Adult Orthodontics
In the last few years there has been considerable interest in orthodontic treatment for the adult patient. A recent survey conducted by the AAO showed an increase in the percentage of patients over 21 years of age from a fraction more than 4% ten years ago to almost 7% today. Nearly 11% is expected after another decade.
Since an adult is defined as one who is fully grown, most males of 18 or 19 and most females of 16 can be considered as adults. The percentage of adult patients would therefore be somewhat higher than the figures shown above. Over the past ten years in my own practice, 10% to 15 % of the patients have been adults.
Dr. Irving Glickman, the eminent periodontist, has often pointed out the need for orthodontic treatment for adult patients. As long as fifteen years ago, he made a strong plea to orthodontists attending the annual AAO meeting to accept adult patients on a routine basis.
What are the differences between adult and child orthodontics? The basic difference is that in children we must concern ourselves with tooth movement plus growth, whereas in adults we are dealing strictly with tooth movement. We cannot count upon growth to help us (or hinder us) in achieving our treatment objectives. In a way, then, adult orthodontics is simpler, for we have one less (and often unpredictable) factor with which to contend. There are, however, several other differences between adult and child orthodontics (Table I) .
Motivation
Why do adults seek orthodontic treatment? Based on my own practice experiences, I would list some of the reasons as follows:
The recent periodontal awareness of the dental profession has indirectly affected the orthodontic specialty in that orthodontic treatment has now become an integral part of the total treatment plan concept. Therefore, close co-operation of the orthodontist with the periodontist and restorative dentist is essential for proper treatment of the adult patient.
Procedure
The usual sequence of procedure in adult patients is as follows:
Occlusal adjustments ( grinding) should be performed when ever necessary during all of the above stages.
It should be pointed out that orthodontic treatment, whether it be for the adult or the child patient, is actually a type of mouth rehabilitation. When performed on the adult patient in conjunction with the restorative dentist, the orthodontic treatment is one aspect of the total oral rehabilitation for that patient. In some instances no restorative work is required following orthodontic treatment. Thus the total oral rehabilitation can be carried out orthodontically. In other instances the rehabilitation can be carried out solely by the prosthodontist (or restorative dentist) through the use of inlays, on-lays, crowns, bridges, splints, etc. Thus if the term "full mouth rehabilitation" applies to the prosthetic restoration of a mouth to proper health and function, it should apply equally to the orthodontic
restoration of a mouth.
Classification
Since many of our adult patients require both orthodontic and prosthetic services, a classification has been devised to facilitate the treatment planning of adult patients (Table II) .
CASES
The following cases will serve as examples of the classification and illustrate the wide scope of adult orthodontic treatment.
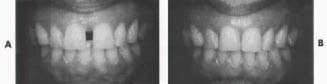
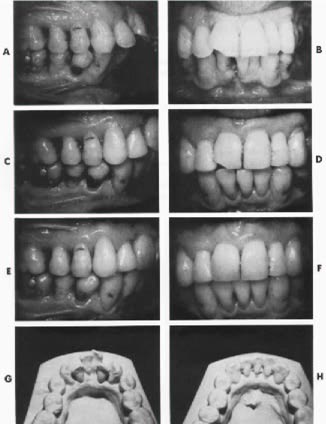
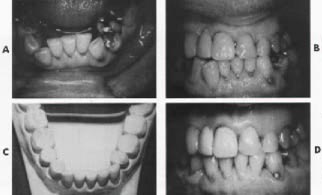
Case 1 (Fig. 1) Mrs. P. S. Age 39
CLASS A 1 (Minor orthodontics; orthodontic retention). Treatment time-- 7 months. Reason for treatment-- Wide diastema between upper centrals which was becoming a major concern to the patient.
Orthodontic treatment--
Maxillary-- removable (high labial type). Mandibular-- none.
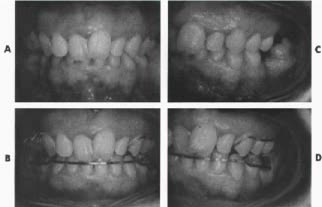
Case 2 (Fig. 2) Mr.E.F Age 37
CLASS B 3 (Minor orthodontic, prosthetic restoration; fixed splinting). Treatment time-- 5 months. Reason for treatment-- Dentist recommended orthodontic treatment for correction of crossbite prior to commencing prosthetic rehabilitation.
Orthodontic treatment--
Maxillary-- removable with pontics replacing upper centrals and upper left lateral. Mandibular-- removable with pontics replacing four lower incisors and posterior bite plane to disarticulate teeth in crossbite.
