JCO Visits Rocky Mountain Data Systems
The Editor went to Sherman Oaks, California to visit Rocky Mountain Data Systems to discuss computerized cephalometric analysis with its President, Bob Schulhof, and to try to clarify what this service is and of what value it might be in case analysis and treatment planning.
JCO What is the objective of your system?
MR. SCHULHOF To provide the doctor with a feasible treatment objective.
JCO Based on what?
MR SCHULHOF Based on a mathematical model. There were about 200 different decisions that had to be made to construct a complete model for orthodontic diagnosis. Each has been tested in a research project by orthodontic graduate students on treated cases that have been out of retention many years.
JCO Is your model based primarily on Ricketts' theories?
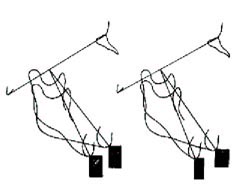
MR. SCHULHOF Yes. Ricketts' method takes into account the expected direction of growth for the individual patient, based upon the finding that certain proportions of the face tend not to change their shape with growth. Growing the patient according to his given configuration, takes his individuality into account (Fig. 1).
There are groups of patients that don't behave according to the normal rules and we are able to pick two out of three of these in advance. We find that the computer is 80% accurate in predicting the amount and direction of growth of the chin, no matter what the original facial pattern--open bite, normal, or Class III. Using average increments, the accuracy drops way down on the extremes.
JCO Predicting chin growth is most important in the extraction decision and also in deciding on the amount of upper distal movement and the amount and kind of headgear.
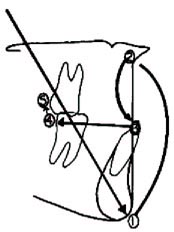
MR. SCHULHOF If you know where the chin will be at the end of treatment, you will know how much to move the maxilla. If you know where the maxilla and the chin will be, you have a guide for placing the lower incisor. Once you know where the lower incisor is, how much arch length shortage you have, and gain or loss treating to the ideal arch form, you know where the lower molar is going to be. When you know where the lower molar is going to be and you wish a Class I molar relationship, you know what you must do with the upper molar. It all started with the prediction of the growth of the chin (Fig. 2).
But, you cannot isolate chin growth as an independent factor. This is a whole system in which no factor can be isolated. Those who look at a few factors, without seeing the interrelationship of the factors, are going to make more mistakes. It is the interactions which gang up on you.
In borderline cases, the interrelationships are especially critical. The difference might be in estimating the distance the upper molar needed to be moved distally. There are some limitations on upper molar distal movement and if the doctor were to be aware beforehand of how much was required, he might decide that it was excessive and therefore extract.
JCO In some borderline cases, the estimate of the probability of third molar eruption with or without extraction might affect the diagnosis.
MR. SCHULHOF If you have 20mm of space between the center of the ramus and the distal of the second molar at maturity, there is very little chance for the third molars to erupt in good occlusion and about an 85% chance of impaction. On the other hand, if you have 30mm of space, the chance of impaction is less than 10%.
We can predict this space in eight-year-olds to a standard error of 2.8mm. Hence, we may predict the likelihood of eruption of third molars at age eight. If their chance of eruption is small, they may be enucleated which I understand is a relatively simple procedure at that age. The earlier they are removed, the less chance of interfering with orthodontic treatment, the less likelihood of a traumatic situation or damage to the second molar.
JCO How do you decide if a patient is a good grower or a poor grower, or a vertical grower or a horizontal grower?
MR. SCHULHOF We don't attempt to pigeonhole people. We have a growth model which amounts to growing each person down his own facial axis. The amount of growth depends on the skeletal age of the patient using a wrist film. There have been different increments of growth shown as an expectation of each age group. The direction of growth is along the facial axis which, with minor modifications isn't going to change. Therefore, rather than saying this person is a good grower and this person is a poor grower, we grow each person his own expected amount and direction.
JCO How about people out on the ends of the distribution curve? Are they also growing down their facial axis?
