revealed a slight distal movement and extrusion of the upper molar. The upper incisor was retracted by muscle function. Dental superimposition in the lower arch showed a distal uprighting of the lower molar and normal eruption of the lower incisor.
At a point which roughly approximates the top of the pterygomaxillary fissure, the maxillary complex rotates in a clockwise direction and, in many cases, all points on the maxillae will appear to arc in an almost concentric fashion (Fig. 5). This rotational effect accounts for the reduction in maxillary protrusion, a downward canting of the palatal plane and concomittant nasal changes. The nasal bone, which normally becomes slightly more procumbent with age, pivots downward and backward at the frontonasal suture, with rhinion moving distally.
As the maxillary complex rotates in the clockwise direction, the contiguous sutures of the midface complex that extend through, and include, the posterior buttressing spheno-occipital complex are altered. Quite often, where they can be clearly delineated on the lateral head film, the pterygoid plates are demonstrably tipped distally as the midface is compressed.
As mentioned previously, the most variable orthopedic response occurs in the mandible. In weaker muscular patterns (in general, the dolichofacial patterns) the extrusion of both the maxillary molar and the maxillae causes a reciprocal clockwise rotation of the mandible, opening of the facial axis and mandibular plane, and a diminishing effect on forward chin posture. In extremely weak growth patterns this downward, backward rotation of the chin can completely negate the effect of maxillary rotation, resulting in an even higher face height with detrimental soft tissue strain and functional (muscular) aberration. The effect in more normal and brachyfacial patterns is, however, quite the converse. The strong muscular patterns may elicit some mild mandibular rotation but, from the vectoral standpoint, the amount of maxillary response more than compensates for this mandibular rotation, by three to four times.
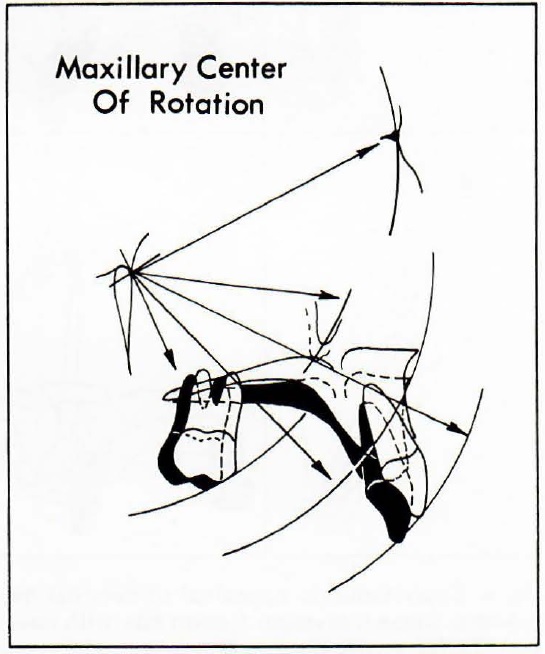
Fig. 5 When a vector of force is applied below the center of resistance of the maxillae (located near the apex of the pterygomaxillary fissure), a rotational orthopedic effect is seen in the maxillae. All cephalometric landmarks appear to arc in a concentric fashion with the apex of the maxillae acting as the center of the radius.
The net effect is that, in weak muscular growth patterns, the extrusive effects of cervical headgear are elicited as a negative response in the mandible (i.e. orthopedic in nature) and, in strong muscular growth patterns, the extrusive forces of the cervical headgear are seen as responses in the dentition (i.e. orthodontic in nature).
Generalized Orthodontic Response With Cervical Headgear Alone
The downward and backward pressure of the cervical headgear, when applied to the upper molars alone, intermittently extrudes these teeth. The first molars often will pivot around the cortical crypt of the erupting second molars. This response, however, is dictated more by the muscular pattern, the length of the outer bow, the occlusion of inclined planes (upper molar vs. lower molar) and the length of wear each day. It is observed that often there is no tipping of the upper molar at all, even with cervical headgear.
The upper incisor will tip lingually (from its apex). It is theorized that this response takes place after overjet has been reduced enough to allow the everted lower lip to close over the upper incisor, rather than on the lingual side of that tooth, creating a functional retraction of the upper incisors.
The lower molars upright and often move distally when carried by the incline planes of the extruded upper molar, which also is being carried distally. The vertical eruption of the lower molars is usually within normal ranges and it is ultimately the net result of lower molar eruption and upper molar extrusion that defines the effective rotation of the mandible.
The lower incisor, without the inhibiting effect of the lower lip, will quite often tip labially as the upper and lower lips start to reach equilibrium, and the tongue starts to dominate the labial positioning of these teeth.
Although the same maxillary response can be gained with several types of headgear combinations, the patient acceptability of the cervical headgear, as well as the overall reciprocal response which occurs in the mandible, make the cervical headgear the appliance of choice in cases of severe maxillary protrusion in the normo-facial through brachyfacial range. It is the ideal appliance in the early treatment experience where a minimum of banding is wanted and, due to the intermittent nature of its application, also lends itself to application in the later stages of treatment.
The Reverse Response
In those cases where a cervical headgear is utilized in combination with a lower utility arch, the orthopedic response in the maxillae will result in the classical rotational response. However, quite a different orthopedic response can be shown in the mandible. The mandibular plane and facial axis will be somewhat stabilized and, in strong muscular patterns (brachyfacial types), the mandible may rotate in a counterclockwise direction, resulting in a closure of the lower face height, mandibular plane and facial axis.
