Invisalign with Photobiomodulation: Optimizing Tooth Movement and Treatment Efficacy with a Novel Self-Assessment Algorithm
Because of its esthetics and convenience, Invisalign* is a popular option for orthodontic treatment, particularly among adults. Until recently, Align Technology has recommended that a new aligner be worn every two weeks; more frequent changes were believed to result in a loss of aligner tracking and potential treatment delays.1,2
In any case, patients in today’s immediate gratification society want and expect things faster than ever before—including orthodontic treatment. Given the inverse relationship between treatment time and compliance, it would be mutually beneficial to offer a safe and effective means of reducing treatment time while maintaining the high-quality results that we seek for our patients.
Methods developed to accelerate treatment include corticotomy,3 vibrational technology,4,5 and laser and light-emitting diode (LED) photobiomodulation (PBM).6 PBM is of particular interest because it is noninvasive and its mechanisms of action are well known, targeting the mitochondria by means of photochemical effects to promote bone remodeling.7,8 Additionally, it has been shown to accelerate a variety of orthodontic therapies, including both fixed appliances9,10 and Invisalign. Published case studies of Invisalign treatment with supplemental PBM have demonstrated that patients can change aligners more rapidly than under the standard Invisalign protocol, thereby reducing treatment time.11,12
Similar articles from the archive:
Like other means of orthodontic treatment, aligners move teeth through the application of compressive and tensile forces to the periodontium.13 Optimal orthodontic tooth movement occurs when light and continuous forces are applied and maintained. The initial forces applied by an aligner diminish and level off, however, as the teeth move.14 The longer the aligners are worn, the more the force will decline.15,16 There is also some variability among individual patients in terms of the speed of tooth movement; some are fast movers, while others are slower.17 To optimize the rate of aligner progression, a patient should be able to transition into subsequent aligners at a frequency that reflects his or her own rate of tooth movement. A new method of self-assessment, as described in this article, was designed to allow such individualized aligner changes, in conjunction with accelerated treatment using PBM.
Materials and Methods
Two patients participated in clinical trials aimed at maximizing the continuity of orthodontic forces with aligners by customizing aligner-change rates, based on a self-assessment algorithm. One patient had aligners prescribed for the conventional 14-day wear, the other for weekly changes. Each patient was instructed to use a daily questionnaire, with aligner pressure rated on a three-point scale. When the score reached 1 (lowest pressure), the patient was told to switch to the subsequent aligner. The orthodontist monitored aligner tracking and progression throughout treatment.
Invisalign’s Best Practice Protocol (BPP) includes the maximum amount of a given type of movement from one aligner to the next. With 14- day changes, these movements may be set to as much as 2˚ of tipping, 1˚ of torque, and 2˚ of rotation per aligner. BPP was used for both patients, with no alteration of movement rates.
OrthoPulse** is a PBM device, approved by the U.S. Food and Drug Administration, that uses continuous 850nm-wavelength light to safely accelerate tooth movement (Fig. 1).

Fig. 1 OrthoPulse** device.
It is wireless, made of medical-grade silicone, and embedded with flex circuit arrays of LEDs. OrthoPulse has been shown to accelerate a variety of tooth movements, including leveling and alignment and space closure, by as much as 2.3 times in animals and humans.9,15 The concept of combining OrthoPulse treatment with aligners is intended to maintain light, continuous forces while facilitating faster treatment. In this study, the rate of aligner changes during daily OrthoPulse treatments was compared to the conventional Invisalign rate for each patient (Fig. 2).
Case 1
A 14-year-old male presented with a dislike of the triangular spaces between his upper central incisors. He demonstrated mild-to-moderate mandibular crowding with incisor supraeruption, a moderate deep bite, evidence of bruxism, and congenitally small upper lateral incisors (Fig. 3). He had a mildly retrusive maxilla and mandible and a short upper lip. After enameloplasty was performed, a course of Invisalign treatment involving biweekly aligner changes was prescribed.