MR. SCHULHOF Yes, with a few exceptions that we are now able to recognize after doing thousands of predictions. When you really start getting out toward the ends, a patient who has a very square jaw and a long condyle head and a wide jaw is more likely to close his facial axis. If the computer sees this combination, it would close the facial axis, depending on how severe the differences were from average. If, on the other hand, we see a short condyle head, an open mandible, and a narrow mandible, we would expect the facial axis to open, and the computer would react accordingly.
JCO Are there other kinds of cases, such as Class III's and maybe division 2's, where the rules are off?
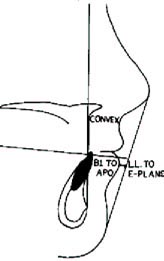
MR. SCHULHOF There is a type of Class III with an abnormality of the posterior cranial base which causes porion to be forward, the ramus to be forward and Basion to be down and forward. When we see these factors in combination, we give more growth in the mandible and less in the cranial base. (Fig. 3).
I believe division 2's are sometimes off because you have a distally displaced condyle. When you unlock the lower jaw you can get an immediate 2mm of forward movement of the chin. You might even get an activator effect having freed the condyle from being trapped against the fossa. I think a 20º laminagraph could pick out these patients.
JCO I'd like to see that study done, because I don't think I have observed that effect in division 2's, although I may not have seen enough division 2's.
The practical value in growth prediction is in helping to formulate a treatment plan and in being able to anticipate growth on the one hand and the effects of treatment on the other. Dr. Ricketts has given us a method to distinguish between the two (JCO April 1975). In your system, how is growth prediction applied to treatment planning?
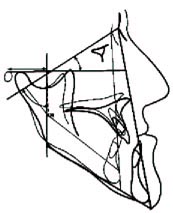
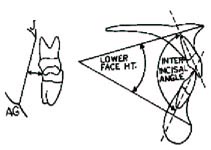
MR. SCHULHOF Knowledge of growth without treatment is of very little value in drawing up a treatment plan. We must change this untreated growth prediction into a visual treatment objective, which shows where we wish to be at the end of treatment as a result of growth and treatment. Many doctors now plan treatment assuming no growth and, if it occurs, it is a safety factor. Therefore, expectation that growth may be helpful or not may influence him one way or the other in a borderline situation. Growth is treated as an isolated input. What I am proposing is what Ricketts and Holdaway have proposed for many years-- that the most useful way of incorporating an estimate of growth into your treatment plan is by drawing up a complete visual treatment objective which incorporates your treatment objectives and treatment effects into the grown face (Fig. 4).
JCO When you do that, you relate the individual to norms and that is the stumbling block for many orthodontists who say that they do not treat their patients to averages.
MR. SCHULHOF Well, people who stray very far from the norm, far from the average, are not accepted by society. If you are within one standard deviation of normal, you are in a safe place and I would take one standard deviation as being as far as I am willing to go (Fig. 5).
JCO Let's assume that somebody extracts 20-30% of his cases, that he was not entirely against extraction, what kinds of things would cause him to go beyond one standard deviation?
MR. SCHULHOF He might have a situation with a perfect lower arch, but with the lower incisor to APo at +4mm. The cephalometric limit of one standard deviation is +3, but he just cannot see breaking up the lower arch for that 1mm. That might be one of the times the orthodontist is quite justified in not going along with the norms. We have to account for this in the computer and extend our borderline in cases of an uncrowded lower arch.
JCO What are your limits in such cases?
MR. SCHULHOF If a case is uncrowded but within a millimeter of the borderline, the computer would take it out of the borderline classification and call it nonextraction. Now, if the patient were out at + 6mm lower incisor to APo with a perfect lower arch, then we have to think. If the lips are flaccid, that might be tolerable. If there is lip strain, that is another matter. We must take several norms into account in making a decision. We would use Holdaway's norms to evaluate the lip balance and Ricketts' esthetic plane to evaluate esthetics The computer will consider lip strain, esthetics and the +6mm in making the decision.
JCO Deciding among esthetics, function and stability calls for some individual decisions.MR. SCHULHOF Yes, and we weight them according to the instructions of the orthodontist. Many feel that they should be equally balanced in reaching a conclusion, but others may have strong preferences for one over the other. Each orthodontist registers his value judgments with us on a scale of 0 to 5 and the computer takes these into consideration.