This unusual orthopedic response in the mandible can be traced back to the dentition, and its response to this combination of mechanics. The extruding upper molar will, as it is moved distally, again pick up (through incline plane effect) the lower molar and upright that tooth in a distal direction. This effect is enhanced by the tipback in the utility arch. As the lower molar uprights, the distalizing force is translated, through the utility arch, to the lower incisors. These teeth will first intrude and then start to follow the lower molar distally. If the lower arch is not held forward, eventually the lower incisor will become encased in the heavy cortical bone at the planum alveolare of the symphysis and further intrusion becomes difficult. At this point, as the action of the utility arch continues, its overall response is applied toward retarding the normal vertical eruption of the lower molar (Figs. 6 and 7).
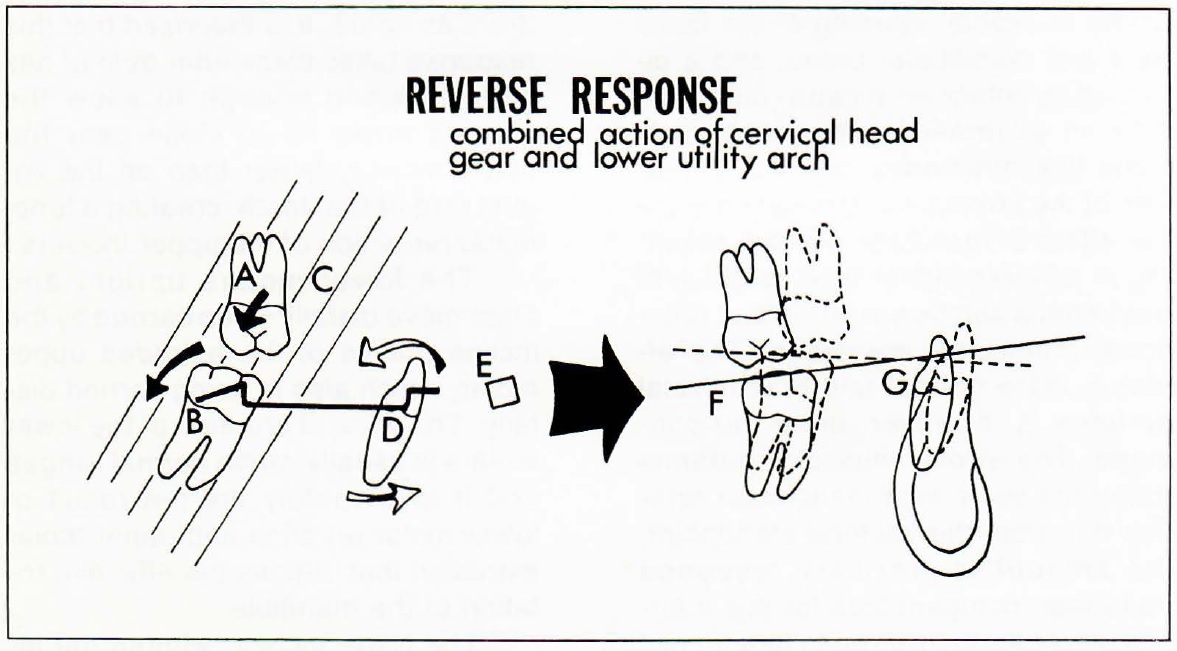
Fig. 6 When the upper molar (A) is extruded and distalized in an intermittent fashion, its inclined planes act to upright and distalize the lower first molar. This is accentuated by the tipback in the utility arch (8) and the labial root torque at the lower incisor (D). The vertical pull of the masseter and pterygoid muscles (C) acts to stabilize lower molar eruption and limit upper molar extrusion. The labial root torque in the lower utility arch (E) also allows the lower incisor to avoid the planum alveolare as it intrudes. The net result of these mechanics will show a limited eruption or intrusion of the lower molar (F) and a distal movement of the lower incisor (G), with concomitant changes in the occlusal plane.
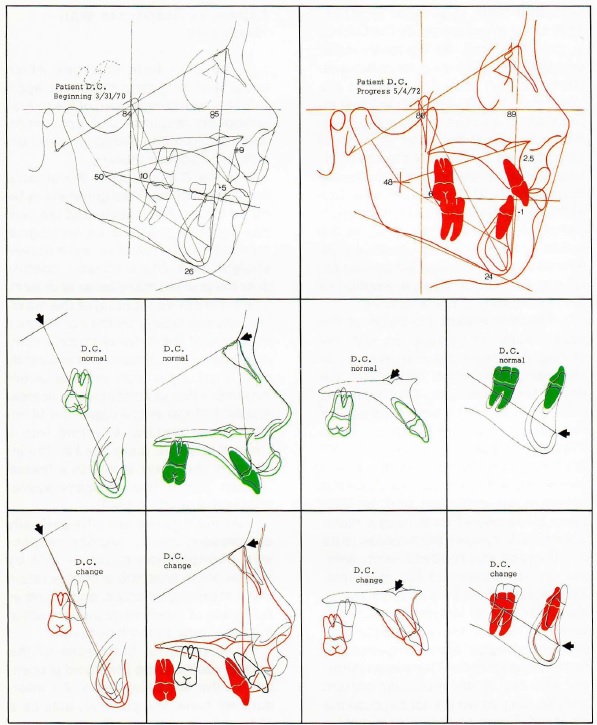
Fig. 7 Cephalometric appraisal of cervical headgear - 900 grams, 12·14 hours per day for 16 months, 8 hours per day every other day for 6 months - in conjunction with lower utility arch. Class II division 1 severe maxillary protrusion and mesofacial growth pattern. Superimposition reveals a closing of the facial axis and considerable orthopedic rotation in the maxillae. Superimposition for the maxillary teeth shows extrusion and distal root tipping of the upper molar and a functional retraction of the upper incisors. Dental superimposition in the lower arch reveals distal uprighting and intrusion of the lower first molar. The lower incisor was slightly intruded and retracted with the lower molar as a function of the utility arch (reverse response).