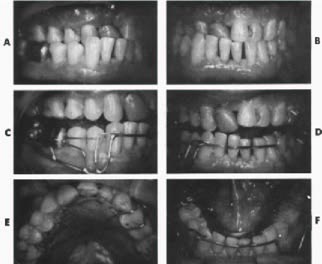
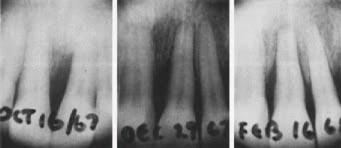
Case 3 (Figs. 3 and 4) Mr. P. S. Age 38
CLASS C 1 + 2 (Major orthodontics; orthodontic retention (maxilla), temporary splinting
(mandible). Treatment time-- 22 months Reason for treatment-- Advice of periodontist. Severe lower anterior crowding contributing
greatly to periodontal problem. Prognosis on four lower incisors uncertain. Better positioning of lower 3s advisable for future bridgework if lower incisors were to be lost.
Orthodontic treatment--
Maxillary-- removable (high labial type). Mandibular-- fixed bands.
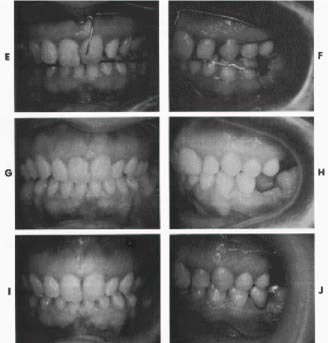
Case 4 (Fig. 5) Miss H. N. Age 30
CLASS D 1 + 2 + 3 (Major orthodontics, prosthetic restoration; orthodontic retention and temporary splinting (maxilla), fixed splinting (mandible) . Treatment time-- 24 months. Reasons for treatment-- Patient concerned with overlapping upper central incisors. Dentist advised orthodontics for better tooth positioning prior to prosthetic restoration
Orthodontic treatment--
Maxillary-- removable (with anterior bite plane). Mandibular-- removable (with posterior bite plane).
Case 5 (Fig. 6) Mrs. M. C. Age 38
CLASS B 1 + 3 (Minor orthodontics, prosthetic restoration; orthodontic retention, fixed splinting).
Treatment time-- 8 months. Reason for treatment-- Severe posterior crossbite on the right side causing difficulties in mastication.
Orthodontic treatment--
Maxillary-- removable. Mandibular-- removable.
Case 6 (Fig. 7)Mr. H. H.Age 49
CLASS C 1 (Major orthodontics; orthodontic retention) Treatment time-- 15 months.Reason for treatment-- Patient was advised by his dentist to have his anterior occlusion corrected orthodontically. Traumatic occlusion was causing occasional small fractures of maxillary incisors.
Orthodontic treatment--
Maxillary-- none. Mandibular-- fixed bands.
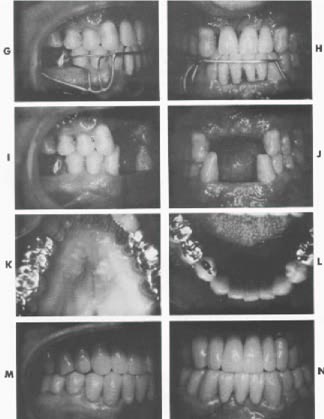
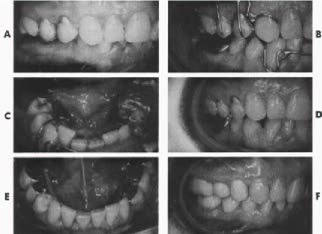
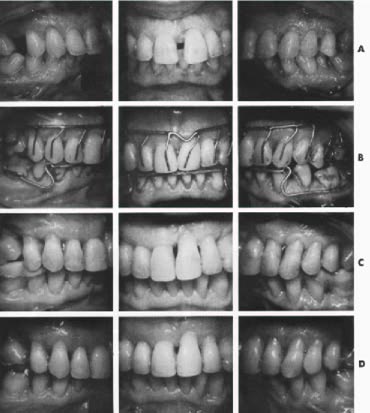
Case 7 (Figs. 8 and 9)Mr. W. F.Age 45
CLASS D 2 + 3 (Major orthodontics, prosthetic restoration; temporary splinting (anteriors), permanent splinting (posteriors) .Treatment time-- 17 months. Reason for treatment-- Recommended by dentist and periodontist for better tooth placement prior to prosthetic rehabilitation. Also for closure of diastema between upper centrals.
Orthodontic treatment--
Maxillary-- removable (high labial type). Mandibular-- removable (Hawley type) . Occupation of patient precluded use of fixed bands.