JCO I don't think most of us realize that you are considering all of these individual factors. But, we still have problems with the norm concept.
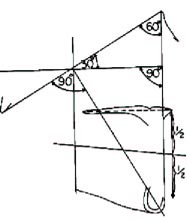
MR. SCHULHOF Well, Nature's way seems to be to determine a basic design from which we all vary a little. What occurs most often is really what Nature intended, and the other people are abnormal or at least unusual. I am struck by the balance and design inherent in the face as represented by our cephalometric references. For instance, at maturity the facial plane comes out perpendicular to the Frankfort plane. If you draw a line from Nasion to Point A, this is also perpendicular. The palatal plane is almost parallel, within one degree of the Frankfort plane. The average facial axis is 90º from the Basion-Nasion plane, which makes a 30º angle with the Frankfort plane, creating a 30-60-90 right triangle. The lower incisor comes out slightly ahead of the APo plane, which is merely a line connecting the anterior limits of the upper and lower jaws. The occlusal plane falls midway between the upper and lower jaws. We see a tremendous amount of logic and balance in Nature's design (Fig. 6).
JCO There are two problems with these thoughts. One is that we are a very heterogeneous genetic mixture and the other is that everybody's idea of beauty is different. Have you found that one average fits better with another average than one extreme might fit with a compensated extreme?
MR. SCHULHOF That's the difference between a descriptive norm--"The patient has a big jaw"--and a functional norm which describes the relationship between the jaws (Figs. 7 and 8).
If you have a large mandible compensated for by a protrusive maxilla, your convexity or ANB will be close to normal. If you have protrusive jaws and the lower incisor has been compensated by moving with the jaws, then you have an adequately compensated function. If you have a large nose, but the teeth are positioned forward to blend with this nose, you have a compensated situation. Sometimes you will have a patient with a retrognathic chin which makes him convex. We would not want to move his maxilla back as far as for a patient with a normal chin.
JCO You mentioned a normal maxilla versus an abnormal mandible. Are you confident from what you have built into the computer that you can tell which one is which?
MR. SCHULHOF Yes.
JCO There are still arguments as to what normal is.
MR. SCHULHOF The arguments are mostly concentrated on how you measure and what you use for a reference frame. Do you use SN or Frankfort plane? We prefer to use the Frankfort plane and I have some statistical evidence for that which we are publishing. The Frankfort plane is less variable from individual to individual if you use the actual porion and not the earrod. In addition, the outside world visualizes the patient from his Frankfort plane since that is how he generally holds his head.
With a good x-ray, Frankfort plane can be traced as accurately as SN.
There are very few arguments of more than a millimeter as to what normal is, once you have decided how you will measure it. This is purely a statistical survey of the literature, which we are continuing to update and hope to publish next year. It will be about one hundred pages long. It shows more agreement than disagreement, provided you define the sample well enough to individualize the norm for that patient.
JCO You mean with regard to age, sex, and racial group?
MR. SCHULHOF Yes, you need a different norm for each age, sex and racial group. Also, if a doctor wants a slightly more protrusive incisor or a flatter profile, this can be varied for his programin the computer.
It is interesting that there is considerable agreement on norms. In the six years we have been in business, we have not had an objection to our norms. There are arguments about whether we can predict, but not about our norms.
JCO What different racial groups do you recognize as requiring different norms?
MR. SCHULHOF We have different norms for Blacks, Chinese, Japanese, and Mexicans.
JCO How about different groups within the Caucasian population?
MR. SCHULHOF We haven't found that necessary. Our functional norms of lower incisor to APo and convexity, as well as esthetics, seem to hold for different groups of Caucasians. The Foundation for Orthodontic Research recently completed a study on a pure Italian sample as representative of the Mediterranean group of facial types and did not find that they differed from the norms we are now using for other normal occlusions. We find in certain groups such as the Mediterraneans, that there is a tendency toward an overdeveloped maxilla, but these people with an overdeveloped maxilla are also Class II.
JCO How do you determine what race a person belongs to? There is a considerable mixture in our population.