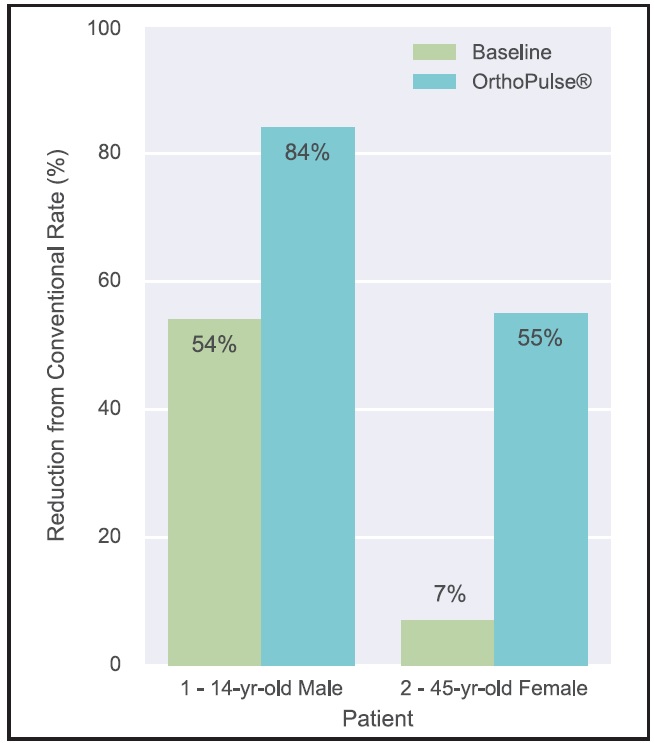
Fig. 2 Aligner-change rates with OrthoPulse compared to those for conventional Invisalign* treatment.
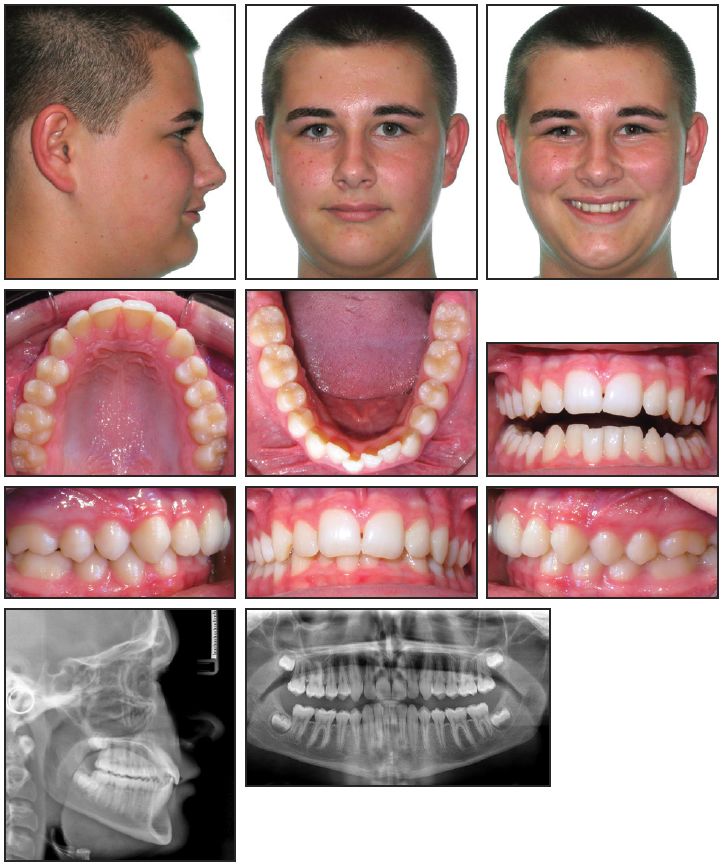
Fig. 3 Case 1. 14-year-old male patient with mandibular crowding and moderate deep bite before treatment.