The intermittent extrusion of the upper molar, in conjunction with the strong muscular pattern, results in stabilizing (and often distalizing) the entire lower dentition. This action is referred to as the reverse response of the lower utility arch and can be utilized to set back the lower arch, for anchorage and for arch length. In essence, this action compensates for the upper molar extrusion and, in fact, takes place only when the upper molar is extruded. It allows the maxillae to be compressed and rotated distally without undue rotation of the mandible. This is almost entirely a functional or muscular type of response and is adverse to our common concepts of a posterior wedge with compensatory mandibular rotation. There is an inherent stability in the muscular pattern and, so long as we do not override the ability of the musculature to maintain this stability, we can certainly control the unwanted side effects of cervical headgear utilization. These side effects, which we have historically thought of as detrimental.(especially that of upper molar extrusion), may be the very factors that create a most desirable response in the lower arch!
Expansive Responses With Headgears
The arch form changes which occur with long-term headgear application are an integral part of the overall orthopedic response and account for some of the often unrecognized benefits of headgear therapy.
In the Class II pose, the anterior portion of the maxillae generally is tapered toward the midline and the buccal occlusion would be in lingual crossbite if the maxillae were moved straight back into a Class I position over the present mandibular arch form. The progressive tapering of the maxillae, caused mainly by the constrictive influence of the caninus muscle complex against the upward and outwardly positioned upper arch, creates an environment that is conducive to ectopic eruption of the entire upper dentition. The upper molars, erupting into a Class II position, are guided by the inclines of the lower arch into a mesial rotation, further limiting space available for the erupting teeth.
As the maxillae are orthopedically compressed distally, two basic expansive phenomenon occur-- one by means of the anatomical configuration of the maxillary complex, and the other by means of mechanical adjustment of the inner bow of the headgear.
The posterior buttresses of the palatal vault are the pterygoid processes of the sphenoid bone. An intermediary bone, the palatine, acts as a slip joint, or area of adjustment, between the maxillary and sphenoid bones. Anatomically these three bones form an outward bevel just distal to the maxillary tuberosities. Any force that places a distal compression on this complex simultaneously creates an expansive influence at the midpalatine suture. As the palatal vaults slide down the outward sutural bevel, a midpalatal dysjunction of significant magnitude can be demonstrated (Fig. 8).
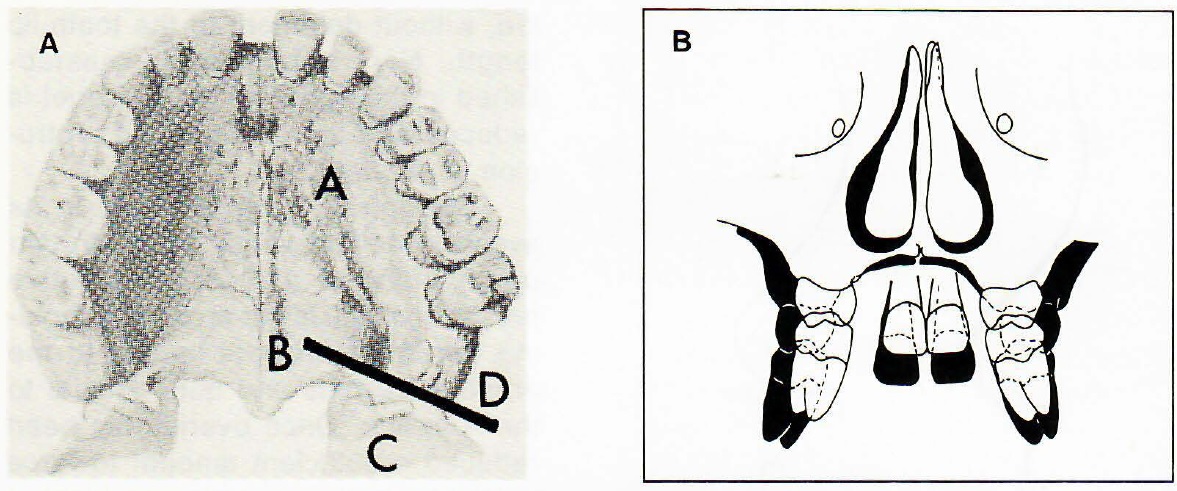
Fig. 8 A. The palatine bone (B) forms an outward bevel between the maxillary tuberosity and the sphenoid bone (C). When the maxilla is compressed distally, it moves down the outward bevel (0), and a natural expansion occurs in the upper arch. B. When superimposed at foramen rotundum in the frontal plane, treatment with cervical headgear creates width increases in the nasal cavity, mid palatal dysjunction, expansion of the maxillary alveolar process, and reciprocal expansion of the lower arch.
If, however, the maxillae are tied at the midline by banding and archwires, much of this natural expansion is eliminated. In most cases this expansive response is beneficial in creating arch form characteristics that are conducive to better tooth alignment.