MR. SCHULHOF If the doctor claims the patient is Caucasian, we will use the Caucasian norms. However, if the doctor claims the patient is Mexican, we will compare the Mexican norms and the Caucasian norms to see which one he fits better. For Blacks, we have a complete Black to half-Black set of norms.
JCO What measurements define the racial differences?
MR. SCHULHOF Lip protrusion, convexity, lower incisor to APo, and anterior cranial base length vs width. The non-Caucasian populations have the same cranial size. It is just that they are shorter from the lateral and wider from the frontal.
JCO In combining growth and norms to produce a treatment objective, where do you start?
MR. SCHULHOF We start with the patient himself. There is certain key clinical information in a diagnosis that is not present in the models or the head film. This includes health of the gingiva, an evaluation of musculature, and an evaluation of excessively decayed teeth that might be prime candidates for extraction.
JCO How does this information get into your computer?
MR. SCHULHOF In the average patient, there would be a standard set of cephalometric limitations provided by the doctor and stored in the computer. However, if the clinical examination reveals problems such as gingival stripping, or excessively tight lips which might limit tooth movement, this information is entered by the doctor on his order form. For example, the doctor can tell us: maximum lower incisor forward movement--2mm; maximum expansion of molars--2mm, maximum lower molar distal movement--1mm; and so forth.
A lower incisor cephalometrically may be 5mm displaced, but if the doctor indicated beforehand that, because of the lip musculature and health of the gingiva, his maximum forward movement would be 3mm, then we must respect that. In this way, the doctor sets the limitations that he is willing to accept for this patient clinically, and it is up to the computer to find the optimum solution within those boundaries.
Our next step is an arch length shortage and mixed dentition analysis.
JCO Does the doctor send you models for this?
MR. SCHULHOF No. We don't need them. All that we require is a one-to-one occlusal view of the lower. This can be supplied using one of our special wax plastic-enclosed impression trays, a mandibular occlusal x-ray, a one-to-one photograph of the models, a Xerox of the models, or a one-to-one intraoral photograph.
JCO Which is best?
MR. SCHULHOF The best method is the one-to-one photograph with Unitek's Orthoscan II intraoral camera. This gives the doctor his record immediately, without waiting for the models to come back. The wax impressions are excellent provided that they are taken carefully, but there is a chance for a poor record. The mandibular occlusal x-ray is ideal except that it increases the patient'sradiation dose. The photograph of the model is good, except that you have to wait for the models to be made.
JCO What do you do with the lower occlusal image?
MR. SCHULHOF Our technicians trace it and locate the mesial and distal points of each tooth (Fig. 9).
These points are then digitized electronically, which just means that they go directly into the computer. The tooth mass is then calculated by adding the mesial and distal widths, and the space available is calculated by the computer which fits a mathematical curve to the center of the most forward lower incisor, the distal contact of the cuspids, and the distal point along the central fossa of the first molars.
JCO Was this based upon Brader's work?
MR. SCHULHOF I have been in close contact with Dr. Brader for many years and his concept of quantification of arch form has been a major stimulus to me. However, his forms are used for fitting the outside of the arch in order to construct an archwire. We were interested in the curve connecting the contact points, which is really a different problem, and we didn't find Brader's elliptical curves to be the most convenient for our purpose to fit a wide variety of naturally growing arches.
JCO What curve do you use?
MR. SCHULHOF It is a modified catenary curve which was first suggested by Dr. Jim Ackerman. In fact, he was the major stimulus for getting us into the procedure of coordinating cephalometrics with the lower arch. If you will imagine putting two poles in the wall and suspending a chain from the poles, the physical shape of the hanging chain will be a catenary. The modification that I made to the formula is unique in that it will fit any lower incisor, distal points of the cuspids and molars for any normal occlusion, and will also fit a tremendous variety of malocclusions. This is used to get a precise evaluation of space available.
JCO In the mixed dentition analysis, do you use a panorex or a full mouth series?
MR. SCHULHOF Either one. The size of the permanent tooth and the corresponding deciduous tooth is recorded with calipers and marked directly onto a form which is then digitized into the computer. The leeway space can be calculated by comparing the size of the deciduous teeth with the permanent teeth that will be replacing them.