The patient was instructed to wear the first two sets of aligners for 14 days each to familiarize himself with typical aligner pressure and fit. Thereafter, under the guidance of the orthodontist, he progressed to the next aligner when he scored 1 for aligner pressure on the daily questionnaire. A baseline rate of aligner change was established for the subsequent four sets of aligners. At that point, OrthoPulse treatment was introduced for five minutes per arch per day for another four sets of aligners. The patient continued to change aligners in accordance with the self-assessment algorithm. He was then instructed to progress through the remaining aligners at the same rate that was established during the OrthoPulse phase.
In the initial baseline period, this patient switched his aligners on average every 6.5 days. With daily OrthoPulse use, he changed aligners on average every 2.3 days—an 84% reduction from the conventional 14 days, and a 54% reduction from the patient’s own baseline. He was able to maintain tracking throughout treatment despite transitioning through aligners every 2.3 days during the OrthoPulse period and the remainder of treatment.
The patient required 26 aligners and an additional 19 refinement aligners. Based on the conventional 14-day change rate, he would have finished treatment in 90 weeks. Even though there were periods of time without OrthoPulse treatment due to the study protocol, he actually completed all aligners in 43 weeks (Fig. 4). He experienced no adverse events at any point during treatment.
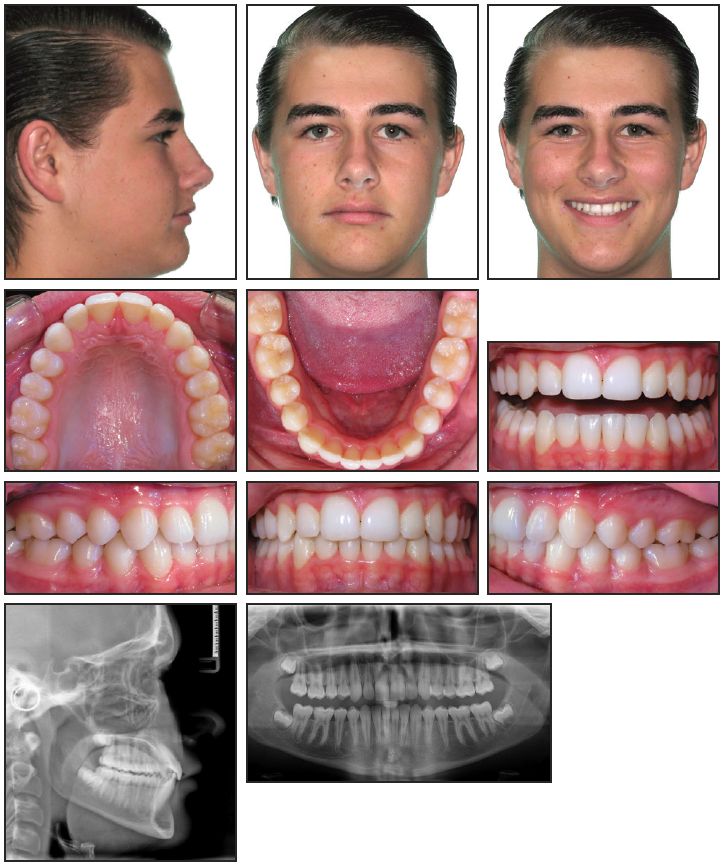
Fig. 4 Case 1. Patient after 43 weeks of treatment.
Case 2
A 45-year-old female was referred by her periodontist, who requested that her teeth be moved prior to gingival grafting. She presented with a skeletal open-bite tendency and normal bone levels (Fig. 5).

Fig. 5 Case 2. 45-year-old female patient with anterior crossbite and Class I molar and canine relationships before treatment.
Her archforms were significantly constricted, with palatally inclined teeth and moderate lower anterior crowding. She had a dental anterior crossbite and Class I molar and canine relationships. The treatment plan was to broaden the arches and move the teeth into position for gingival grafting. Treatment objectives also included aligning the teeth, alleviating the mandibular crowding, and improving the smile arc.
The patient was prescribed seven-day aligners, which are designed to achieve half the desired magnitude of tooth movement as with 14-day aligners, following the same Invisalign BPP. As in Case 1, the patient was instructed to change aligners when she reached a pressure score of 1 on the daily questionnaire.