From the mechanical standpoint, a progressive widening and tipping of the alveolar base is accomplished by a widening of the inner bow of the face bow. This expansive process provides for several distinct considerations:
1. Reciprocal expansion of the lower arch. As the upper arch form slowly changes, a natural widening of the lower arch also occurs. A more normal muscle function, one without the strain associated with the severe protrusion, begins to act on the dentition as the factor creating changes reciprocal to those expansive alterations occurring in the maxillae. These expansive changes can be observed on the lateral head film as anterior movement of the lower incisors. In the horizontal plane, increases in arch width occur.
2. Preventing impacted second molars. When the upper first molar is translated distally without expansion, the incline planes of that tooth start to reciprocally constrict the lower molars, carrying them to the lingual. If this occurs early, prior to second molar eruption, the lingual movement of the lower first molar is expressed in the second molar, either to impact that tooth or to force it to the buccal . It is worthy of note that the best way to prevent impaction of the lower second molar is to keep the headgear inner bow liberally expanded .
Soft Tissue Esthetic Changes
Normal growth of the soft tissue nose, evaluated by superimposing along the Basion-Nasion line at Nasion, reveals a concentric type of growth (Fig. 9). Following a pivotal orthopedic alteration of the maxillae, the soft tissue nose crosses over at the bridge, the tip becoming less procumbent and, with muscular attachment to anterior nasal spine, the nose can be seen to lengthen vertically as the anterior palatal plane drops.
The upward cant of the nares often is tipped down in the front and the nasolabial angle is seen to become more acute (all desirable esthetic reactions in the microrhino dysplasia). The upper lip, often atrophic due to lack of function, also will pivot with the maxillae, without detriment to the tooth-lip length. Normal function is reestablished in the upper lip once overjet is reduced and the strain of the protrusion is alleviated.
The lower lip, hypertonic in its everted position under the protruded upper incisors, places a restrictive pressure on the lower arch, often holding the lower incisors lingual to the erupting cuspids and quite lingual to the APo line. Once overjet has been reduced a sufficient amount to force out the lower lip (its resting position), it begins to restrict the upper incisors, while allowing the tongue to exert pressure on the lingual of the lower incisors. The net result, as demonstrated by superimpositional analysis, is that there is often a functional retraction of the upper incisors and a functional advancement of the lower incisors.
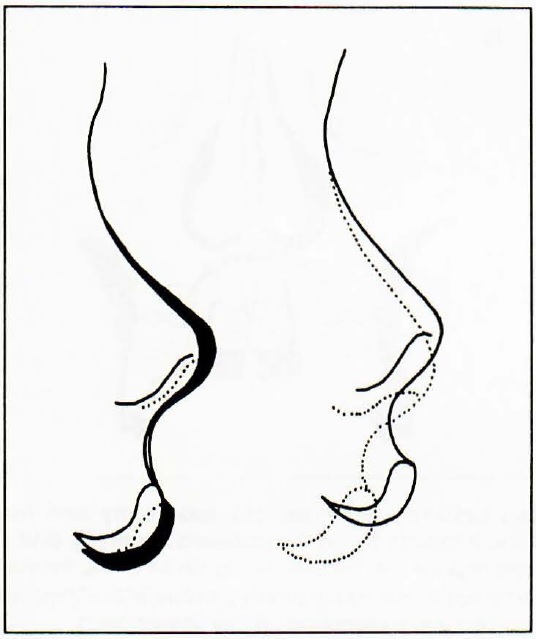
Fig. 9 Changes in the overall position and growth of the soft tissue nose are evident following maxillary orthopedic rotation. With normal growth (left), the soft tissue nose is seen to grow concentrically approximately 1 mm per year at the tip. The cant of the nares remains unchanged. Following headgear therapy (right), the nose is seen to cross over at the bridge, lengthen vertically, and the upward cant to the nares is tipped down to a more horizontal position.
Reduction of the maxillary protrusion also allows the soft tissue chin, dominated by the upward strain of the mentalis muscle and the constricting influences of the quadratus muscle, to distribute evenly over the symphysis.
Tongue thrust, a natural phenomenon when open bite exists (due to the maxillary position), can also be alleviated when overjet is reduced enough to prevent apposition between the everted lower lip and the forward thrusting tongue (Fig. 10).
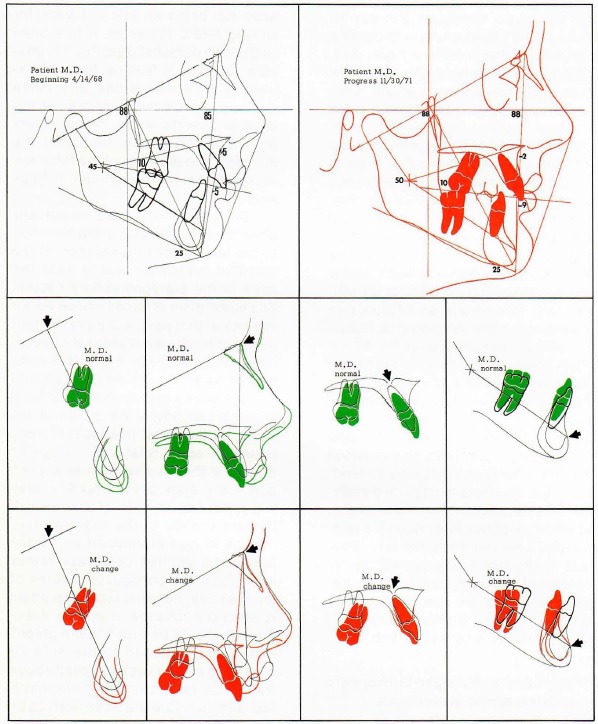
Fig. 10 Cephalometric appraisal of cervical headgear - 900 grams, 12-14 hours per day for 24 months- in conjunction with lower utility arch worn 16 months (extreme overtreatment). Class II division 1 with moderate maxillary protrusion, mild microrhino dysplasia, mesofacial growth pattern, and retrusive lower arch. Superimposition reveals a stabilized mandible and classical orthopedic rotation of the maxillae. Superimposition for the maxillary teeth reveals an extreme extrusion and distal tipping of the upper molars and mild retraction of the upper incisors. Dental superimposition in the lower arch demonstrated an extreme distal positioning of the lower arch following a reverse with a lower utility arch. The net result of this combination of mechanics over a prolonged period of time was substantial flattening of the midface and retrusion of the entire denture, further worsening the esthetic problem. The distal movement of the lower arch following the maxillary orthopedic rotation was profound, and none at the Class II occlusion was corrected. The extreme overtreatment resulted in a detrimental overall orthopedic response.