JCO How do you correct for distortion and enlargement?
MR. SCHULHOF Since the computer knows the size of the deciduous tooth from the one-to-one occlusal record of the lower arch, it can compare the known value with the apparent size on the x-ray. The calculated enlargement can then be applied to correct the estimate of the permanent bicuspid or cuspid.
JCO Is this greatly more accurate than what the doctor can do himself?
MR. SCHULHOF Not if he were willing to go through all the steps that we do. Usually the doctor doesn't have the time to measure each tooth, estimate the tooth size, and bend a wire to the shape of the lower arch, and compare these measurements. Usually, he takes shortcuts by eyeballing the imbrication.
The arch length analysis has caused our telephone to ring quite often, because of the difference between eyeball estimates and the exact calculation. There is a tremendous optical illusion involved, and we find cases that appear to have 3-4mm of crowding by eye, but when we arrange the teeth one at a time along the computer arch, we may find that they all fit and there is no deficiency.
Many orthodontists will use a rule of thumb that there are 3mm of leeway space without going through the measurements of the particular teeth involved. For example, if the E is the only deciduous tooth remaining, there may be 3mm difference on each side between deciduous and permanent teeth for a total of 6mm.
JCO Do you always assume that the clinician's mechanics can hold all of the leeway space?
MR. SCHULHOF No. We can get an estimate from each doctor of what percentage of the leeway space he would assume is useful to him. In addition, we vary the amount of leeway space that can be held according to the facial pattern.
JCO You mean the more vertical the pattern, the less you assume can be held?
MR. SCHULHOF That's correct. Most clinicians find that the brachyfacial pattern, which is characterized by a flat mandibular plane, short lower face height and wide square jaws, has more biologic anchorage than a vertical pattern with a high mandibular plane and a long lower face.
JCO What is your starting point in making your analysis?
MR. SCHULHOF We begin in diagnosis with the lower incisor.
JCO Do you use APo plane?
MR. SCHULHOF Yes, and this is where the growth prediction comes in. If you are interested in treating to the APo plane, you have to estimate where A and Po are going to be at the end of treatment. Point A can be influenced by headgear and even heavy elastics, while Po will have its own growth vector and be influenced by tooth movements.
JCO You mean eruption of molars?
MR. SCHULHOF Yes.
JCO Is mandibular rotation predictable?
MR. SCHULHOF Nothing is perfectly predictable, but once again we make the best estimate we can with the information available. The odds change greatly with facial pattern, amount of Class II correction, and amount of orthopedics required in the maxilla. Also, whether the objective of the mechanics will be to open or close the bite. Since this is a function of high pull or cervical headgear, headgear must be determined before anything else. The amount and type of headgear used will determine the position of Point A and also influence the position of Po. Therefore, along with growth, headgear will determine the final APo plane. If you are using APo plane, you can't discuss tooth position until you know where A and Po are going to be.
JCO The computer decides on the headgear?
MR. SCHULHOF First of all, it looks ahead, based on the individual facial pattern to see how much profile may be expected to flatten without treatment. After we know how much a profile will flatten by itself, we know how much would be desirable to flatten it further with headgear. Then we determine how much it is possible to retract Point A in this person as a function of age, sex, race, and molar relation; and we check again to make sure that we are not treating a normal maxilla to an abnormal mandible, in which case a compromise would be necessary.
JCO How about direction of pull?
MR. SCHULHOF Based upon the shape of the mandible, lower face height, facial axis, palatal plane and tooth movement required, we determine how strong we would lean to high pull or cervical headgear.
JCO Can the doctor influence your decision on this?
MR. SCHULHOF Yes. He can tell us if he uses cervical headgear in the majority of cases and high pull in only severe vertical patterns, or whether he uses high pull in most cases and cervical in only very deep bite patterns, or anywhere in between.
Since we know the pattern and we have his instructions matching his choice of headgear to patterns, we can then make a reasonable decision.
JCO Is it really necessary to make several measurements and a growth prediction just to decide what headgear to use?