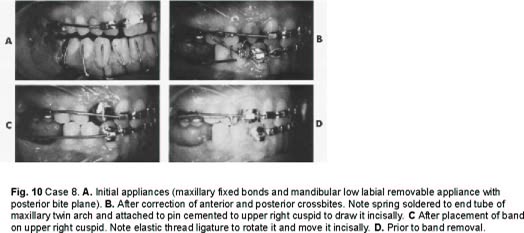
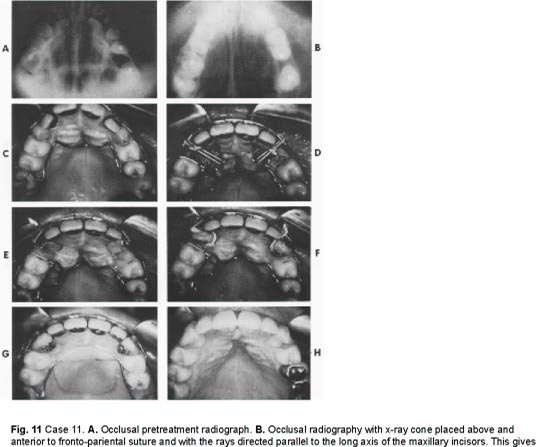
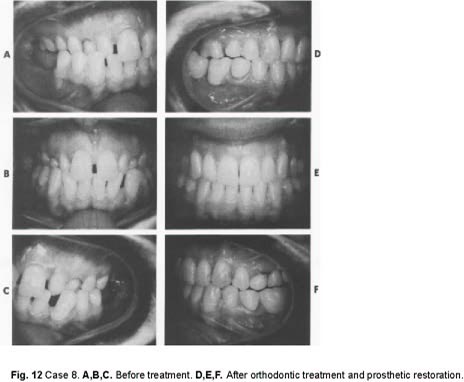
Case 8 (Figs. 10, 11, and 12) Miss D. L. Age 26
CLASS D 1 + 3 (Major orthodontics, prosthetic restoration; orthodontic retention, fixed splinting). Treatment time-- 33 months. Reason for treatment-- Patient concerned with the appearance of her teeth and the health of her mouth. She came from a small town where no orthodontic treatment was available. She now has an important position and wishes to do whatever is possible to improve herself. Orthodontic treatment--
Maxillary-- fixed bands. Mandibular-- first removable, then fixed bands.
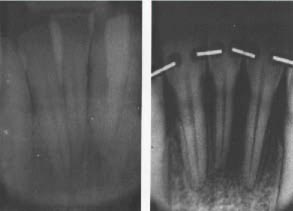
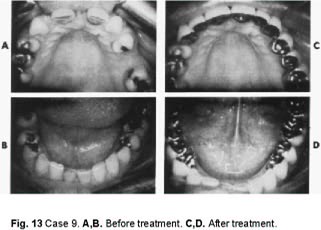
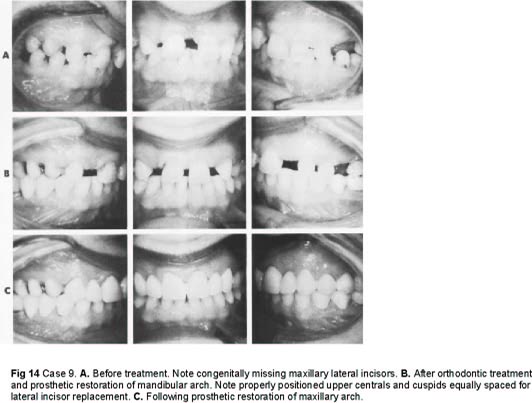
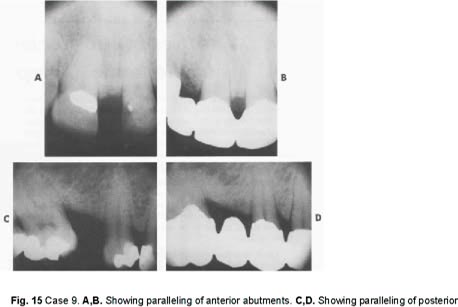
Case 9 (Figs. 13), 14) and 15) Mrs. M. L. Age 38
CLASS D 3 (Major orthodontics, prosthetic restoration; fixed splinting). Treatment time-- 17 months.Reason for treatment-- Patient was extremely self-conscious about the appearance of the anterior teeth, especially the upper central diastema which was due primarily to congenitally missing laterals. Upon accepting positions of responsibility in community organizations, she felt something had to be done about her teeth. Her dentist felt that proper results could not be achieved by bridgework alone.
Orthodontic treatment--
Maxillary-- fixed bands.
Mandibular-- removable.
Conclusion
There is a great need for orthdontic treatment for the adult patient. Continuing education of the general public will result in an increasing demand for this type of service. The orthodontist should update his knowledge and his thinking in this aspect of his responsibility, and should try as much as possible to co-ordinate his efforts with those of his confreres in other branches of dentistry in order to render to the population a better and more complete dental health service.