This patient changed the seven-day aligners every 6.5 days when OrthoPulse was not used, for a 7% reduction in transition rate from the conventional pattern. She switched aligners every 3.2 days when OrthoPulse was used daily—a 55% reduction from conventional aligner changes. Although she was estimated to finish treatment in 62 weeks, based on the number of first-series aligners in her plan, she actually completed all aligners in 35 weeks. The patient was then prescribed 11 14-day refinement aligners, which under the normal protocol would have taken 22 weeks; she progressed through these aligners in four weeks, changing every 2.5 days. With daily OrthoPulse use throughout most of treatment, this patient completed active Invisalign treatment in 39 weeks, compared to the normally expected time of 84 weeks (Fig. 6).

Fig. 6 Case 2. Patient after 39 weeks of treatment.
The patient was ready to return to her periodontist for grafting procedures after nine months of active treatment, which was a significant advantage in expediting multidisciplinary care. Although the primary role of OrthoPulse in this study was to permit faster aligner changes, it may also have contributed to pain resolution, as seen with other PBM devices. The second patient reported feeling less sensitive to pressure and feeling less dental pain as soon as daily OrthoPulse use was introduced. Following the initial study period, we suggested that she increase her OrthoPulse treatments to twice daily, and she reported a further reduction in pain. She experienced no adverse events at any point during treatment.
Discussion
The two patients presented in this article demonstrate not only the variability among individuals in rates of tooth movement and optimal aligner changes, but the potential benefits of LED PBM administration in accelerating Invisalign treatment. By utilizing the new self-assessment algorithm, we can tailor our biomechanics to each patient’s unique biology.
When teeth have moved to their programmed positions, the aligner will no longer apply force, and the patient will perceive a low pressure.14,15,17 This is why aligner pressure as rated by the patient was used to determine the optimal rate of aligner change for that individual. Although an increase in pressure tolerance could have occurred, leading to premature aligner changes, each patient was instructed to remove and clean the aligners before placing them back in the mouth and rating the pressure. Furthermore, the orthodontist consistently monitored aligner tracking to prevent premature switching. Both patients maintained tracking throughout treatment, as demonstrated by their positive results.
In both cases, adjunctive OrthoPulse use allowed substantially faster aligner changes than under the conventional protocol. The efficacy of this PBM device was confirmed in previous studies by Shaughnessy and colleagues10 and Kau and colleagues.9 PBM devices using laser light sources have also been shown to be effective in accelerating tooth movement.18-20 Although the safety of faster aligner changes may be more of a concern, a previous study of accelerated orthodontic treatment with PBM found no increase in root resorption.21 Our two patients showed no adverse effects from PBM, and neither has experienced any orthodontic relapse.
FOOTNOTES
- *Registered trademark of Align Technology, Inc., Santa Clara, CA; www.aligntech.com.
- **Registered trademark of Biolux Research Ltd., Vancouver, BC, Canada; www.bioluxresearch.com.
REFERENCES
- 1. Boyd, R.L.: Increasing the predictability of quality results with Invisalign, Proc. Ill. Soc. Orthod., Oak Brook, IL, March 7, 2005, www.gpso.org/events/2003_outline.pdf, accessed Oct. 8, 2015.
- 2. Bollen, A.M.; Huang, G.; King, G.; Hujoel, P.; and Ma, T.: Activation time and material stiffness of sequential removable orthodontic appliances, Part 1: Ability to complete treatment, Am. J. Orthod. 124:496-501, 2003
- 3. Kim, S.J.; Park, Y.G.; and Kang, S.G.: Effects of corticision on paradental remodeling in orthodontic tooth movement, Angle Orthod. 79:284-291, 2009.
- 4. . Kau, C.H.: A radiographic analysis of tooth morphology following the use of a novel cyclical force device in orthodontics, Head Face Med. 7:14, 2011.
- 5. Woodhouse, N.R.; DiBiase, A.T.; Papageorgiou, S.N.; Johnson, N.; Slipper, C.; Grant, J.; Alsaleh, M.; and Cobourne, M.T.: Supplemental vibrational force does not reduce pain experience during initial alignment with fixed orthodontic appliances: A multicenter randomized clinical trial, Sci. Rep. 5, 2015.