MR. SCHULHOF In about 70% of the cases the doctor would reach the same conclusion just by looking at ANB and the mandibular plane. Users of our service have told us that in about 30% of the cases, they are quite surprised at our recommendation, but after reviewing the data more carefully, they agree with us. I think we have prevented overuse of headgear in a large number of cases.
JCO You just said that if you use APo plane, you can't discuss tooth position until you know where A and Po are going to be. You do use APo as a guide and you do, therefore, have to predict A and Po.
MR. SCHULHOF Yes. We calculate the normal growth during treatment and then build the effects of treatment into it to predict A and Po. Once we have the APo plane, we next predict the occlusal plane before we begin to set teeth.
JCO Which occlusal plane do you use?
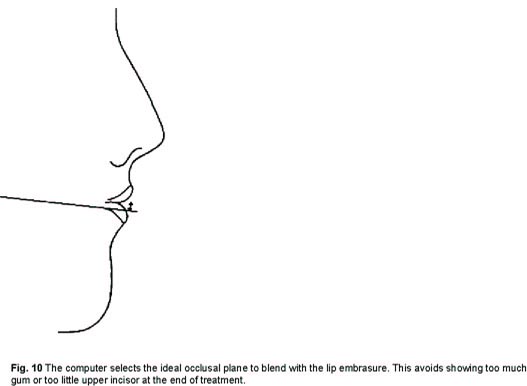
MR. SCHULHOF Ricketts uses the occlusal plane defined by the bicuspids and molars, not the incisors. We determine where it should be to give the most attractive smile line. If the occlusal plane is too low compared to the embrasure of the lips, you see too much gum. If it's too high, you don't see the upper incisors at all (Fig. 10).
JCO Now, once you have established the APo plane and the occlusal plane you are ready to position teeth, starting with the lower incisors?
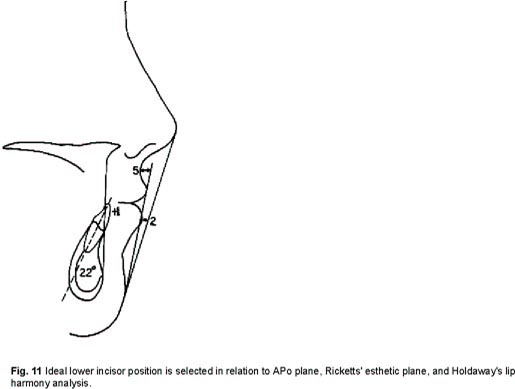
MR. SCHULHOF That's right. We use an ideal of +1mm for the lower incisors to the APo plane, which we consider to be a functional ideal. We have a second ideal which is a 22º angulation of lower incisor to APo, which many clinicians believe to be associated with stability, although we have never proven it.
We also determine the ideal position based upon Ricketts' esthetic plane and a separate determination using Holdaway's line which attempts to get an ideal lip contour free of constraint (Fig. 11).
JCO Do these analyses often conflict?
MR. SCHULHOF In the majority of cases they will come up with the same position, but when they do conflict we take into account the wishes of the individual clinician. Among the weighting factors he has given us previously, he has told us which of these analyses he considers to be the most important.
In this way, we arrive at the ideal position of the lower incisor, and the computer then prints out how many millimeters of labial or lingual movement would be required to achieve the ideal position. Next we tackle arch form.
Our catenary curve needs the ideal position of the incisors, cuspids and molars to arrive at the ideal arch form. The position of the incisors has been determined. The molar width is based on the frontal analysis and facial pattern. We find that wide, square jaws can accommodate wider molars, as you would expect.
For the cuspid, we find that jaw variability is a lot greater than intercuspid width variability. We calculate the ideal width at the distal of the cuspids as a function of tooth size and facial pattern. So far, cuspid width seems to be more of a tooth determined factor than jaw determined, although there is a correlation between the squareness of the jaw and intercuspid width.
JCO Is there any validity that you have established for the idea of extracting bicuspids and moving cuspids back into a wider area of the arch?