Generalized Response With Combination Type Headgears
In those cases where the severe maxillary protrusion exists, but the growth of the mandible is weak (dolichofacial patterns), it often is desirable to create a rotational orthopedic effect in the maxillae and at the same time maintain mandibular stability. Cervical type headgear therapy in these cases often results in excessive extrusion of the maxillary molar and, without the retarding effect on the lower arch created by a strong functional response, the mandible rotates in a counterclockwise direction. Long-term directional headgear therapy (part time wear), where the force is applied below the center of resistance of the maxillae, again allows the classical orthopedic response, but without the upper molar extrusion. If the force applied moves the maxillae distally without overriding musculature, and is in conjunction with mandibular growth, the lower face height can be closed or maintained while achieving a reduction of the maxillary protrusion. All too often, however, the distal compression of the maxillae on a short-term basis (fulltime wear) will result in an adverse mandibular response, even though the upper molar is intruded. The distal movement of the maxillae is so defined that, from the purely geometric standpoint, the mandible must pivot distally. Adverse facial change in these cases, however, depends more upon the relationship between the upper and lower face height than it does on mandibular rotation. If the lower face height is decreased (i.e., more maxillary rotation than mandibular rotation), the overall change will be a beneficial one.
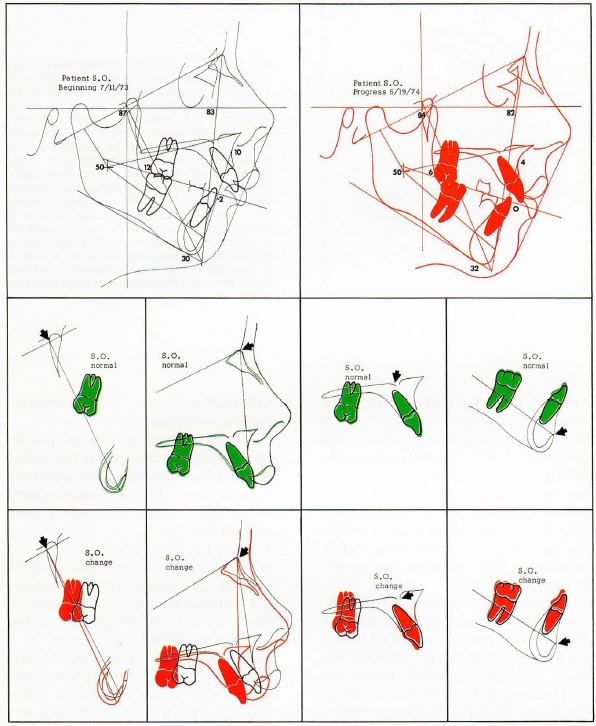
Fig. 11 Cephalometric appraisal of combination headgear- 1000 grams hi-pull, 500 grams cervical pull, 20 hours per day for 9 months - in conjunction with upper utility arch. Class II division 1 open bite with severe maxillary protrusion, microrhino dysplasia and dolichofacial growth pattern. Superimposition reveals a 5° rotation of the facial axis (negative mandibular rotation) and a considerable orthopedic rotation of the maxillae. The maxillary rotation equaled the mandibular rotation to maintain the lower face height at 50°. Superimposition for the maxillary teeth revealed intrusion of the upper molar and slight retraction of the upper incisors, indicating that almost the entire Class II correction occurred by orthopedic movement of the maxillae. Mandibular superimposition shows a normal eruption of the lower arch. Even though the upper molar was intruded, the mandibular rotation occurred as the maxillae was compressed distally into the wedge of occlusion, not allowing adequate time for mandibular growth or muscular stabilization.