- 6. Long, H.; Pyakurel, U.; Wang, Y.; Liao, L.; Zhou, Y.; and Lai, W.: Interventions for accelerating orthodontic tooth movement: A systematic review, Angle Orthod. 83:164-171, 2013.
- 7. Chung, H.; Dai, T.; Sharm, S.K.; Huang, Y.Y.; Carroll, J.D.; and Hamblin, M.R.: Nuts and bolts of low-level laser (light) therapy, Ann. Biomed. Eng. 40:516-533, 2012.
- 8. Prindeze, N.J.; Moffatt, L.T.; and Shupp, J.W.: Mechanisms of action for light therapy: A review of molecular interactions, Exp. Biol. Med. (Maywood) 237:1241-1248, 2012.
- 9. Kau, C.H.; Kantarci, A.; Shaughnessy, T.; Vachiramon, A.; Santiwong, P.; de la Fuente, A.; Skrenes, D.; Ma, D.; and Brawn, P.: Photobiomodulation accelerates orthodontic alignment in the early phase of treatment, Prog. Orthod. 14:30, 2013.
- 10. . Shaughnessy, T.; Kantarci, A.; Kau, C.H.; Skrenes, D.; and Ma, D.: Intraoral photobiomodulation-induced orthodontic tooth alignment: A preliminary study, BMC Oral Health 16:3, 2016.
- 11. Ojima, K.; Dan, C.; Kumagai, Y.; and Schupp, W.: Invisalign treatment accelerated by photobiomodulation, J. Clin. Orthod. 50:309-317, 2016.
- 12. Shaughnessy, T.G.: Long-distance orthodontic treatment with adjunctive light therapy, J. Clin. Orthod. 49:757-769, 2015.
- 13. Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; and Debernardi, C.L.: Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review, Angle Orthod. 85:881-889, 2015.
- 14. Simon, M.; Keilig, L.; Schwarze, J.; Jung, B.A.; and Bourauel, C.: Forces and moments generated by removable thermoplastic aligners: Incisor torque, premolar derotation, and molar distalization, Am. J. Orthod. 145:728-736, 2014.
- 15. Vardimon, A.D.; Robbins, D.; and Brosh, T.: In-vivo von Mises strains during Invisalign treatment, Am. J. Orthod. 138:399-409, 2010.
- 16. Alikhani, M.; Alyami, B.; Lee, I.S.; Almoammar, S.; Vongthongleur, T.; Alikhani, M.; Alansari, S.; Sangsuwon, C.; Chou, M.Y.; Khoo, E.; Boskey, A.; and Teixeira, C.C.: Saturation of the biological response to orthodontic forces and its effect on the rate of tooth movement, Orthod. Craniofac. Res. 18:8-17, 2015.
- 17. Tanne, K.; Sakuda, M.; and Burstone, C.J.: Threedimensional finite element analysis for stress in the periodontal tissue by orthodontic forces, Am. J. Orthod. 92:499-505, 1987.
- 18. Maheshwari, S.; Verma, S.K.; Tariq, M.; and Gaur, A.: Rapid orthodontics: A critical review, Univ. J. Dent. Sci. 1:35-38, 2015.
- 19. Cruz, D.R.; Kohara, E.K.; Ribeiro, M.S.; and Wetter, N.U.: Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: A preliminary study, Lasers Surg. Med. 35:117-120, 2004.
- 20. Genc, G.; Kocadereli, I.; Tasar, F.; Kilinic, K.; El, S.; and Sarkarati, B.: Effect of low-level laser therapy (LLLT) on orthodontic tooth movement, Lasers Med. Sci. 28:41-47, 2013.
- 21. . Nimeri, G.; Kau, C.H.; Corona, R.; and Shelly, J.: The effect of photobiomodulation on root resorption during orthodontic treatment, Clin. Cosmet. Investig. Dent. 15:1-8, 2014.