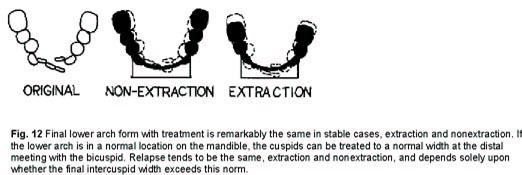
MR. SCHULHOF Our most recent research on treated cases shows that from cuspid to cuspid you get approximately the same arch form in extraction or nonextraction (Fig. 12).
This often calls for a gain in arch length from the distal of one cuspid to the distal of the other. If this had been included in the original calculation on such cases, you might say that extraction was not necessary in the first place.
JCO Which might suggest extracting a lower incisor at times.
MR. SCHULHOF It might depend on whether the lower arch would be abnormal in relation to APo. We haven't studied enough of those cases. We do know that there is a low correlation of cuspid width to jaw shape and a higher correlation with tooth size. Somehow, doctors seem to feel safer extracting first bicuspids and expanding cuspids to get them to fit with second bicuspids. Our data shows that the cuspids reached their ideal width and have the same rate of relapse when they are overexpanded, whether you extracted in back of them or not. If the lower arch is in a normal place on the mandible, the cuspids should attain a normal width at the distal meeting of the bicuspid.
JCO This might be more of a function of bicuspid expansion than cuspid expansion in most cases.
MR. SCHULHOF Yes. The key is that we are discussing the distal contact of the canines. Don Gardner's thesis at UCLA showed that the first bicuspids were the most consistently expanded, that molar relapse was minimal and that the majority of cases showed significant intercuspid width relapse.
The research was carried one step further in Randy Schuller's thesis at Loma Linda which divided the cases into those that relapsed and those that didn't. Ninety percent of the cases which were expanded 2mm or more in the cuspids but which were not expanded past the norm, showed negligible relapse. The cases which relaped were expanded past the norm. Thus, it agreed with previous data, but it carried it one step further.
JCO At this point, the computer has calculated ideal incisor position, the effect of treating to an ideal arch form with its implications about various widths, and it has calculated arch length shortage, if any. In the event of inadequate space, does it offer a specific solution in each case?
MR. SCHULHOF The computer would determine a compromise, including the possibility that it might allow up to one standard deviation forward of ideal for the lower incisor.
JCO What would this depend on?
MR. SCHULHOF The wishes of the doctor for one thing, and facial pattern.
JCO Is there agreement on facial patterns?
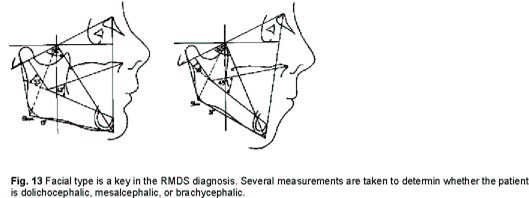
MR. SCHULHOF Some people may prefer one measurement more than another. We combined several measurements and I think most people would agree with our facial typing (Fig. 13).
The clinical findings with Ricketts' cases show that a brachyfacial pattern can accept a more forward lower incisor position, probably due to the interaction between growth and lip function. The dolichofacial pattern has a mandible rotating downward, which rolls the teeth into the lips inviting relapse. Bjork also has shown that, with growth, the brachyfacial pattern gives you more space, whereas the dolichofacial gives you less space. In addition, most clinicians would agree that a brachyfacial pattern gives you a better natural anchorage. This means that if you extract in such a case, you stand a risk of moving the lower incisor too far lingually because the lower molar doesn't want to come forward .
If a compromise is needed, we usually give the brachycephalic pattern the benefit of the doubt before we extract, and in the dolichocephalic we would have a predisposition for extraction .
JCO Does the computer ever consider distal movement of the lower molars?
MR. SCHULHOF We can calculate cephalometrically whether the lower molar is positioned normally, or is mesial or distal of normal. If it is mesial, distalization is a consideration. Another factor is that, on the order form, the doctor gives us his maximum for lower molar distal movement.
After we have positioned the molars, we have a calculation of the maximum space available in this arch considering esthetics, function and stability. If there is space for the teeth within these constraints, this is a nonextraction case in the lower arch. If there is insufficient space, it is an extraction case.