Differentiation Between Orthopedic and Orthodontic Movements
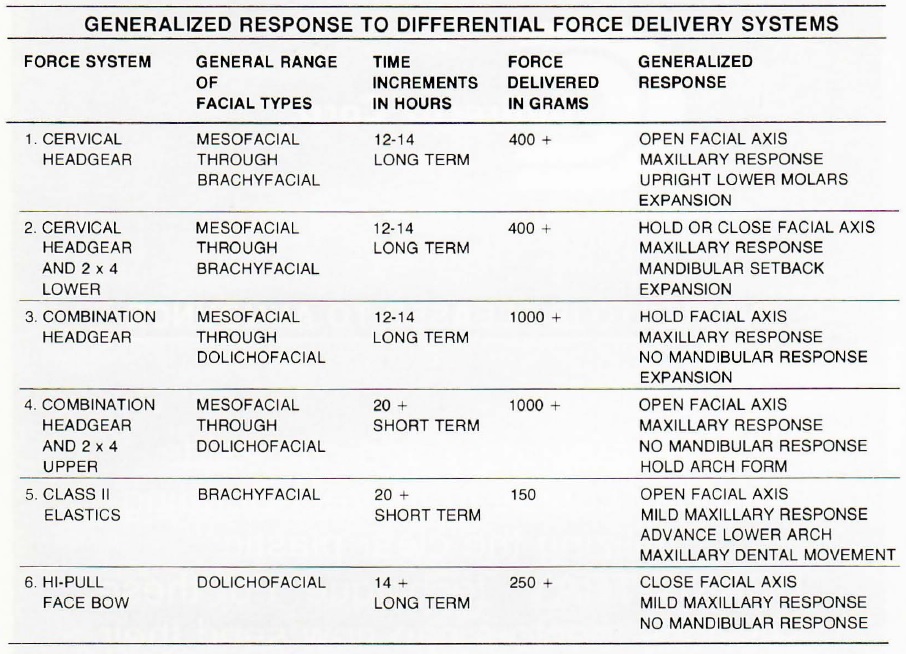
It has been suggested that the major determinant for creating changes in the jaws themselves (orthopedics) versus changes in the dentition (orthodontics) is that of force amount. Studies have shown that forces above the 400-gram level tend to be adequate for opening sutures and overriding muscular pullback, while not being an efficient force for moving teeth. However, it has been sufficiently demonstrated that it is possible to apply a full-time force of extremely high magnitude and move nothing except the dentition, if the force is oriented in the proper direction. It is felt at this time that the direction and duration of the force are as significant as the amount of force applied.
Direction becomes important when the overall vector of the force lies below the center of resistance of the maxillae, which is located near the apex of the pterygomaxillary fissure. Any summation of forces whose vector lies below that point will have the tendency to produce a rotational effect of the maxillae (Fig. 12). It is, in fact, quite difficult to get an overall force applied to the maxillae that is above that level (since it lies above the crown of the skull), so that most headgear therapy results in some rotational orthopedic change in the maxillae. Forces applied above the apex of the maxillae have the tendency to restrict downward, forward growth of the maxillae (i.e. change in growth amount) but, since the forces applied compress rather than shear the contiguous sutures of the maxillae, no great rotational effect is seen (i.e. change in growth direction). It should be noted that high-pull headgears attached to the anterior arch have a force vector applied above the center of resistance of the maxillae, and therefore are more likely to be growth restrictive than rotational in nature.
Force duration, as defined by continuous versus intermittent pressures, also plays a significant role in the type of movement achieved. Although it may be argued that excessive force levels create a pathologic or backward type of resorption in the dentition, it can be demonstrated that any continuous pressure, regardless of amount, has the tendency to move the dentition. It will also move the jawbones, if the force is applied in the downward, backward direction. One-half of the total Class II correction resulting from use of face bow therapy typically is accounted for by tooth movement, and the other half by orthopedic movement.
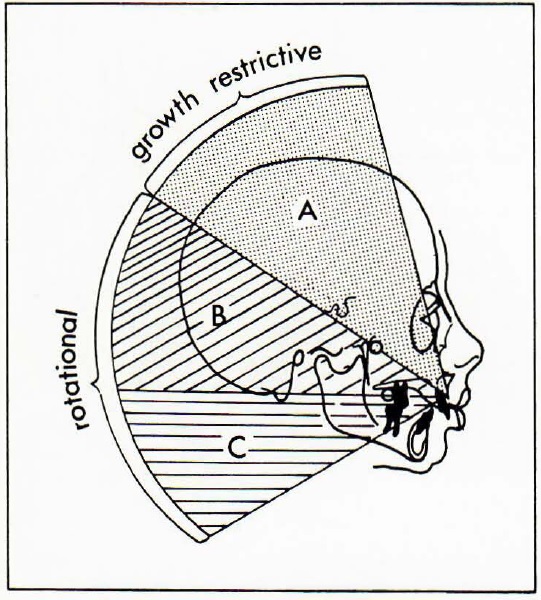
Fig. 12 Forces applied to the maxillae through the face bow are either growth restrictive (i.e. retard the downward, forward growth of the maxillae) or rotational (i.e. tip the maxillae downward and backward) in nature. The vectoral sum of forces (A) that lies above the center of resistance of the maxillae will be growth restrictive. The vectoral sum of the forces that lies below the center of resistance of the maxillae (8 and C) will produce rotational effect. A vectoral sum of forces that lies above the center of resistance of the upper molar (8) will produce a rotation of the maxillae and will also intrude the upper molar. A vectoral sum of forces that lies below the center of resistance of the upper molar (C) will provide a rotational effect on the maxillae but will extrude the upper molar.
In general, where orthopedic rotation of the maxillae is desired, a heavy force (400 grams+) is applied below the center of resistance of the maxillae in an intermittent manner. Note also that this type of force application gives a wide variation of face bow combinations with the main criterion of selection being whether or not we desire to extrude, hold, or intrude the upper molar. When the same force direction is applied in a heavy, continuous manner, often the molar will move so far distally that time is not given for gaining orthopedic change. Even this can be eliminated by tying the upper molar to the upper incisors, thereby increasing the anchorage in the maxillae.
Another factor contributing to orthopedic type movement is the nature of the bone supporting the dentition. The character of the bone surrounding these teeth varies, depending upon several factors.
1. Sinus Development.In some young children, maturity of the sinuses occurs early in life and a heavy 2-3 mm thickness of cortical bone on the sinus floor will encase the upper first molar. When this occurs in a young child (with active sutural adjustments), the movement of the maxillae is enhanced by the inability of the upper first molar to move through this cortical support. This sinus relationship occurs generally in cases with low alveolar height and early sinus maturity, and can easily be detected on lateral head film.
2. Distal Root Tip. Any distal pressure to the upper first molar has the tendency to allow that tooth (anatomically) to pivot and tip at its apex, around the cortical crypt of the erupting second molar. By controlling and/or counteracting the tendency for distal crown tip, orthopedic movement of the maxillae is enhanced while orthodontic movement of the molars is minimized. We have noted that use of a long outer bow canted up to the ala of the ear specifically counteracts the tipping effect. When the orthopedic pressures are exerted intermittently over a long period of time, physiologic override by virtue of incline planes and muscular rebound has shown an ability to move the upper molars distally without tipping, even with use of cervical headgear.
3. Stacking Factors. By increasing our anchorage in the maxillae, orthopedic response can be enhanced. One must remember that, when a headgear is placed to the upper molars alone, we are in effect applying force against six teeth in total (first, second, and third molars on both sides). By banding more of the dentition, the root surfaces (and stacking effect) may be enhanced. Full-banding with a cervical headgear has many drawbacks, however, and most full-banded headgear therapy is reserved for directional headgear.
4. Sutural Freedom.The most significant factor in defining orthopedic versus orthodontic type movement is the relative ability of the contiguous sutures of the maxillae to adjust to expansive, compressive and shear type pressures. This is directly related to age. The maxillae shows an adjustment type of bone growth that becomes quite immutable, generally after puberty. Most very defined orthopedic changes are relegated to youngsters from birth to 14 years of age. A true orthopedic type of response in the mature skeleton is quite rare and cannot be counted upon as a medium for correction of the Class II malocclusion.
Mechanical Application of The Cervical Headgear
Since a major tool for creating an orthopedic type of response in the growing child is the cervical headgear, discussion of its mechanical application is in order.
When specific orthopedic rotation and expansion in the maxillae is desired, as well as the reciprocal responses that occur in the lower arch, the following headgear adjustments are recommended:
1. Force Level. A force level above 400 grams is ideal. From the practical standpoint, it is difficult to apply the average neck strap with a force much under 400 grams. In most patients, forces up to 1000 grams can easily be tolerated and should be applied when possible.
2. Intermittent Wear. When the cervical headgear is worn in an intermittent manner, several important advantages are gained:
(a) A heavy, intermittent force to the upper molars will create a sclerotic condition around the roots of these teeth. The overall effect is that tooth movement is decreased and orthopedic movement is enhanced by the relative inability of these teeth to move through the hyaline type bone.
(b) Rebound, also, is allowed to occur in an intermittent manner, which results in stability in the mandible, especially in the stronger growth trends. When utilized in conjunction with a lower utility arch, this muscular rebound acts to influence a distal movement of the entire lower dentition. The slow, methodical expansion of the maxillae also allows the arch form and width changes that are quite often seen in the lower arch. Although the pivotal rotation of the maxillae can be accomplished quite efficiently with continuous headgear wear, it is the intermittent wear which gives time for physiologic rebound, muscular adaptation and arch form and width changes.
(c) Since more growth occurs at night and more function occurs in the day (where the teeth come into contact upon swallowing), it is ideal that the cervical headgear be worn mostly in the evening and sleeping hours.
(d) Patient acceptability is enhanced by allowing mainly nighttime wear. Most children are amenable to wearing the headgear over a longer period of time on that basis, while full-time headgear wear is a difficult proposition for most youngsters.
3. Outer Bow Length and Position. To minimize the tipping of the upper molar, a long, rigid outer bow extending past the molars is suggested. The outer bow should be tipped up 15°, approximately to the ala of the ear, to bring the resultant force vector above the center of resistance of the upper molar. This will prevent "propping open" the bite by excessive tipping at the molars and will maximize the orthopedic response by pitting the roots back against the cortical crypt of the upper second molar.
4. Expansion-Rotation. As the maxillae are rotated downward and backward, the distal movement of these bones will bring them into crossbite with the lower arch. It is essential to continually expand the inner bow of the cervical headgear, not only to correct the tendency to crossbite but also to allow a functional development of the lower arch. In addition, the mesially rotated upper molars should be rotated distally to assist in the achievement of Class II correction, and to accomplish their final ideal rotation. From the practical standpoint, a flexible inner bow is suitable for cervical headgear, as it is a good medium for these expansive and rotational changes. Each child is instructed to expand the inner bow 2 cm before insertion of the headgear. Distal rotation of the upper molars will occur as a straight distal force is applied to the buccal of the upper molar, and these teeth are allowed to pivot around their large lingual roots. At each appointment, a headgear plier is utilized to progressively rotate the distal legs of the inner bow, thereby allowing this distal rotation to occur.
5. Freedom of Movement of the Maxillae. It is of prime importance that the cervical headgear be utilized by itself in the upper jaw. The overall changes we have discussed take place in light of several factors:
(a) As the rotation of the maxillae occurs, the overbite increases as the anterior portion of the maxillae drops. When the upper incisors contact the lower incisors, a traumatic occlusion ensues that generally will be avoided by the patient and restriction of function occurs. This restriction of function allows the buccal segments to extrude and the mandible to reciprocally rotate distally. This response points out why the patient with microrhino dysplasia with open bite, who has good muscular rebound, responds so well to cervical headgear therapy. The maxillary rotation closes the open bite while normal function in the mandible maintains its relative stability.