The upper arch is next. Once we have positioned the lower molar and considered growth, we can determine how far the upper molar needs to be moved distally. The doctor can give us a maximum that he would be willing to move upper molars distally in this patient, including considerations of age and cooperation potential. We then check the required upper molar distal movement against the clinical maximum the doctor has set.
JCO if excessive upper molar distal movement is required, does the computer make a choice between first bicuspid, second bicuspid, or second molar extraction?
MR. SCHULHOF That is really a clinical decision. We will only print the fact that extraction is required. The rest would be left to the doctor.
JCO So, the computer derives the ideal positions for the teeth. Does it then print them out in words and as a diagram?
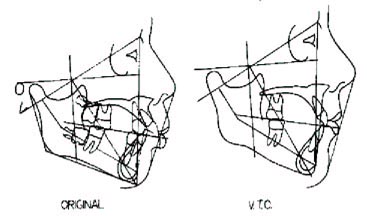
MR. SCHULHOF Before the information can be put into this Visualized Treatment Objective, it is necessary to interpret the growth prediction using superpositions (Fig. 14 and 15).
JCO That was the essence of Dr. Ricketts' article in the April 1975 JCO.
MR. SCHULHOF That's right.
JCO Is there agreement on what are the best points of superposition?
MR. SCHULHOF Not really, but if you refer to Ricketts' article, his positions were found to be statistically significant. The first superposition is Basion-Nasion at the facial axis to show the doctor how much rotation he can expect during treatment. If he begins to exceed this, he has a warning to change his treatment mechanics, since the plan is based on no more than the specified amount of rotation.
We have found that the facial axis does not tend to change even over a 10-year period. The mandibular plane changes a degree every three years. So, if your treatment closed the mandibular plane, you would not be doing anything that normal growth could not have done. If it closed the facial axis, you can be sure that this was not a normal growth expectation and was an effect of treatment better than 90 % of the time.
The angle SNA or BaNA doesn't change more than a degree during the treatment period unless it is affected by treatment. Hence, our superposition 2 (at Nasion) shows the doctor the amount of reduction of Point A that is called for in the case. He may then compare progress tracings against this goal and have a better understanding of patient cooperation, as well as knowing when he should terminate orthopedic forces. When he has achieved the goal in terms of Point A movement, he should switch to lighter forces.
JCO To evaluate the eruption of teeth, Dr. Ricketts' Four Step Analysis uses corpus axis as a reference instead of mandibular plane, which most people have used. Why is that?
MR. SCHULHOF We think that corpus axis is more suitable because there is about 50% more variation using the mandibular plane and, without treatment, the incisors appear to erupt lingually if you use mandibular plane. This may be why many authors have claimed that moving the lower incisors forward results in post-treatment relapse. If you use the mandibular plane and consider settling after treatment due to band space, most cases will tend to show lingual movement post-treatment.
JCO Now from all of this you send the doctor treatment objectives and alternatives and diagrams of the Visualized Treatment Objective along with the four-position analysis which distinguishes between the effects of treatment and of natural growth. How does he use these?
MR. SCHULHOF He constructs his own treatment plan, based on this organized data, which has been individualized not only by the profile of the doctor's treatment parameters which we have in the computer, but also any constraints that the doctor may have wanted to place on this particular case. The doctor checks over our objectives and alternatives for the case, to see if he agrees with our recommendations and the logic by which they were derived.
JCO It seems to me that people who think of your service as growth prediction have really got the wrong idea.
MR. SCHULHOF Yes. Growth prediction is a minor portion of the value of our service.
JCO Are there some orthodontists who will benefit more from the computer service than others?
MR. SCHULHOF If a doctor places a value on treating a case nonextraction, he will have a far greater use for the computer than one who extracts in 80% of his cases. The computer will tell you how to minimize the number of extractions in those cases where it can be done with a minimum risk of relapse. If a doctor has no interest in that, he would have a lesser interest in our service.
We have worked up a little over 40,000 cases now and have many doctors using the service for several years. We have feedback from all of these users on the cases we have processed for them and we have evolved a service which can fit a great number of orthodontic practices.
JCO I want to think you, Bob, for clarifying computerized cephalometric analysis for us.