(b) Banding the upper incisors and tying them to the upper molar compounds this problem. Any distal tipping in the upper molars is translated directly to the upper incisors as an extrusive force. As mentioned previously, extrusion of the maxillae will not detrimentally affect the lip-to-tooth relation. On the other hand, extrusion of the upper incisors can create a "gummy" smile. To allow the ideal orthopedic manipulation of the maxillae and maximize the reciprocal rebound responses in the mandible, it is imperative to employ the principle: "Correct the overbite before correcting the overjet". The most detrimental effects we have observed with cervical headgear therapy occur when a cervical headgear is applied to a full-banded upper arch in deep bite.
(c) We, in effect, negate many of the expansive characteristics of cervical headgear application if we tie the two maxillae together at the midline. The free, natural outward movement of the maxillae as they are compressed in a distal direction is restricted, as well as any reciprocal arch form and expansive changes that we could expect to see in the lower arch. By not tying the maxillae together with full-banding, the arch form changes create space for the erupting lateral incisors and cuspids.
Factors Causing Excessive Mandibular Rotation
The cervical headgear has been maligned for its role in negative mandibular rotation, to the extent that some have lost their belief in the inherent value of this direction of headgear force, in spite of cases where its overall response could be considered ideal. Several inherent factors are mainly responsible for this over rotation of the mandible and they should be discussed.
1. Weak Muscular Pattern. In cases where the rebound musculature of the mandible is not adequate to maintain overall mandibular stability when the headgear is worn on an intermittent basis, the extrusion, tipping, and distal movement of the upper molar overrides both the functional and growth ability of these cases to maintain stability. These are typically the patients with high mandibular plane and showing vertical growth. The overall pull of the masseteric-pterygoid muscular complex is in a direction more forward than the vertical direction which we see in most normo-facial and brachyfacial growth types. Stimulation of a functional muscle response by gum chewing, a textured diet, and generous arch widening of the inner bow (to increase salivation) is recommended .
2. Not Retarding Effective Eruption of The Lower Molars. When there is extrusion of the upper molar as it is compressed distally, if at the same time the lower molar is allowed to achieve its normal eruption potential, some negative rotation of the mandible will occur. In certain facial growth patterns this may be an acceptable or even desirable development of the lower face height. Retarding the normal upward, forward development of the lower molar will have a tendency to counteract the overall rotational effect on the mandible, while still allowing the orthopedic response to take place in the maxillary complex. In those mesofacial through brachyfacial cases where utilization of the cervical headgear is contemplated, stabilizing the eruption of the lower dentition through the use of a lower utility arch is recommended, when mandibular stability is a goal of treatment.
3. Severe Tipping of Upper Molars. Extreme extrusion and tipping of the upper molar props the mouth open by elongating the mesial inclines of those teeth. Maintaining a slight upward cant to the outer bow will minimize this tipping effect. Severe tipping also is seen in those cases where effective growth has been completed and there is an inability of the posterior buttresses of the maxillae to adjust to the compression of the upper jaw.
4. Full Arch Therapy Without Freeing Anterior Occlusion-- Incisal Trauma. A sequelae of contemporary orthodontic therapy (where round arch leveling is utilized) is that interferences are created at the incisors as the maxillae are rotated distally, worsening the deep bite problem and creating incisal interferences which ultimately result in a negative rotation of the mandible. It then becomes a situation where no effective correction of the Class II condition can occur as the maxilla is simply chasing the mandible distally. In those cases where deep bite exists, it is suggested that overjet be created to allow the anterior maxillae freedom of movement without accentuating the incisal trauma. Effective movement of the teeth and/or the jaws can occur only when they are freed from negative influences.
5. Full-time Cervical Headgear Therapy. Since stability of the mandible is dictated by muscular rebound and growth, treatment that overrides or limits this rebound/growth phenomenon ultimately will result in rotation of the mandible. It is the extrusion of the upper molar that can allow beneficial effects in the lower arch, but this will occur only in cases that exhibit a propensity for strong muscular rebound.
Summary
Orthopedic alteration of the skeletal complex is a major tenet of the Bioprogressive Therapy. Prior to the defined orthodontic movements to create the ideal occlusion, an acceptable symmetry between the upper and lower jaws is needed to allow the ultimate framework upon which an esthetic, functional, and stable occlusion can be built. As demonstrated, we have the tools not only to hold or direct growth, but to physically manipulate the position of both jaws. A rotational effect in the maxillae, sometimes accounting for a 6 mm to 8 mm movement away from the normal growth direction, is possible with the proper application of forces.
It was shown that any force directed below the center of resistance of the maxillae will account for this rotational effect. Control of the upper molar is defined by our ability to place a directive force to that tooth. Extrusion of the upper molar can be quite beneficial in gaining some reciprocal tooth movement in the lower arch when it is intermittently extruded and function is allowed to work against a lower banded unit (utility arch). Those cases which allow functional rebound are ideally suited to cervical headgear therapy.
Inasmuch as the broad spectrum of Class II malocclusions are most predominantly in the mesofacial to brachyfacial ranges, some detailed discussion of the principles of cervical headgear therapy were discussed.
In the scheme of treatment planning, a defined orthopedic alteration of the jaws is the benchmark of creating harmony in both the occlusion and the esthetic profile.


